Failure of separation
advertisement

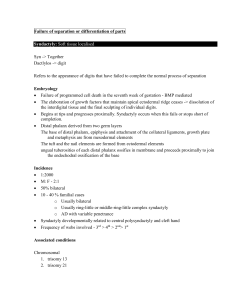
Failure of separation or differentiation of parts Syndactyly: Soft tissue localised Syn -> Together Dactlylos -> digit Refers to the appearance of digits that have failed to complete the normal process of separation Embryology Failure of programmed cell death in the seventh week of gestation - BMP mediated The elaboration of growth factors that maintain apical ectodermal ridge ceases -> dissolution of the interdigital tissue and the final sculpting of individual digits. Begins at tips and progresses proximally. Syndactyly occurs when this fails or stops short of completion. Distal phalanx derived from two germ layers The base of distal phalanx, epiphysis and attachment of the collateral ligaments, growth plate and metaphysis are from mesodermal elements The tuft and the nail elements are formed from ectodermal elements ungual tuberosities of each distal phalanx ossifies in membrane and proceeds proximally to join the endochodral ossification of the base Incidence 1:2000 M: F - 2:1 50% bilateral 10 - 40 % familial cases o Usually bilateral o Usually ring-little or middle-ring-little complex syndactyly o AD with variable penetrance Syndactyly developmentally related to central polysyndactyly and cleft hand Frequency of webs involved - 3rd > 4th > 2nd> 1st Associated conditions Chromosomal 1. trisomy 13 2. trisomy 21 Craniofacial Aperts Pfeiffer Carpenter Saethre-Chotzen Mobius Oro-facial-digital Pierre Robin Others Polands anomaly TAR Holt-Oram syndrome Classification Simple only soft tissue webbing present. Complex Bony fusion between adjacent fingers May involve all of phalanges or only at tips – acrosyndactyly (due to constriction band) Complicated syndactyly in which more than simple side-side bony fusion exists. Complete: involved digits unite throughout length Incomplete: Common web extends a variable length along fingers but not as distal as DIP joint Anatomic pathology fingers are joined by excess fascial connections across the syndactyly, which link with Cleland and Graysons ligaments. o responsible for growth retardation The tuft of distal phalanx are joined in complex syndactyly but the base and collateral structures are separate and normal Underlying skeletal, tendon and neurovascular variations common o Should explore vascular bundles first in surgery Symphalangism occurs commonly with syndactyly in symbrachydactyly and many craniofacial syndromes with syndactyly Phalangeal abnormalities common – delta thumb phalanx, clinodactyly Presence of synonychia or absence of differential motion of the DIPJ indicates underlying bony involvement (complex syndactyly) Contraindication for surgery GA contraindications Severe mental retardation Lack of concern for syndactyly Treatment Aims 1. improve function 2. improve cosmesis 3. permit normal growth Principles 1. Creation of commissure using a proximally based dorsal flap 2. Separation of involved digits using volar /dorsal triangular flaps and FTSG placed along lines to minimize contractures 3. Operate on 1 side of the finger at one time 4. Create a normal nail 5. Correct skeletal anomaly Timing of surgery Surgical release early to allow growth of affected digits and prevent malrotation and angulation (due to differential growth rates of the involved fingers) –especially involving 1st web and 4th webs where digits are unequal length (4-6 mths of age, others at one yr) In older child (>18 months) , procedures should be staged unilaterally as they do not tolerate bilateral immobilisaion Planning normal web ends midway down the proximal phalanx. hourglass configuration wider distally than proximally, with a 45° slope dorsal to palmar. In multiple web involvement, priority given to thumb index and ring-middle finger webs. Release can also be done in the other webs from tip to DIPJ to reduce urgency of the second stage. Polydactylous components can be used as spare parts Methods 1) Mild incomplete simple syndactyly New commissure reconstructed using one or more flaps Dorsal flaps best to deepen web A) Butterfly (double opposing Z) flap B) Dorsal flap C) Four flap Z- plasty for thumb and index finger 2) Moderate to complete syndactyly Volar and dorsal interdigitating flaps are essential to prevent volar skin contractures. Usually possible to achieve skin cover with flaps distal to PIPJ but skin grafts are required proximal to PIPJ Usually more dorsal than volar skin FTSG are used to cover residual defects and usually from groin (taken lateral to femoral art to reduce hair growth) o If possibility of requiring groin flap in the future, harvest FTSG from Pfannenstiel incision. o Other donors – plantar aspect of foot, hypothenar eminence and penile foreskin (poor color match) In complex syndactyly when bone is exposed, bone should be covered with flap of subcutaneous tissue before grafting or graft onto cancellous bone Finger tips require reconstruction of nail fold Divide fascial bands - proximal division of the common digital nerve is often the structure limiting the proximal release. Skin incision Dorsal flap drawn beginning at the metacarpal heads and extends to a point 2/3rd the way between points placed between the prominences of the metacarpal heads and the heads of the proximal phalanx when pip jts are flexed. The width of the flap tapers distally by one half and the distal edge of the flap is perpendicular or only slightly angled to the long axis of the flap The length of this flap must be longer than the halfway point of the proximal phalanx The palmar incisions are planned by placing dots at the mid web at the level of the digital flexor crease. Brunners are then drawn by crossing from one finger onto the other at the dots. Tips of the Brunners end at the middorsal line of each finger Reciprocal dorsal flaps are created by matching apex to defect and matching length of flap where there is enough skin to allow closure. Any defects ftsg from groin Finger tips Finger tips complete sydactyly vary in the amount and contour of the pulp tissue If there is inadequate tissue, may replace with 1. ftsg, 2. thenar flaps, 3. local and distal flaps 4. composite tissue from hypothenar eminence or fibular aspect of big toe a. accurate skin apposition as revascularisiation occurs here Finger nails eponychial fold – laterally based interdigitating flaps (Buck-Gramcko) Post op Sutures used 6’0 catgut Splint Dressings intact for 2-3 weeks Causes of failure 1. Circulatory deficit a. Digital necrosis - both sides of digit should not de operated on at same time) If circulatory problems release dressings and grafts 2. Contracture a. Most often in the web space 3. Web creep/ Recurrence a. advancement of commissure distally (10-60%) b. early - usually due to the presence of synechiae between the incisional lines c. late – due to differential growth rates between the scar and the surrounding tissue, leading to the appearance of an incomplete simple syndactyly Aperts Syndrome Acrocephalosyndactyly syndrome type 1 defect in chromosome 10, arm q, site of the fibroblast growth factor-2 receptor. Incidence 1 in 100,000 – 160,000 Highest in Asians Clinical Four features: 1. Complex syndactyly always involving the index, middle and ring fingers - sharing common nail (synonychia). 2. short radially deviated thumb - due to an abnormally shaped proximal phalanx (ie, delta phalanx); 3. symbrachyphalangism of the central segments of the index, long, ring, and small fingers 4. simple syndactyly of the fourth web. Movement at MCP preserved. fifth finger usually being the least affected. Symphalangism is the process of progressive calcification and fusion of the interphalangeal joints to form a single phalanx. the proximal interphalangeal joints are usually not present, either because they have formed and then fused prenatally or have failed to develop at all The distal interphalangeal joints are usually present but have a limited range of motion. They progressively stiffen with age, until no movement is possible, usually at the age of 5 or 6. These ankylosed distal interphalangeal joints eventually calcify completely, forming a single abnormal phalanx in the digit Abnormal epiphyseal plate function are responsible for brachydactyly and abnormal growth, including clinodactyly, following syndactyly release Upton Classification Classified into three depending on degree of thumb involvement Type 1. Thumb free a. Most common – spade hand b. thumb short with a radial clinodactyly due to a delta phalanx of the proximal phalanx. c. Shallow first web space d. 4th web simple syndactyly - complete or incomplete 2. Thumb simple syndactyly a. Mitten hand b. simple complete or incomplete syndactyly of 1st web space 3. Thumb complex syndactyly a. Rosebud hand b. Most severe, least common c. Tight cartilaginous or osseous union of thumb/index/middle/ring d. All 5 nail plates are conjoined, and they sometimes have longitudinal ridges, which indicate separate underlying distal phalanges. e. Thumb is indistinguishable from the index ray. f. Little finger although joined by a common fingernail, does not have an osseous union at the distal phalanx and remains a simple but complete syndactyly. Surgical aims 1. separation of the digits and thumb 2. lengthening and realignment of the thumb Chang PRS Feb 2002 Zuker recommends Upton type I or II hands, - syndactyly release and full-thickness skin graft only. More severe type II hands may need composite toe-pulp grafts for small areas of exposed bone or joint at the long-ring web. type III, or rosebud, hand poses the greatest difficulty. Priorities here should be an adequate thumb-index web space (which requires a large dorsal skin flap and split-thickness skin graft at the donor site), separation of the border digits (which requires local flaps and skin grafts), and separation of the long-ring web with preservation of each finger. This requires osteotomies and coverage of significant adjacent areas of exposed bone, joint, and soft-tissue deficiency. Upton Type 1. Pre and post op Upton Type 2. Pre and post op Upton Type 3. Pre and post op Arthrogryposis: Soft tissue generalised Collection of conditions with unknown cause but share similar characteristics Incidence Most are sporadic 1 in 3000 Aetiology Most common cause is amyoplasia – fibrofatty infiltration of muscles Clinical Most common pattern encountered: o Wasted shoulders with deficient soft tissues o Shoulders have no abduction and held in internal rotation o Elbows held in extension o Wrist in flexion and ulnar deviation o Fingers flexed especially at MCPJ o Thumbs clasped in adduction and flexion o Absent skin creases Management Passive manipulation and splinting needs to be tried first Shoulder Derotational osteotomy – proximal third of humerus Fusion of glenohumeral joint generally not recommended Elbow Posterior release of elbow capsule with Z lengthening of triceps Avoid correcting both elbows (need 1 in extension for perineal care) To achieve active flexion 1. Pectoralis major transfer o Disadvantage reduces power for thoracohumeral grasp and scissor grasp between 2 limbs o Advantage better excursion/power than Steindler flexorplasty o Insertion is attached to coracoid process (more shoulder adduction) or acromion (more shoulder flexion) o Muscle belly is tubed o Origin + rectus fascia is attached to Biceps tendon (rarely present) Ulnar medial to flexor, pronator mass – preferable Radius – may cause radial head dislocation o Splint for 3 weeks in adduction to prevent tension on medial pedicle 2. Steindler flexorplasty o Proximal transposition of common flexor pronator origin o Produces an elbow flexion contracture – helps to initiate elbow flexion o Not as powerful as pectoralis transfer o Disadvantages: To produce elbow flexion, forearm flexors and pronator must contract Tendency for progressive flexion or pronation contractures – minimize by inserting flexors medially on humerus 3. Triceps Transfer o Disadvantages: Flexion contracture (unopposed flexion) o Advantages Simple Can be done together with posterior capsule release o Detach insertion with strip of periosteum, dissect up to spiral groove and swing round to attach to ulna or radius. 4. Others: o Free gracilis transfer o Lattisimus transfer Not available in arthrogryposis o Pectoralis minor and SCM described Wrist Bony correction –volar capsular release, dorsal wedge osteotomy, proximal row carpectomy Tendon transfer o deforming FCU is transferred to act as a radial extensor o pronator teres reinserted as a supinator by step division based distally and carried round the radius. Fingers Combination of capsular releases and skin grafting/local flaps Skin shortage volarly is the rule Release indicated for severe deformities for hygiene and to allow splintage even if complete correction not possible Windblown Hand: Soft tissue Craniocarpotarsal dystrophy May be a distal form of arthrogyyposis Consists of flexion and adduction contracture of thumb, narrowing of 1st web space, thenar muscles often hypoplastic camptodactyly ulnar deviation of fingers at MCPJ Part of Freeman-Sheldon syndrome o Usually sporadic, also Autosomal dominant o Mask like facies o paramedian grooves between the lower lip and the chin tip. (H shape) o long philtrum. o Hypoplastic alar o Small whistling mouth o Clubfeet Management Nonoperative o Splinting to hold out thumb and fingers in extension, maintain 1st web space Correct ulnar deviation Surgical o Volar release Transverse incision across base of finger and skin grafting Abnormal fascial bands need to be released Lengthening finger flexors release of joint capsules st o 1 web space Dorsal flap to recreate web space release of the adductor pollicis, the first dorsal interosseous muscles, or both o Radialise fingers Centralise extensor tendons - Release ulnar sagital bands and plicate radial bands Cross intrinsic transfers o Opponenplasty Ring finger superficialis transfer o Derotational osteotomy Subcapital osteotomy of metacarpus for ulnar deviation not otherwise correctable Congenital clasped thumb: Soft Tissue Infants stop clasping thumb at 3-4 mths of life Clinical Characteristic posture shows extreme flexion of MCP jt with adduction into palm secondary to extensor side underdevelopment, flexor side tightness, or both. Seen in isolation or as part of wind blown hand Incidence M: F - 2:1 often bilateral Classified into four groups Group one (mild) Deficient extensor mechanism with no contracture treated with splinting before 6months Group two deficient extension with flexion contracture if flexion contracture is not passively correctable then surgical release plus z plasty or dorsal flap Group Three hypoplasia of the muscle and tendons and may be variant of hypolastic thumb FPL and abductor transverse head require lengthening tendon transfers required for powering extension (EI may be hypoplastic thus consider PL, FDS, BR) Group four clasped thumb in association with ext mechanism deficiency and polydactyly If resistant may require fusion of the MCP joint Congenital Triggering: Soft Tissue As in adults, thumb more common than fingers 2 percent of all congenital upper extremity anomalies Some believe this is an acquired deformity Does not present until at least 3-4 months due to normal flexion posturing of the thumb until this age Aetiology Unknown ? due to lack of separation of the FPL tendon from the pulley Mangement 30-50% will spontaneously resolve by 1yr Surgery delayed until 2nd yr As long as deformity corrected by 3rd year no long term contracture results Surgery involves release of thickened sheath without trimming of nodule Camptodactyly: Soft Tissue congenital flexion deformity of the proximal interphalangeal (PIP) joint. which most often affects the little finger. It may affect all fingers with incidence greatest on the ulnar side and diminishes towards radial side Condition worsens with time if left untreated Worsens during growth spurts Classification (Siegert) 1. Simple – isolated lexion deformity of the PIP joint only 2. Complex - associated with other deformities (e.g., syndactyly, clinodactyly, arthrogryposis) Incidence 1% of population, only affects Caucasians 2/3rd bilateral 80% present in infancy (M=F) 20% present in adolescence (mainly female) Most cases are sporadic with some familial AD inheritance Anatomy All layers involved - Skin, fascia (retinaculum cutis), tendon sheaths, flexor digitorum superficialis tendon, lumbricals and interossei (particularly the lateral bands), joint capsule, neck of the proximal phalanx, and extensor. Theory of disturbed equilibrium between flexor and extensor forces Controversial which is primary and which is secondary Nearly always found are an abnormal insertion of lumbrical (to MCPJ capsule, FDS) and a shortened FDS tendon Flattening and tapering of the proximal phalanx (chisel-shaped head of proximal phalanx) shown on x-rays are secondary and due to compression of the head by the central slip, which is attenuated and stretched. Examination Extension correctable or non correctable correctable in MP flexion– implying problem is proximal to MCPJ rotation (supination) may be present in long standing cases as an adaptive change pain on extension may indicate abnormal insertion of lumbrical to FDS just proximal to A1 pulley Differential Diagnosis 1. juvenile palmar fibromatosis (mimics Dupuytrens’s) 2. Trigger finger Management Non Operative Stretching and splintage – cornerstone of treatment Operative Indications failure of conservative treatment PIPJ contracture >30 Skin shortage o FTSG o Volar Z plasties o Local flap – Glicenstein: proximally based flap is transposed 90 to fill the defect across the base of the finger. Retinaculum cutis o runs from the pretendinous band distally and includes the lateral digital sheets. o Divide this tough fascia including the bony attachment of Grayson's ligaments. FDS tendon o Test with tenodesis to determine if short Lengthen Divide if there is proximal aplasia of tendon Lasso procedure Transfer to lateral band Lumbricals o Divide abnormal insertion Intrinsics o lateral bands of the intrinsic apparatus and interosseous muscles are freed from their abnormal and widespread attachment to the sides of the proximal phalanx. Volar plate o Released FDP tendon o In severe cases, insertion raised subperiosteally and reinserted more proximally Symphalangism: Skeletal involvement Failure of interphalangeal joint differentiation Symphalangism is the process of progressive calcification and fusion of the interphalangeal joints to form a single phalanx. Although xray shows a space, the joint consists of a solid cartilaginous bar Incidence 1. 0.5% of congenital hands 2. 50% inherited Classification 1. true symphalangism - the digits are of normal length. 2. brachysymphalangism - the digits are short as well as stiff. 3. syndromic symphalangism - related to specific syndromes, particularly Poland and Apert syndromes. Clinical Most have associated brachydactyly Absent creases Stiffness actively and passively Radiograph may show joint space No joint capsules and no proper synovial Jt cavity with both flex and ext tendons absent and no flex and ext skin creases Treatment Vascularised second toe IP joint transfer promising Arthoplasty and arthodesis generally disappointing (Flatt) Palmieri reported good results with silastic implant in adults Clinodactyly: Skeletal Congenital radial or ulnar deviation of digits (>10 considered abnormal) Most commonly radial deviation of little finger at DIP joint due to middle phalanx that has trapezoidal shape (delta phalanx) Incidence 1% of births Most inherited – AD, most of these bilateral Aetiology Due to abnormal angulated phalanx, most commonly middle phalanx (very rarely metacarpus) Angulated growth due to longitudinal bracketed epiphysis Associations Craniofacial syndromes – Carpenter, Aperts (thumb) Symbrachydactyly Downs syndrome (80%) Indications for Surgery Rarely causes functional problems Surgery risks disrupting growth Treatment Vickers popularized interpositional fat after resection of bracket at age 3-4years Other options are opening or closing osteotomies Kirner’s Deformity Progressive volar and radial curvature of the distal segment of the little finger F>M 2:1 Fingernail becomes markedly shortened and curved Aetiology Idiopathic nontraumatic disruption of distal phalanx physis - ? secondary to abnormal pull of FDP Treatment Rarely required, largely cosmetic Early treatment – dorsal hemiepiphysiodesis Late treatment – multiple volar osteotomies bone graft