(6) Systems-based Practice
advertisement

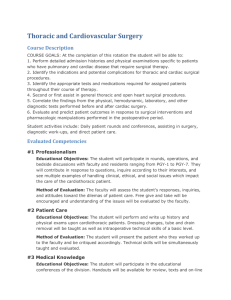
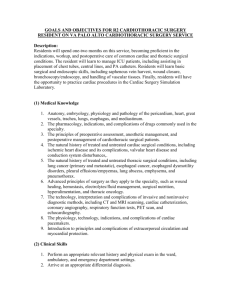
GOALS AND OBJECTIVES FOR R1 CARDIOTHORACIC SURGERY RESIDENT ON THORACIC SURGERY SERVICE Description The thoracic surgery rotation at Stanford Hospital will be serve as an introduction to general thoracic surgery (common and tertiary care patients), including preoperative workup and postoperative care. Residents will learn how to recognize and care for critically ill patients, including placement of chest tubes and obtaining central venous access. Finally, this rotation will teach basic surgical and endoscopic techniques. (1) Medical Knowledge 1. Anatomy, embryology, physiology and pathology of the trachea, lungs, esophagus, pleura, and mediastinum. 2. The pharmacology, indications, and complications of drugs commonly used in the specialty, including anti-arrhythmics, diuretics, anticoagulants, bronchodilators, and pain medications. 3. The general principles of preoperative assessment and postoperative management of thoracic surgical patients. 4. The natural history of treated and untreated diseases of the specialty, including lung cancer, esophageal cancer, emphysema/COPD, interstitial lung diseases, esophageal dysmotility disorders, and Barrett’s esophagitis. 5. Principles of surgery, including hemostasis, wound healing, wound complications, electrolyte and fluid replacement, surgical nutrition, and oncology. 6. Understand common postoperative care issues in the thoracic surgery patient, including pain management, exercise expectations/limitations, need for home oxygen, indications for SNF/rehab facility. 7. Understanding of pulmonary function tests, ABGs, ventilation-perfusion tests, MVO2 studies, and esophageal mannometry studies. (2) Clinical Skills 1. Perform an appropriate relevant history and physical exam in the ward, ambulatory clinic, and emergency department settings. 2. Order appropriate laboratory, radiological and other diagnostic procedures. 3. Demonstrate knowledge in the interpretation of laboratory investigations, CXR, ECG, CT scan, MRI, and PET scan. 4. Arrive at an acceptable plan of management for the disease process, including differential diagnosis. 5. Manage the patient throughout as much of the hospital stay as possible demonstrating knowledge and ability to recognize potential complications of the disease process and operative procedures. 6. Demonstrate ability to perform daily resident work rounds efficiently, including dictation of operative cases performed, daily progress notes, dictation of discharge summary, prescription writing. 7. Provide a plan for patient follow-up. 8. Assessment/triage of urgent/emergent thoracic surgery patients. (3) Patient Care Expected: 1. Function as a first or second assistant in the operating room for common thoracic surgery cases, including a lobectomy, VATS wedge resection/biopsy, mediastinoscopy, and esophagectomy. 2. As primary surgeon, resident should perform a posterior lateral thoracotomy and participate in thoracotomy closure. 3. As primary surgeon, resident should perform flexible bronchoscopy, with understanding of bronchial segmental anatomy. 4. Handle tissues and surgical instruments in an appropriate manner, and demonstrate adherence to sterile techniques. 5. Insertion and removal of chest tubes and performance of thoracentesis outside the operating room. 6. Manage cardiac arrhythmias and common postoperative conditions (atrial fibrillation/flutter, ventricular tachycardia/fibrillation, sinus bradycardia/tachycardia, wound infections, poor urine output, and post-operative bleeding). Recommended: 1. Insertion of internal jugular, subclavian, and femoral central venous catheters; insertion of radial and femoral arterial lines in the ICU with supervision. 2. Perform VATS wedge resection/biopsy as primary surgeon. 3. Perform VATS pleural biopsy as primary surgeon. 4. Perform VATS talc pleurodesis and/or PleurX catheter placement as primary surgeon. (4) Professionalism 1. The ability to be honest, reliable and respectful of the religious, racial and gender characteristics of patients, their families and other members of the health care team. 2. The ability to give and receive advice in a manner that is consistent with the harmonious operation of a health care team. 3. The ability to recognize when to seek assistance from more experienced colleagues. 4. Deliver highest quality care with ethics, integrity, honesty and compassion. 5. Exhibit appropriate personal and interpersonal professional behaviors. 6. Understand the professional, legal and ethical codes to which physicians are bound. (5) Interpersonal and Communication Skills 1. 2. 3. 4. 5. 6. 7. 8. Listen effectively. Establish therapeutic relationship with patients and families. Obtain and synthesize relevant history from patients and family. Inform patients and families about their condition at an appropriate and understandable level. Write clear consultation notes, progress notes, discharge summaries, and clinic notes. Prepare and present ward rounds in an organized manner. Participate actively in scheduled rounds. Communicate effectively with allied health care professionals. (6) Systems-based Practice 1. Utilize resources effectively to balance patient care, learning needs and outside activities. 2. Allocate finite health care resources wisely. 3. Work effectively and efficiently in a health care organization. 4. Understand the importance of and mechanisms to safely utilize resources in a cost-effective manner to benefit all patients. 5. Recommend practices to effectively utilize resources including undertaking studies to assess effectiveness of standard care procedures. (7) Practice-Based Learning and Improvement 1. Develop effective self-directed learning strategies for continuing education and assessment of knowledge base. 2. Critically appraise sources of medical information and be aware of resources available. 3. Prepare and present scheduled rounds. 4. When possible, participate actively in scheduled morbidity and mortality conferences. 5. Actively participate in journal club. 6. Participate effectively in facilitate learning of patients, teaching house staff/students and other health professionals. Method of assessment of resident academic performance 1. Bi-yearly general competencies evaluation on Stanford Medhub. 2. Yearly in-service training exam. 3. Bi-yearly 360 degree evaluation (nurse and patient). GOALS AND OBJECTIVES FOR R2 CARDIOTHORACIC SURGERY RESIDENT ON PAVA CARDIOTHORACIC SURGERY SERVICE Description: Residents will spend two months on this service, becoming proficient in the indications, workup, and postoperative care of common cardiac and thoracic conditions. The resident will learn to manage ICU patients, including placement of chest tubes, central lines, PA catheters, and IABPs. Residents will learn basic surgical and endoscopic skills, including saphenous vein harvest, wound closure, bronchoscopy/endoscopy, and handling of vascular tissues. Finally, residents will have the opportunity to practice cardiac procedures and situations in the Cardiac Surgery Simulations Laboratory. (1) Medical Knowledge 1. Anatomy, embryology, physiology and pathology of the pericardium, heart, great vessels, trachea, lungs, esophagus, and mediastinum. 2. The pharmacology, indications, and complications of drugs commonly used in the specialty. 3. The principles of preoperative assessment, anesthetic management, and postoperative management of cardiothoracic surgical patients. 4. The natural history of treated and untreated cardiac surgical conditions, including ischemic heart disease and its complications, valvular heart disease, thoracic aortic disease, conduction system disturbances, and pericardial disease. 5. The natural history of treated and untreated thoracic surgical conditions, including lung cancer (primary and metastatic), esophageal cancer, esophageal dysmotility disorders, pleural effusions/empyemas, lung abscess, TB, emphysema, and pneumothorax. 6. Advanced principles of surgery as they apply to the specialty, such as wound healing, hemostasis, electrolytes/fluid management, surgical nutrition, hyperalimentation, and oncology. 7. The technology, interpretation and complications of invasive and noninvasive diagnostic methods, including CT and MRI scanning, cardiac catheterization, coronary angiography, respiratory function tests, PET scan, and echocardiography. 8. The physiology, technology, indications, and complications of cardiac pacemakers and defibrillators. 9. Introduction to principles and complications of extracorporeal circulation and myocardial protection. (2) Clinical Skills 1. Perform an appropriate relevant history and physical exam in the ward, ambulatory, and emergency department settings. 2. Arrive at an appropriate differential diagnosis. 3. Order appropriate laboratory, radiological, and other diagnostic procedures; demonstrate proper interpretation of the results. 4. Formulate a plan of management, demonstrating knowledge in the operative and non-operative management of the disease process. 5. Manage the patient throughout the hospital stay, including management in an intensive care unit setting, demonstrating knowledge and ability to anticipate, recognize, and manage potential complications of the disease processes and operative procedures. 6. Provide a plan for patient follow up. 7. Management of post-operative bleeding (medical and surgical). 8. Management of low-cardiac output syndrome (medical and surgical). 9. Troubleshooting pacemakers. 10. Assessment and treatment of post-operative arrhythmias. 11. Identification of critically ill and major complications of patients on the ward with appropriate acute management. (3) Patient Care Expected: 1. As the operating surgeon or first assistant, demonstrate an ability to anticipate surgical maneuvers, to take direction well, to make reasonable suggestions, and to contribute to a positive operating room atmosphere. 2. Remove the long saphenous vein, with attending supervision. 3. Insertion of central lines, PA catheter, arterial lines, insertion/removal chest tubes, and thoracentesis in the operative and ICU setting. 4. As the operating surgeon, perform flexible bronchoscopy, demonstrating knowledge of lobar segmental anatomy. 5. Observe common cardiac and thoracic surgical procedures, including CABG, aortic valve replacement, mitral valve replacement, lobectomy, esophagectomy, VATS lung wedge resection/biopsy. 6. Demonstrate ability to recognize errors in technique and possible consequences of specific technical mistakes. Recommended: 1. Removal of intraaortic balloon pump. 2. Exposure of femoral vessels for CPB. 3. As the operating surgeon, perform posterior lateral thoracotomy. 4. As the operating surgeon, perform VATS lung wedge resection/biopsy. (4) Professionalism 1. The ability to be honest, reliable, and respectful of the religious, racial and gender characteristics of patients, their families and other members of the health care team. 2. The ability to give and receive advice in a manner that is consistent with the harmonious operation of a health care team. 3. The ability to recognize when to seek assistance from more experienced colleagues. 4. Deliver highest quality care with ethics, integrity, honesty, and compassion. 5. Exhibit appropriate personal and interpersonal professional behaviors. 6. Understand the professional, legal, and ethical codes to which physicians are bound. (5) Interpersonal and Communication Skills 1. 2. 3. 4. 5. 6. 7. 8. Listen effectively. Establish therapeutic relationship with patients and families. Obtain and synthesize relevant history from patients and family. Inform patients and families about their condition at an appropriate and understandable level. Write clear consultation notes, progress notes, discharge summaries, and clinic notes. Prepare and present ward rounds in an organized manner. Participate actively in scheduled rounds. Communicate effectively with allied health care professionals. (6) Systems-based Practice 1. 2. 3. 4. Utilize resources effectively to balance patient care and learning needs. Allocate finite health care resources wisely. Work effectively and efficiently in a health care organization. Understand the importance and mechanisms to safely utilize resources in a costeffective manner to benefit all patients. 5. Recommend practices to effectively utilize resources including undertaking studies to assess effectiveness of standard care procedures. (8) Practice-Based Learning and Improvement 1. Develop effective self-directed learning strategies for continuing education and assessment of knowledge base. 2. Critically appraise sources of medical information and be aware of resources available. 3. Read around clinical cases. 4. Prepare and present scheduled rounds. 5. Participate actively in scheduled morbidity and mortality conferences. 6. Actively participate in journal club. 7. Participate effectively in facilitate learning of patients, teaching house staff/students and other health professionals. Method of assessment of resident academic performance 1. Bi-yearly general competencies evaluation on Stanford Medhub. 2. Yearly in-service training exam. 3. Bi-yearly 360 degree evaluation (nurse and patient).