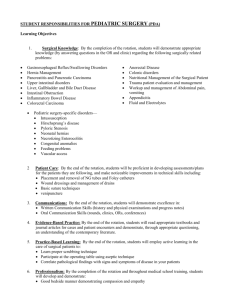
STUDENT RESPONSIBILITIES FOR PEDIATRIC SURGERY (PDA)
advertisement
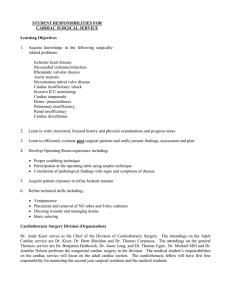
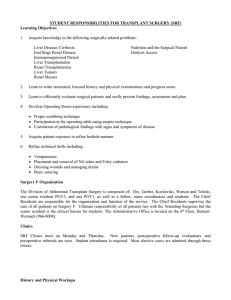
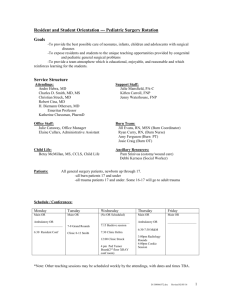
STUDENT RESPONSIBILITIES FOR PEDIATRIC SURGERY (PDA) Learning Objectives 1. Acquire knowledge in the following surgically-related problems: Acute Abdomen Necrotizing Enterocolitis Gastroesophageal Reflux Disease Gastroschisis Intussusception Intestinal Obstruction Diseases of the Liver and Gallbladder Pediatric Solid Tumors Malrotation Inflammatory Bowel Disease Gastrostomy Tubes Central Venous Catheters Hirschsprung’s Disease Hernia Nutritional Management Minimally-Invasive Surgery Congenital Anomalies Pain management in children 2. Learn to write structured, focused history and physical examinations and progress notes. 3. Learn to efficiently evaluate surgical patients and orally present findings, assessment and plan. 4. Develop Operating Room experience including: Proper scrubbing technique Participation at the operating table using aseptic technique Correlation of pathological findings with signs and symptoms of disease 5. Acquire patient exposure to refine bedside manner. 6. Refine technical skills including: Venipuncture Placement and removal of NG tubes and Foley catheters Dressing wounds and managing drains Basic suturing Pediatric Surgery Organization The Pediatric surgery service includes 5 attending surgeons (Drs. Von Allmen, Phillips, Weiner, Adamson and Lange) a chief resident, a 3rd year resident, one or two interns and 2 nurse practitioners (Lynne Farber and Amy Lamm). The Chief Residents supervise the care of all patients on Pediatric surgery. The housestaff and students are responsible to the Chief Residents. Ultimate responsibility of all patients lies with the Attending Surgeons. Clinics Pediatric surgery clinics are held every day except Tuesdays. There are also several clinics in our Raleigh office (Ask the attendings the best days to come to any of those clinics). New patients, postoperative follow-up evaluations, and preoperative referrals are seen. Student attendance is required. Most elective cases are admitted through these clinics. History and Physical Workups A major source of learning is obtained from new admission workups. Students are to obtain a complete history and perform a physical examination on all new admissions or patients seen in consultation who ultimately come to the surgical service for an operation or management. Occasionally, workups may be done during a clinic visit. New patient workups should be shared among students regarding number and disease processes. History & Physical workups should adhere to the following format: Referring Physician Infosource: Chief complaint: (c.c.) HPI PMH (medical, surgical, medications, allergy, gestational age at Birth) SH (smoking, etc) FH (any bleeding or anesthetic problems) ROS (complete, emphasis on pertinent negatives) PE (complete) Database Problem list/Assessment Plan Progress Notes Students are expected to write daily progress notes on the patients they are following. These progress notes do not replace the housestaff notes. All progress notes should contain the pertinent subjective (S) and objective (O) findings, as well as a concise assessment (A) and plan (P). The Student Progress Note must be concise and pertinent. Lab data are recorded. Assessment and plans should be discussed with a physician before writing in the chart. Remember the chart is a legal record, and statements should show responsible thinking. A minimum of one Student Progress Note every day until discharge is required. The surgical house staff and Attending physician countersign Student Progress Notes and add comments, corrections, and additions. The Student Progress Note should follow the format outlined: Date Student Progress Note PO Day # ______ S: Events and active complaints since last rounds O: Vitals signs, I/Os including drains and tubes Physical exam, focused New labs A: Concise list of active issues P: Plan for each active issue Operating Room Opportunities Each student should have the gross pathology demonstrated to him/her in the operating room on all the patients he/she is following. Student operating room assignments will be decided the day before surgery to give each student ample opportunity to read and prepare for the particular case. It is expected that each student be familiar with each case on which they scrub. Students should make every effort to see the patients pre-op. At a minimum their chart should be reviewed. Although the student following an assigned patient is expected to scrub on that operation, other students are encouraged to view operations whenever possible during the rotation. All students are expected to be knowledgeable in operating room conduct. It is the student's responsibility to check on the time of the operative procedure so that he/she may plan his/her activities to be present. Students may elect to go to WakeMed to get more exposure to surgical procedures with the attendings that operate over there. This is an excellent way for students to have more one-on-one time with the attendings and often act as first assistants. Check with the attendings to find out the best days to spend the morning or entire day at WakeMed. On Call PDA students are On-Call as directed in the clerkship orientation materials. Each on-call student should notify the Resident On-Call where he/she can be reached. Orders Students are to learn to write postoperative orders. This is done by observing the housestaff during computerized physician order entry. Proper organization of orders is a high priority. Knowledge of the correct dosage of medicine, proper laboratory tests, and nursing orders is necessary. Conferences There is an abundance of formal teaching sessions that meet on a regularly scheduled basis on PDA. The students should attend as many of these sessions as possible. Priorities include: 1. Cross Block Lectures - 7:30 am Monday, Tuesday, Thursday; 8:30 am Wed, 8:00 am Friday OR classroom 2. Surgery Grand Rounds - 7:15 am Wednesday, Clinic Auditorium 3. M & M Conference - 5:00 pm Wednesday - OR classroom 4. Division M&M 7:00am 1st and 3rd Monday, 3010 Old Clinic Building conference room 7. Tutorials – As scheduled with Attending Physicians Rounds Early morning Work Rounds are conducted by the housestaff to determine any changes in each patient's condition and make decisions regarding management for the day. Students are responsible for keeping abreast of the clinical condition of their patients and decisions for management. An attending (or sometimes more than one) will round with the housestaff and students on all of the patients in the afternoon. Questions and discussion are encouraged. Students should be able to present a brief, but concise synopsis of the patient's problem and progress on rounds. Evaluations Mid-rotation feedback will be provided by faculty members and residents at the 2-week point. Specific feedback will be given related to submitted write-ups available and overall performance. Students are encouraged to seek feedback and recognize it in all its forms. At the completion of each rotation, the attendings and housestaff meet to discuss the performance of the students. Patient care, Knowledge, Self-improvement, Communication skills, Professionalism and system-based practice are the main areas that will be evaluated. A consensus evaluation form is then submitted to the Surgery Clerkship Office usually within two weeks of the end of the rotation. Students are encouraged to meet with the Section Chief or other faculty members to review their evaluations. Revised 3/6/07 PL