Volume 26 - No 5: Fusarium
advertisement
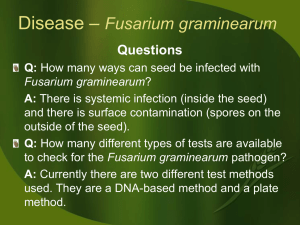
JOHNS HOPKINS U N I V E R S I T Y Department of Pathology 600 N. Wolfe Street / Baltimore MD 21287-7093 (410) 955-5077 / FAX (410) 614-8087 THE JOHNS HOPKINS MICROBIOLOGY NEWSLETTER Vol. 26, No. 05 Tuesday, March 6, 2007 A. Provided by Sharon Wallace, Division of Outbreak Investigation, Maryland Department of Health and Mental Hygiene. 17 outbreaks were reported to DHMH during MMWR Week 9 (Feb. 25- Mar. 3, 2007): 13 Gastroenteritis outbreaks 7 outbreaks of GASTROENTERITIS associated with Nursing Homes (Baltimore City, Talbot Co., Montgomery Co., Allegany Co., Calvert Co., 2 Harford Co.) 3 outbreaks of GASTROENTERITIS associated with Assisted Living Facilities (Washington Co., 2 Montgomery Co.) 2 outbreaks of GASTROENTERITIS associated with Hospitals (Wicomico Co., Baltimore Co.) 1 outbreak of GASTROENTERITIS associated with an Adult Daycare (Baltimore City) 4 Respiratory illness outbreaks 1 outbreak of INFLUENZA associated with a Nursing Home (Baltimore City) 2 outbreaks of STREPTOCOCCAL PHARYNGITIS/ SCARLET FEVER associated with Schools (Caroline Co., Wicomico Co.) 1 outbreak of SCARLET FEVER associated with a Daycare (Wicomico Co.) B. The Johns Hopkins Hospital, Department of Pathology, Information provided by, Alexandra C. Hristov, M.D. Case Summary: The patient is a 64-year-old man status post a living unrelated renal transplant on 7/2006 for end stage renal disease secondary to focal segmental glomerulosclerosis. On 2/1/2007, the patient was admitted via the emergency department for severe abdominal pain and rigid abdomen and was subsequently diagnosed with cecal volvulus requiring an exploratory laparotomy and right hemicolectomy. The patient’s post-operative course was notable for acute renal failure requiring stress dose steroids followed by dyspnea of unclear etiology requiring extended supplemental oxygen. The patient was eventually discharged on 2/17/2007, but returned 5 days later with worsening dyspnea and radiographic evidence of new right upper lobe pneumonia and increased pleural effusions. Organism: Fusarium is a filamentous fungus widely distributed on plants, in the soil and in water. It is a transient component of aeroflora and is a common contaminant of commodities such as rice, bean and soybean. Currently, there are over 20 known species of Fusarium, with only some causing infections in humans. Notably, Fusarium is an emerging cause of opportunistic mycoses. Clinical Significance: Fusarium is a causative agent of superficial, locally invasive and systemic infections in humans. Fusarium solani is the most virulent Fusarium species. In immunocompetent hosts, the most common infections include keratitis and onychomycosis. Fusarial keratitis is particularly associated with contact lens use and has also been associated with contact lens solutions. Trauma, particularly burns, is a major predisposing factor for the development of cutaneous infections. Immunocompromised patients, especially transplant and neutropenic patients, may develop disseminated infections. In particular, patients with prolonged neutropenia or T-cell deficiencies are at risk. Fusarium have been reported to cause a variety of other infections in both immunocompetent and immunocompromised hosts including endophthalmitis, otitis media, onychomycosis, mycetoma, sinusitis, pulmonary infection, endocarditis, peritonitis, central venous catheter infections and septic arthritis. Fusarial pneumonia is more common among immunocompromised patients and is nonspecific both clinically and radiographically. Typically, it presents with dry cough, dyspnea, and pleuritic chest pain, and displays nonspecific alveolar or interstitial infiltrates, nodules or cavities on chest imaging. The prognosis of fusarial infections depends upon disease extent and immunosuppression, particularly neutropenia. Of note, Fusarium infections following solid organ transplantation tend to remain local and have a better outcome compared to patients with hematologic malignancies or patients who have received a bone marrow transplant. Fusarium also contributes to human illness via toxin elaboration. Ingestion of grains contaminated with Fusarium toxins can lead to allergic reactions or may be carcinogenic with long-term exposure. Epidemiology: Fusarium enters its host most commonly through the airways, via inhalation of aerosolized conidia. Sites of skin breakdown and possibly mucosal membranes are other sites of entry. Nosocomial infections have been reported and may be caused by contamination of hospital water systems or hospital plants. Most commonly, Fusarium affects cancer patients, particularly those with acute leukemia, but can affect immunocompetent and immunocompromised hosts. Since the approximately the mid-1970s, the epidemiology of invasive fungal infections has changed. The incidence has increased, the patient populations at risk have expanded and the infectious etiology is more likely to be molds such as Fusarium. Proposed causes for these changes include medical interventions such as chemotherapeutic agents with resulting neutropenia, antifungal prophylaxis and medical devices, or changes in the host including more severe immunosuppression or different types of immunosuppression. Laboratory Diagnosis: Fusarium grow rapidly on Sabouraud dextrose agar at 25C and produce woolly to cottony, flat, spreading colonies, and may display a variety of colors from the surface (creamy, white, tan, salmon, cinnamon, yellow, red, violet, pink or purple) or the reverse (colorless, tan, red, dark purple or brown). Fusarium will grow on all fungal media not containing cyclohexamide. Microscopically, Fusarium display hyaline septate hyphae that branch at 90 and acute angles, conidiophores, phialides, macroconidia and microconidia. Phialides are cylindrical with a small collaret, and may be solitary or part of a complex branching system. They may also be monophialides or polyphialides. Macroconidia are produced from phialides on unbranched or branched conidiophores and are composed of 2 or more cells with a thick wall. They may be smooth and cylindrical or canoe-shaped, they have a distinct basal foot cell and pointed distal ends, and they accumulate in balls or rafts. Microconidia are formed on long or short unbranched conidiophores. They are 1,2 or 3 celled, smooth, hyaline, ovoid to cylindrical, and arranged in balls or occasionally chains. The diagnosis of Fusarium is based on macroscopic and microscopic features including colony color, macroconidia length and shape, and the number, shape and arrangement of microconidia. Molecular methods, such as 28s rRNA gene sequencing may also be used for rapid identification of six medically important Fusarium to the species level. Treatment: Fusarium is one of the most drug resistant fungi. In particular, Fusarium solani is the most drug resistant of all. Fusarium has high MICs for many antifungal agents (flucytosine, ketoconazole, miconazole, fluconazole, itraconazole and posaconazole) and is intrinsically resistant to the glucan synthesis inhibitors caspofungin, anidulafungin, and micafungin. Amphotericin B, voriconazole, and natamycin have low MICs. Voriconazole and posaconazole are effective choices for Fusarium. Amphotericin B, particularly lipid formulations, alone or with flucytosine or rifampin is commonly used for fusariosis. For localized Fusarium infections, antifungal therapy should be preceded by surgical debridement. For optimal therapy, fungal susceptibility should be determined and the antifungal agent should be administered at the highest tolerable doses. Unfortunately, Fusarium is difficult to treat and invasive forms are often fatal. Fusarial infections can be prevented in the immunocompromised host by limiting patient exposure to sources of Fusarium such as tap water and improperly cleaned showers. Before hematopoietic stem cell transplant, a thorough evaluation of skin and nails for breakdown or evidence of onychomycosis may also help to prevent infection. Finally, for patients with known fusarial infection, improving neutropenia or reducing immunosuppression as well as antifungal prophylaxis can prevent recurrence. References: 1. 2. 3. 4. 5. 6. Chang, DC et al. Multistate outbreak of Fusarium keratitis associated with use of contact lens solution. JAMA 2006. 296(8): 953-963. Enoch, D.A. et al. Invasive fungal infections: a review of epidemiology and management options. J Medic Micro 2006. 55:809-818. Merz, W.G. et al. Diagnosis and successful treatment of Fusariosis in the compromised host. J Infect Dis 1988. 158(5):1046-1055. Nucci, Marcio and Elias Anaissie. Emerging fungi. Infect Dis Clin N Am 2006. 20:563-579. Procop, G.W. and G.D. Roberts. Emerging fungal diseases: the importance of the host. Clin in Lab Med 2004. 24(3): 691-719. Summerbell, R. “Ascomycetes: Aspergillus, Fusarium, Sporothrix, Piedraia, and Their Relatives.” in Pathogenic Fungi in Humans and Animals. J.W. Bennett ed. 395-411. Fusarium spp. www.doctorfungus.com