Supplemental Table 2. Design and findings of eligible studies Study
advertisement
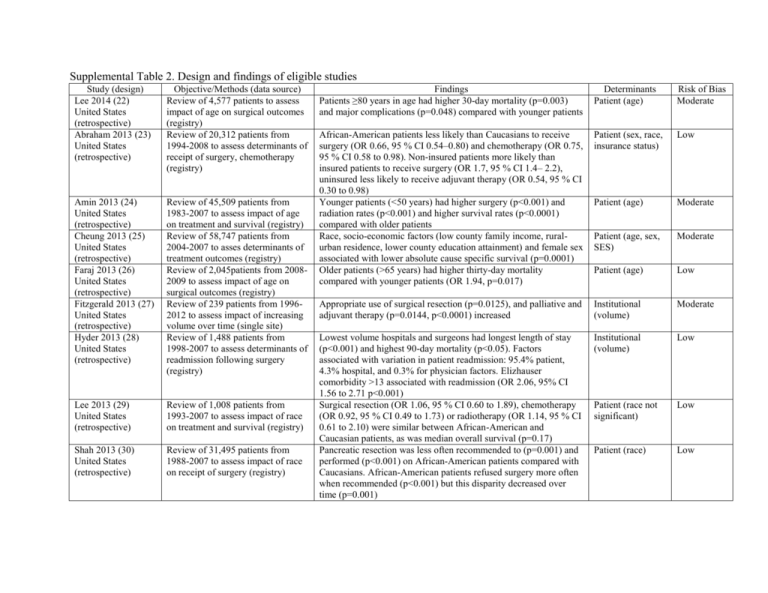
Supplemental Table 2. Design and findings of eligible studies Study (design) Lee 2014 (22) United States (retrospective) Abraham 2013 (23) United States (retrospective) Objective/Methods (data source) Review of 4,577 patients to assess impact of age on surgical outcomes (registry) Review of 20,312 patients from 1994-2008 to assess determinants of receipt of surgery, chemotherapy (registry) Amin 2013 (24) United States (retrospective) Cheung 2013 (25) United States (retrospective) Faraj 2013 (26) United States (retrospective) Fitzgerald 2013 (27) United States (retrospective) Hyder 2013 (28) United States (retrospective) Review of 45,509 patients from 1983-2007 to assess impact of age on treatment and survival (registry) Review of 58,747 patients from 2004-2007 to asses determinants of treatment outcomes (registry) Review of 2,045patients from 20082009 to assess impact of age on surgical outcomes (registry) Review of 239 patients from 19962012 to assess impact of increasing volume over time (single site) Review of 1,488 patients from 1998-2007 to assess determinants of readmission following surgery (registry) Lee 2013 (29) United States (retrospective) Review of 1,008 patients from 1993-2007 to assess impact of race on treatment and survival (registry) Shah 2013 (30) United States (retrospective) Review of 31,495 patients from 1988-2007 to assess impact of race on receipt of surgery (registry) Findings Patients ≥80 years in age had higher 30-day mortality (p=0.003) and major complications (p=0.048) compared with younger patients Determinants Patient (age) Risk of Bias Moderate African-American patients less likely than Caucasians to receive surgery (OR 0.66, 95 % CI 0.54–0.80) and chemotherapy (OR 0.75, 95 % CI 0.58 to 0.98). Non-insured patients more likely than insured patients to receive surgery (OR 1.7, 95 % CI 1.4– 2.2), uninsured less likely to receive adjuvant therapy (OR 0.54, 95 % CI 0.30 to 0.98) Younger patients (<50 years) had higher surgery (p<0.001) and radiation rates (p<0.001) and higher survival rates (p<0.0001) compared with older patients Race, socio-economic factors (low county family income, ruralurban residence, lower county education attainment) and female sex associated with lower absolute cause specific survival (p=0.0001) Older patients (>65 years) had higher thirty-day mortality compared with younger patients (OR 1.94, p=0.017) Patient (sex, race, insurance status) Low Patient (age) Moderate Patient (age, sex, SES) Moderate Patient (age) Low Appropriate use of surgical resection (p=0.0125), and palliative and adjuvant therapy (p=0.0144, p<0.0001) increased Institutional (volume) Moderate Lowest volume hospitals and surgeons had longest length of stay (p<0.001) and highest 90-day mortality (p<0.05). Factors associated with variation in patient readmission: 95.4% patient, 4.3% hospital, and 0.3% for physician factors. Elizhauser comorbidity >13 associated with readmission (OR 2.06, 95% CI 1.56 to 2.71 p<0.001) Surgical resection (OR 1.06, 95 % CI 0.60 to 1.89), chemotherapy (OR 0.92, 95 % CI 0.49 to 1.73) or radiotherapy (OR 1.14, 95 % CI 0.61 to 2.10) were similar between African-American and Caucasian patients, as was median overall survival (p=0.17) Pancreatic resection was less often recommended to (p=0.001) and performed (p<0.001) on African-American patients compared with Caucasians. African-American patients refused surgery more often when recommended (p<0.001) but this disparity decreased over time (p=0.001) Institutional (volume) Low Patient (race not significant) Low Patient (race) Low Supplemental Table 2 continued. Design and findings of eligible studies Study (design) Tamagno (31) 2013 United Kingdom (before-after) Al-Refaie 2012 (32) United States (retrospective) Singal 2012 (33) United States (retrospective) Visser 2012 (11) United States (retrospective) Objective/Methods (data source) Review of 91 patients before, and 42 patients after introducing a multidisciplinary management approach (single center) Review of 9,611 patients from 2003-2008 to assess determinants of complex surgery at low-volume hospitals (registry) Review of 16,282 patients from from 1988-2007 to assess impact of race on treatment and outcomes (registry) Review of 3,706 patients from 2001-2006 to assess factors influencing receipt of guidelinerecommended care (registry) Wray 2012 (34) United States (retrospective) Review of 1,039 patients from 1998-2010 to assess the impact of race on treatment and survival (two centers) Lemmens 2011 (35) The Netherlands (retrospective) Review of 1,139 patients before (1995-2000), and 990 patients after (2005-2008) centralizing care to higher volume centers (registry) Review of 351 patients from 20032006 to assess determinants of treatment received (registry) Review of 249 patients from 19962008 to assess impact of centralizing care to high volume centers (registry) Borgida 2011 (37) Canada (retrospective) Gooiker (36) 2011 Netherlands (retrospective) Findings The multidisciplinary approach improved consistency in biochemical, imaging, and pathological findings before treatment initiation and during follow-up, and in receipt of guidelinerecommended management Non-Caucasian patients (p<0.0001) and patients with lower income (p<0.0001) were more likely to undergo surgery at low-volume sites. Low-volume sites had higher inpatient mortality compared with higher volume sites (OR 2.53, 95% CI, 2.03 to 3.04) African-Americans had lowest survival compared with nonAfrican-Americans (HR 1.19, 95% CI 1.12 to 1.26). AfricanAmericans, Hispanics less likely to receive any treatment compared with Caucasians and Asians (p<0.0001) Older patients (>65 years) less likely to receive guidelinerecommended care (OR 0.68, 95% CI 0.46 to 0.99, p<0.045) and had higher mortality (OR 2.2, 95% CI 1.42 to 3.49, p<0.0001). Hispanic patients were less likely to receive guidelinerecommended care (p<0.0001). Survival was higher at academic (OR 0.66, 95% CI 0.51 to 0.84, p<0.0001) and higher-volume centers (OR 3.2, 95% CI 2.4 to 4.3, p < 0.0001) Older patients (OR 0.97, 95% CI 0.96 to 0.98, p<0.001), African Americans (OR 0.62, 95% CI 0.44 to 0.87, p=0.01) and Asians (OR 0.44, 95% CI 0.22 to 0.96, p=0.04) were less likely to receive chemotherapy. Mortality was higher among males (OR 0.84, 95% CI 0.73 to 0.97, p=0.02), African Americans (OR 1.2, 95% CI 1.0 to 1.4, p=0.05) and older patients (OR 1.02, 95% CI 1.0 to 1.3, p<0.001) Centralization increased resection rates (p<0.001), decreased inhospital mortality (p<0.001) and increased two-year survival (p=0.001) Determinants Intervention (multidisciplinary approach) Risk of Bias Low Institutional (volume); Patient (race, SES) Low Patient (race) Low Patient (age, race); Institution (academic, volume) Low Patient (race, sex, age) Moderate Intervention (centralization) Low Younger patients (≤70 years) were more likely to undergo curative resection (p=0.03). Resections were less frequently aborted in academic compared with non-academic centers (p<0.001) Centralization increased surgical treatment (from 14.3% to 18.4%, p=0.08), decreased risk of death (HR 0.50, 95% CI 0.34 to 0.73), and increased two-year survival from adenocarcinoma (from 28% to 49%, p=0.04). Patient (age); Institution (academic) Institutional (volume) Moderate Moderate Supplemental Table 2 continued. Design and findings of eligible studies Study (design) Woodmass 2011 (37) Canada (retrospective) Objective/Methods (data source) Review of 124 patients from 20042006 to asses determinants of surgical referral and receipt of surgery (registry) Cheung 2010 (38) United States (retrospective) Review of 16,104 patients from 1998-2002 to assess impact of SES on treatment and outcomes (registry) Review of 3,777 patients from 1992-2002 to assess impact of race on receipt of surgical care (registry) Review of 375 patients from 20002004 to assess determinants of receipt of surgery (single center) Riall 2010 (39) United States (retrospective) Sandroussi 2010 (40) Canada (retrospective) Simunovic 2010 (41) Canada (retrospective) Chang 2009 (42) United States (retrospective) Eppsteiner 2009 (43) United States (retrospective) Sharp 2009 (15) United Kingdom (retrospective) Stitzenberg (44) 2009 United States (retrospective) Review of 1,859 patients before, and 1,396 patients to assess surgical mortality after centralization of surgery in high volume centers (registry) Review of 8,370 patients from 2000-2005 to assess patient factors associated with referral to high volume centers (registry) Review of 3,581 patients from 1998-2005 to assess determinants of surgical mortality (registry) Review of 3,173 patients from 1994-2003 to assess determinants of receiving surgery, chemotherapy (registry) Review of 13,472 patients from 1996 to 2006 to assess surgical mortality after centralization (registry) Findings Among eligible patients, 39% were not referred to a surgeon, 11% underwent surgery, and 70% received no treatment. Patients younger than 65years were more likely to be referred for surgical consultation (OR 5.57, 95% CI 1.5 to 21) or undergo surgery (OR 4.6, 95% CI 1.2 to 17) Low SES patients were less likely to receive surgery (p<0.001), chemotherapy (p<0.001) or radiotherapy (14.3% vs. 16.9% p=0.003); had higher 30-day mortality (p<0.001) and lower median survival (p<0.001) African-Americans were less likely to receive surgical consultation compared with Caucasians (OR 0.57, 95% CI 0.42 to 0.77) and resection (OR 0.64, 95% CI 0.49 to 0.84) Determinants Patient (age) Risk of Bias Moderate Patient (SES) Low Patient (race) Low Older patients (OR 1.1, p<0.001), non-English speaking (OR 4.3, p=0.001), tumor type (p=0.001), and Charlson combined comorbidity index (OR 1.239, p=0.001) were associated with an increased risk of not undergoing resection Operative mortality decreased (OR 0.46, 95% CI 0.29 to 0.72, p<0.001) Patient (age, race) Low Institutional (volume) Low Patients referred were more likely to be younger than 85 years (OR 0.33, 95% CI 0.18 to 0.61, p<0.001) or non-Caucasian (OR 0.59, Patient (age, race) Low Institutional (volume); Patient (age) Patient (age, marital status) Low Institutional (volume) Low 95% CI 0.48 to 0.72 African American; OR 0.57, 95% CI 0.45 to 0.72 Hispanic; OR 0.61, 95% CI 0.43 to 0.86 Asian) Surgical mortality lower in high-volume centers (p<0.0001). Patient age associated with surgical mortality (HR 1.04, CI 1.01 to 1.07, p=0.002) Patients aged 65 to 74 (OR 0.5, 95% CI 0.37 to 0.69, p<0.001) or 75 to 84 (OR 0.18, 95% CI 0.11 to 0.28, p<0.001) and unmarried (OR 0.68, 95% CI 0.5 to 0.92, p=0.013) were less likely to receive surgery or chemotherapy After centralization surgery at low-volume centers declined (OR 0.85, 95% CI 0.84 to 0.87) Low Supplemental Table 2 continued. Design and findings of eligible studies Study (design) Yermilov 2009 (45) United States (retrospective) Bilimoria 2007 (46) United States (retrospective) Birkmeyer 2007 (47) United States (retrospective) Riall 2007 (48) United States (retrospective) Birkmeyer 2006 (49) United States (retrospective) Liu 2006 (50) United States (retrospective) Objective/Methods (data source) Review of 2,023 patients from 1994-2003 to assess determinants of readmission following surgery (registry) Review of 700 patients at Veterans Administration hospital and 28,009 patients at other hospitals from 1985-2004 to assess receipt of treatment, surgical mortality and survival (registry) Review of 855 patients from 19922002 to assess impact of hospital volume on treatment and mortality (registry) Review of 3,189 patients from 1999-2004 to assess determinants and outcomes of surgery at a highvolume center (registry) Review of 5,607 patients from 2000-2002 to assess impact of hospital volume on surgical mortality (registry) Review of 2,216 patients from 2000-2004 to assess determinants of treatment at high-volume centers (registry) Findings 59% were readmitted within one year, and readmission was associated with lower median overall survival (p<0.0001). Patients older than 73 years were more likely to be readmitted (OR 1.37, 95%, p<0.02) VA hospitals were more likely to use surgery (OR 2.20, 95% CI 1.73 to 2.79) and adjuvant chemotherapy (OR 1.77, 95% CI 1.28 to 2.46). Adjusted perioperative mortality and 3-year survival rates after surgery were similar at VA and academic hospitals. Determinants Patient (age) Risk of Bias Low Institutional (hospital type) Low Patients at low volume hospitals were substantially less likely to receive either adjuvant radiation therapy or chemotherapy (p<0.001). Mortality was lower at high-volume hospitals (OR 0.74, 95% CI 0.60–0.92) High-volume centers had lower surgical mortality compared with low-volume centers (p<0.0001). Patients who were >75 years (OR 0.51), female (OR 0.86), Hispanic (OR 0.58), and living >75 miles from a high-volume center (OR 0.93) were less likely to be resected at high-volume centers (all p<0.05) High-volume centers has lower surgical mortality (OR 4.28, 95% CI 2.93 to 6.27) Institutional (volume) Low Institutional (volume) Low Institutional (volume) Low African-Americans (OR 0.40, 95% CI 0.21 to 0.67, p<0.05) and Hispanics (OR 0.46, 95% CI 0.32 to 0.68, p<0.05, and uninsured patients (OR 0.29, 95% CI 0.07 to 0.73, p<0.05) were less likely to receive care at a high-volume Patient (race, insurance) Low