TITLE: Efficacy of Posterior-Only Approach and Pedicle Subtraction
advertisement
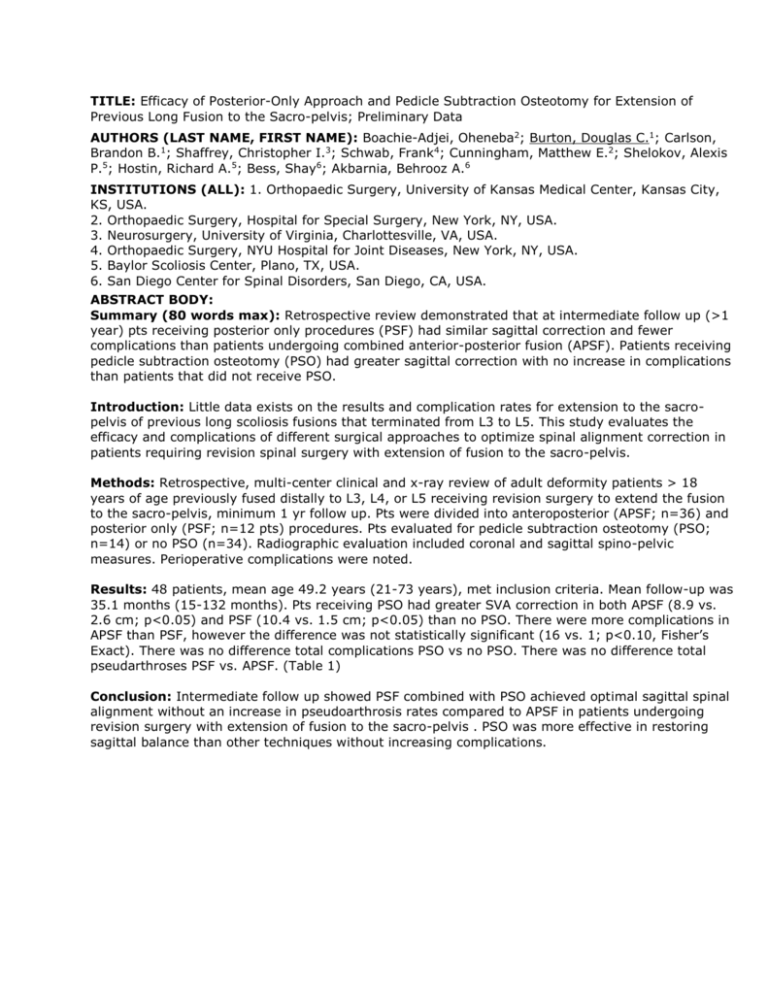
TITLE: Efficacy of Posterior-Only Approach and Pedicle Subtraction Osteotomy for Extension of Previous Long Fusion to the Sacro-pelvis; Preliminary Data AUTHORS (LAST NAME, FIRST NAME): Boachie-Adjei, Oheneba2; Burton, Douglas C.1; Carlson, Brandon B.1; Shaffrey, Christopher I.3; Schwab, Frank4; Cunningham, Matthew E.2; Shelokov, Alexis P.5; Hostin, Richard A.5; Bess, Shay6; Akbarnia, Behrooz A.6 INSTITUTIONS (ALL): 1. Orthopaedic Surgery, University of Kansas Medical Center, Kansas City, KS, USA. 2. Orthopaedic Surgery, Hospital for Special Surgery, New York, NY, USA. 3. Neurosurgery, University of Virginia, Charlottesville, VA, USA. 4. Orthopaedic Surgery, NYU Hospital for Joint Diseases, New York, NY, USA. 5. Baylor Scoliosis Center, Plano, TX, USA. 6. San Diego Center for Spinal Disorders, San Diego, CA, USA. ABSTRACT BODY: Summary (80 words max): Retrospective review demonstrated that at intermediate follow up (>1 year) pts receiving posterior only procedures (PSF) had similar sagittal correction and fewer complications than patients undergoing combined anterior-posterior fusion (APSF). Patients receiving pedicle subtraction osteotomy (PSO) had greater sagittal correction with no increase in complications than patients that did not receive PSO. Introduction: Little data exists on the results and complication rates for extension to the sacropelvis of previous long scoliosis fusions that terminated from L3 to L5. This study evaluates the efficacy and complications of different surgical approaches to optimize spinal alignment correction in patients requiring revision spinal surgery with extension of fusion to the sacro-pelvis. Methods: Retrospective, multi-center clinical and x-ray review of adult deformity patients > 18 years of age previously fused distally to L3, L4, or L5 receiving revision surgery to extend the fusion to the sacro-pelvis, minimum 1 yr follow up. Pts were divided into anteroposterior (APSF; n=36) and posterior only (PSF; n=12 pts) procedures. Pts evaluated for pedicle subtraction osteotomy (PSO; n=14) or no PSO (n=34). Radiographic evaluation included coronal and sagittal spino-pelvic measures. Perioperative complications were noted. Results: 48 patients, mean age 49.2 years (21-73 years), met inclusion criteria. Mean follow-up was 35.1 months (15-132 months). Pts receiving PSO had greater SVA correction in both APSF (8.9 vs. 2.6 cm; p<0.05) and PSF (10.4 vs. 1.5 cm; p<0.05) than no PSO. There were more complications in APSF than PSF, however the difference was not statistically significant (16 vs. 1; p<0.10, Fisher’s Exact). There was no difference total complications PSO vs no PSO. There was no difference total pseudarthroses PSF vs. APSF. (Table 1) Conclusion: Intermediate follow up showed PSF combined with PSO achieved optimal sagittal spinal alignment without an increase in pseudoarthrosis rates compared to APSF in patients undergoing revision surgery with extension of fusion to the sacro-pelvis . PSO was more effective in restoring sagittal balance than other techniques without increasing complications.