Audit of the Number of Patients Opting for and Undergoing PD in
advertisement
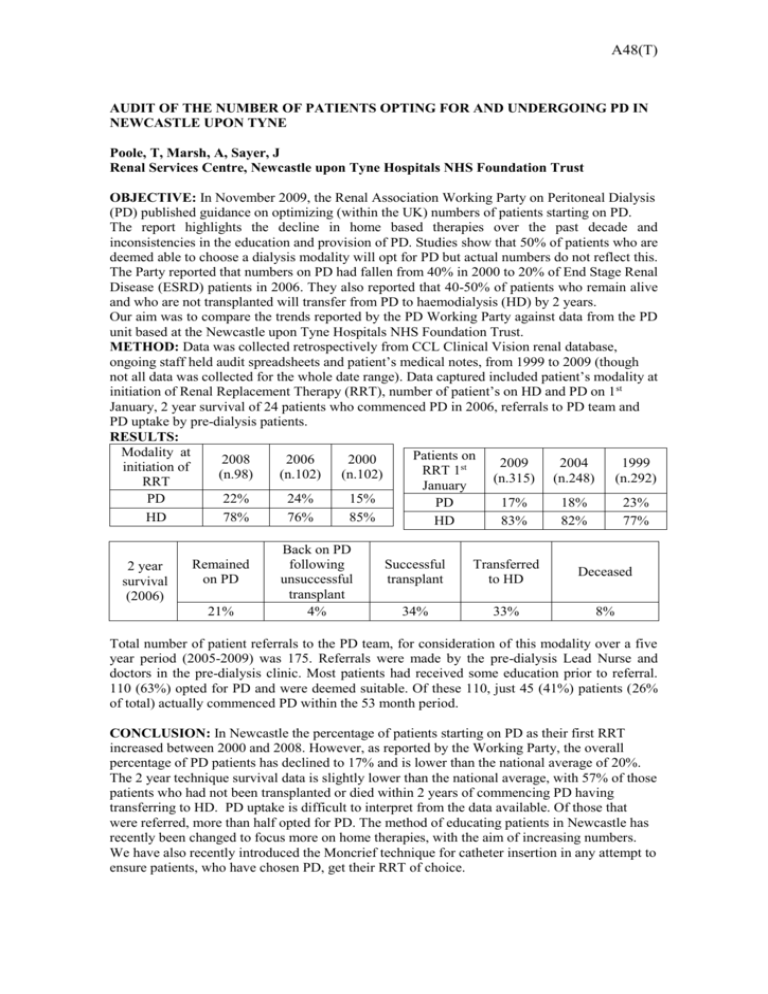
A48(T) AUDIT OF THE NUMBER OF PATIENTS OPTING FOR AND UNDERGOING PD IN NEWCASTLE UPON TYNE Poole, T, Marsh, A, Sayer, J Renal Services Centre, Newcastle upon Tyne Hospitals NHS Foundation Trust OBJECTIVE: In November 2009, the Renal Association Working Party on Peritoneal Dialysis (PD) published guidance on optimizing (within the UK) numbers of patients starting on PD. The report highlights the decline in home based therapies over the past decade and inconsistencies in the education and provision of PD. Studies show that 50% of patients who are deemed able to choose a dialysis modality will opt for PD but actual numbers do not reflect this. The Party reported that numbers on PD had fallen from 40% in 2000 to 20% of End Stage Renal Disease (ESRD) patients in 2006. They also reported that 40-50% of patients who remain alive and who are not transplanted will transfer from PD to haemodialysis (HD) by 2 years. Our aim was to compare the trends reported by the PD Working Party against data from the PD unit based at the Newcastle upon Tyne Hospitals NHS Foundation Trust. METHOD: Data was collected retrospectively from CCL Clinical Vision renal database, ongoing staff held audit spreadsheets and patient’s medical notes, from 1999 to 2009 (though not all data was collected for the whole date range). Data captured included patient’s modality at initiation of Renal Replacement Therapy (RRT), number of patient’s on HD and PD on 1st January, 2 year survival of 24 patients who commenced PD in 2006, referrals to PD team and PD uptake by pre-dialysis patients. RESULTS: Modality at Patients on 2008 2006 2000 2009 2004 1999 initiation of RRT 1st (n.98) (n.102) (n.102) (n.315) (n.248) (n.292) RRT January PD 22% 24% 15% PD 17% 18% 23% HD 78% 76% 85% HD 83% 82% 77% 2 year survival (2006) Remained on PD 21% Back on PD following unsuccessful transplant 4% Successful transplant Transferred to HD Deceased 34% 33% 8% Total number of patient referrals to the PD team, for consideration of this modality over a five year period (2005-2009) was 175. Referrals were made by the pre-dialysis Lead Nurse and doctors in the pre-dialysis clinic. Most patients had received some education prior to referral. 110 (63%) opted for PD and were deemed suitable. Of these 110, just 45 (41%) patients (26% of total) actually commenced PD within the 53 month period. CONCLUSION: In Newcastle the percentage of patients starting on PD as their first RRT increased between 2000 and 2008. However, as reported by the Working Party, the overall percentage of PD patients has declined to 17% and is lower than the national average of 20%. The 2 year technique survival data is slightly lower than the national average, with 57% of those patients who had not been transplanted or died within 2 years of commencing PD having transferring to HD. PD uptake is difficult to interpret from the data available. Of those that were referred, more than half opted for PD. The method of educating patients in Newcastle has recently been changed to focus more on home therapies, with the aim of increasing numbers. We have also recently introduced the Moncrief technique for catheter insertion in any attempt to ensure patients, who have chosen PD, get their RRT of choice.