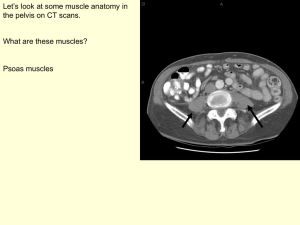
Anterior Abdominal Wall and Inguinal Canal Learning Objectives – 1
advertisement

© 2009 Mark Tuttle Anterior Abdominal Wall and Inguinal Canal Learning Objectives – 1/5/09 [LANE] 1. Define the boundaries of the abdominal cavity and the skeletal components related to the abdominal wall. a. Boundaries: i. Superior: Diaphragm ii. Anterior: Aponeuroses iii. Inferior: Superior pelvic aperture (imaginary) iv. Posterior: Anterior longitudinal ligament of vertebral bodies b. Skeletal components i. Lumbar vertebrae ii. Lower ribs iii. Pubic bones 1. Iliac crest 2. Describe the major surface landmarks of the anterior abdominal wall. a. Linea semilunaris: On the lateral side of each rectus abdominus muscle b. Umbilicus: Remnant of the umbilical cord c. Linea alba: “happy trail.” Medially between rectus abdominal mm. 3. Describe the lines and planes that are used to divide the abdomen into quadrants and regions. a. Quadrants i. Dividers 1. Transumbilical plane (TUP) a. IV disk L3/L4 2. Median plane (follows linea alba) ii. Regions (4) 1. Right upper quadrant (RUQ) 2. Left upper quadrant (LUQ) 3. Right lower quadrant (RLQ) 4. Left lower quadrant (LLQ) b. Regions i. Dividers 1. Mid-clavicular lines (2): Middle of clavicle down 2. Subcostal plane: Tangent to lowest ribs (L2) 3. Transtubercular plane: Midway between the upper transverse and the upper border of the symphysis pubis. Between iliac tubercles. (L5) ii. Regions (9) 1. Epigastric 2. Right/Left hypochondriac 3. Umbilical 4. Right/Left lumbar 5. Hypogastric 6. Right/left inguial c. Other planes i. Transpyloric: L1, just above subcostal at L2 ii. Interspinous plane: Connects right/left ASIS, just above transtubercular © 2009 Mark Tuttle 4. Describe the attachments, orientations, relative positions, actions, and fascia of the four major abdominal muscles. a. External oblique i. Attachment 1. 5th-12th ribs, inferiorly 2. (Linea alba) 3. Pubic tubercle 4. Anterior ½ of iliac crest. “jumps across” inguinal ligament ii. Orientation 1. Like a “V”, or “hands in pockets” iii. Relative position 1. Superior lateral, membranous tendon inferior medial iv. Action 1. Compress abdominal contents v. Innervation 1. Ventral rami T7-T12 (Thoracoabdominal nn.) +/- L1 vi. Fascia 1. Superficial: a. Camper’s: Fatty (superficial) layer of superficial fascia b. Scarpa’s: Membranous (deep) layer of superficial fascia c. Deep fascia 2. Deep: a. Deep fascia b. Internal oblique i. Attachment 1. Thoracolumbar fascia 2. Anterior 2/3 of iliac crest 3. Inginal ligament (lateral ½) 4. Lower ribs ii. Orientation 1. Upside-down “V” iii. Relative position 1. Inferior lateral, membranous tendon superior medial iv. Action 1. Unilateral: same side rotation/bending v. Innervation 1. Ventral rami T7-T12 (Thoracoabdominal nn.) +/- L1 vi. Fascia 1. Superficial/Deep: Deep fascia c. Transverse oblique i. Attachment 1. Ribs/costal muscle 2. Thoracolumbar fascia 3. Iliac crest 4. Lateral 1/3 of inguinal ligament a. Important b/c it does NOT contribute a layer to the spermatic cord ii. Orientation © 2009 Mark Tuttle 1. Horizontal iii. Relative position 1. Lateral, membranous medial iv. Action 1. Raise abdominal pressure v. Innervation 1. Ventral rami T7-T12 (Thoracoabdominal nn.) +/- L1 vi. Fascia 1. Superficial: Deep 2. Deep: Transversalis fascia d. Rectus Abdominus i. Attachment 1. Costal cartilage of ribs 5-7 2. Xyphoid process 3. Pubic crest ii. Orientation 1. Vertical iii. Relative position 1. Segmented, with 4 sets of membranous aponeurosess iv. Action 1. Flexes trunk, compresses abdomen v. Innervation 1. Ventral rami T7-T12 (Thoracoabdominal nn.) +/- L1 vi. Fascia 1. Above arcuate line: a. Superficial/Deep: Internal oblique aponeurosis 2. At/below arcuate line: a. Superficial: All abdominal aponeuroses b. Deep: Perietal peritoneum 5. Define the blood supply, nerve supply, fascial layers, muscle layers, extraperitoneal fat, and parietal peritoneum of the anterior abdominal wall. How do these relate to the various surgical approaches to the abdominal cavity? a. Blood supply i. Superior 1. Internal thoracic a. a. Musculophrenic a. branches laterally along subcostal angle b. Superior epigastric a. branches medially along rectal sheath ii. Inferior 1. External Iliac a. a. Inferior epigastric a. branches superior medial. Supplies more of rectus abdominus than superior epigastric because it is deep. b. Deep circumflex iliac a. branches superior medial c. Femoral a. continuation inferior to inguinal ligament i. Superficial epigastric a. branches superior medial © 2009 Mark Tuttle ii. Superficial circumflex iliac a. branches superior lateral along iliac crest superficially iii. Lateral 1. Intercostal aa. Even those of false ribs 2. Subcostal a. b. Nerve supply i. Pathway: 1. Between internal oblique mm. and transverse abdominis mm., pierce the rectus sheath to supply rectus ab. Mm. + provide anterior cutaneous branches ii. Thoracoabdominal nn. (T7-T11) 1. Cutaneous innervation separately of medial/lateral portions iii. Iliohypogastric n. (L1) supplies mons pubis iv. Ilioinguinal n. (L1) supplies scrotum/labia majora v. T10 supplies of umbilicus vi. T5 supplies skin over xyphoid process c. Surgical approaches i. General goals 1. Try not to transect arteries/nerves 2. Use “Gridiron technique” in appendix surgery with McBurney’s point ii. Landmarks 1. Subcostal: outdated way for spleen surgery 2. Median: linea alba 3. Paramedian: just lateral to linea alba 4. Super pubic: just above mons pubis, used in C-sections 5. McBurney’s point a. Line between ASIS and umbilicus b. 1/3 of the way from ASIS to umbilicus c. Used for appendix surgery 6. Describe the configuration of the anterior and posterior walls of the rectus sheath superior and inferior to the arcuate line. a. Superior to the arcuate line, the internal oblique aponeurosis surrounds the abdominus rectus b. Inferior to the arcuate line, the internal oblique aponeurosis is only superficial to the abdominus rectus since it pierces it 7. Define the inguinal canal, including the location of the deep and superficial inguinal rings. a. Know the structures forming the walls of the inguinal canal. i. Superficial inguinal ring 1. Medial Crus 2. Lateral Crus 3. Intercrural fibers (not very pronounced in most cadavers) ii. Borders: 1. Anterior: External oblique 2. Posterior: Internal oblique/conjoint tendon 3. Superior: Internal oblique 4. Inferior: Inguinal ligament © 2009 Mark Tuttle b. Define the function and mechanics of the inguinal canal. i. Route of passage for the testes from posterior abdominal wall to scrotum ii. Contains the spermatic cord in males and the round ligament in females c. Describe the contents of the inguinal canal. How do these differ between the sexes? i. Males: spermatic cord, (gubernaculums) ii. Females: round ligament d. Describe the borders of the inguinal triangle (Hasselbach’s Triangle). i. rectus abdominis muscle (medially) ii. inguinal ligament (inferiorly) iii. inferior epigastric vessels (superior and laterally). 8. Define the anatomy and relationships of the: a. Process vaginalis i. Portion of peritoneal cavity that “follows” the testes as they descent. Normally is obliterated, but can be patent in adults. b. Spermatic cord i. Fascia layers 1. External spermatic fascia 2. Cremasteric fascia 3. Internal spermatic fascia (continuous with transversalis fascia) ii. Contents 1. Ductus (Vas) deferens 2. Testicular arvery, artery of Vas 3. Pampiniform plexus of veins a. Helps cool temperature in testicles 4. Lymph vessels 5. Nerves c. Epididymus i. Narrow, tightly-coiled tube connecting the efferent ducts from the rear of each testicle to its vas deferens. ii. Storage of sperm d. Cremaster muscle i. Originates from the internal oblique ii. Surrounds the testes iii. Helps regulate testes temperature to optimal for spermatogenesis e. Testes i. Site of spermatogenesis ii. Consist of seminiferous tubules f. Scrotum i. Surrounds the testes ii. Layers 1. Skin 2. Tunica dartos Dartos fascia/muscle a. Colles’ fascia and dartos m. (smooth m.) 3. External spermatic fascia External oblique 4. Cremaster muscle/fascia Internal oblique 5. Internal spermatic fascia Transversalis fascia © 2009 Mark Tuttle 6. Tunica vaginalis (parietal/visceral) Peritoneum 9. Describe the coverings of the spermatic cord and their role in the descent of the testes during development. How do these layers relate to the coverings of the scrotum? a. Many of the layers of the testes are continuous with analagous layers in the spermatic cord. However, the tunica vaginalis of the scrotum is a remnant of the peritoneum which is sealed off from the testes in normal adults 10. Chart the blood supply and lymphatic drainage of the testis. How do they differ from that of the scrotum? a. Testes i. Blood: Testicular arteries ii. Lymphatic: Inguinal Nodes b. Scrotum i. Blood: Anterior/posterior scrotal arteries ii. Lymphatic: Deep lumbar nodes 11. What is an inguinal hernia? What features distinguish a direct from an indirect inguinal hernia? a. Direct i. Through the inguinal triangle ii. Transversalis fascia forms hernia sac iii. Occurs medially to epigastric artery iv. Less common than indirect hernias b. Indirect i. Through the deep/superficial inguinal rings ii. Covered by all three layers of spermatic cord iii. Remains of the process vaginalis forms the hernia sac iv. 20x more common in males than females v. More common in younger people © 2009 Mark Tuttle Peritoneum and Major Vessels -1/6/2009 [LANE] 1. Define the peritoneum and peritoneal cavity. a. Peritoneum i. Large, thin, transparent sheet of serous membrane which lines the walls of the abdominopelvic cavity and is reflected onto the viscera b. Peritoneal cavity i. Potential space between adjacent layers of peritoneum usually containing a small amount of fluid 2. Understand what distinguishes parietal from visceral peritoneum. a. Parietal peritoneum lines the abdominal and pelvic walls b. Visceral peritoneum covers abdominal and pelvic organs 3. Describe the shape and extent of the peritoneal cavity a. 4. Know what the borders of the greater and lesser sac are. a. Lesser sac borders i. Anterior 1. Lesser omentum 2. gastrocolic ligament ii. Inferior 1. Trasverse mesocolon iii. Superior 1. Caudate lobe of liver iv. Posterior 1. Pancreas 2. Aorta 3. Celiac trunk 4. Splenic a. and v. 5. Gastrosplenic fold 6. Left suprarenal gland 7. Left kidney v. Right 1. Liver 2. Duodenal bulb vi. Left 1. Spleen 2. Gastrosplenic ligament b. Greater sac borders i. Everything else within the peritoneum 5. Describe the components of the greater and lesser omentums. a. Greater Omentum i. Attaches the stomach (along the greater curvature) to the posterior abdominal wall. ii. Subdivided into 3 ligaments: (PCS) 1. Gastrophrenic 2. Gastrosplenic 3. Gastrocolic b. Lesser Omentum i. Attaches the stomach (along the lesser curvature) to the liver. © 2009 Mark Tuttle ii. Subdivided into 2 ligaments: 1. Hepatogastric 2. Hepatoduodenal 6. Know what forms the borders of the epiploic foramen. What spaces does it connect? a. It connects the greater and lesser sacs b. Also known as the Foramen of Winslow c. Borders: i. Anterior 1. Hepatoduodenal ligament ii. Posterior 1. Peritoneum covering the inferior vena cava iii. Superior 1. Peritoneum covering the caudate lobe of the liver iv. Inferior 1. Peritoneum covering the duodenum/proper hepatic a. 7. Know what organs and structures within the abdomen are intraperitoneal (peritoneal) and which are primarily and secondarily retroperitoneal? a. Primarily retroperitoneal i. Esophagus ii. Suprarenal glands iii. Kidneys iv. Rectum b. Secondarily retroperitoneal i. Pancreas ii. Duodenum (except for superior portion) iii. Ascending colon iv. Descending colon c. Intraperitoneal i. Everything else 8. Be able to describe and give examples of peritoneal pouches, folds, recesses and gutters. a. Folds i. Lateral umbilical fold (2) (inferior epigastric) ii. Medial umbilical fold (2) (obliterated umbilical a.) iii. Median umbilical fold (1) (urachus) b. Recesses i. Subphrenic recess 1. Between liver and diaphragm ii. Superior recess of omental bursa 1. Posterior part of liver 2. Part of the lesser sac 3. Borders the greater sac via the coronary ligaments iii. Inferior recess of omental bursa 1. Between stomach and transverse colon c. Pouches (pouch of peritoneum formed by peritoneal folds or ligaments) i. Rectovesical pouch 1. Everything eventually drains here ii. Hepatorenal pouch © 2009 Mark Tuttle 9. 10. 11. 12. d. Gutters i. Right paracolic gutter ii. Left paracolic gutter e. Spaces i. Supracolic compartment ii. Infracolic compartment iii. Right infracolic space 1. Leaks can stay localized here for a while 2. Bordered by mesentery iv. Left infracolic space Distinguish between mesentery, mesocolon, greater omentum, lesser omentum and the various peritoneal ligaments. a. Mesocolon i. Transverse + Sigmoid sections of colon that are intraperitoneal b. Greater omentum i. Hangs down from front of stomach ii. Gastrophrenic + gastrosplenic + gastrocolic ligaments c. Lesser omentum i. Between stomach and liver ii. Hepatogastric + hepatoduodenal ligaments Describe the causes and relations of the peritoneal reflections located on the anterior abdominal wall. a. Lateral umbilical folds (L + R) i. Houses the inferior epigastric artery b. Medial umbilical folds (L + R) i. Houses the obliterated umbilical artery c. Median umbilical fold i. Houses remnant of urachus, an embryological canal connecting the urinary bladder of the fetus with the allantois List the three unpaired branches of the abdominal aorta. Know the terminal branches of these main arteries. a. Splenic a. i. Short gastric aa. ii. Left gastro-omental a. (gastropiploic) (on the greater curvature) iii. Pancreatic a. iv. Posterior gastric a. (60-80% of people) b. Proper hepatic a. i. Right gastric a. ii. Left hepatic a. iii. Right hepatic a. iv. Cystic a. c. Gastroduodenal a. i. Supraduodenal a. ii. Superior pancreatocoduodenal a. iii. Right gastro-omental a. (gastroepiploic) (on the greature curvature) Describe the venous drainage from the abdominal viscera. What is the hepatic portal system? © 2009 Mark Tuttle a. Begins at the venous ends of capillaries in the organs of the GI tract and ends at the venous sinusoids in the liver b. Formed bythe joining of the plenic vein with the superior mesenteric vein c. Inferior mesenteric vein usually joins the splenic vein d. NO VALVES in portal vein 13. What is a portal-systemic anastomoses? Where do four major portal-systemic anastomosis occur in the body and what is the clinical significance of varicosities at these sites a. Esophageal varices i. Portal: Esophageal branch of left gastric v. ii. Systemic: Esophageal branch to Azygous v. b. Anorectal varices i. Portal: Superior rectal branch of inferior mesenteric v. ii. Systemic: Middle and inferior rectal to internal iliac v. c. Caput medusa i. Portal: Paraumbilical (in falciform ligament) branch of portal ii. Systemic: Superior and inferior epigastric vv. d. Retroperitoneal varices (Veins of Retzius) i. Portal: Colic, duodenal, and pancreatic vv. ii. Systemic: Lumbar and renal vv. to inferior vena cava © 2009 Mark Tuttle GI Tract and Associated Organs - Lane 1. Abdominal part of esophagus a. Comes through the diaphragm at T8 2. Stomach: a. Cardiac and pylorus orifices i. Cardiac orifice is at the top of the stomach at the gastroesophageal junction in the cardia region ii. There are no chief cells in the cardiac region iii. The pyloric orifice lies at the distal part of the stomach, part of the gastric sphincter b. Relation with greater and lesser omentum i. The greater omentum takes its origin along the greater curvature of the stomach 1. Attaches the stomach to the posterior abdominal wall 2. Composed of Gastrophrenic, gastrosplenic, and gastrocolic ligaments ii. The lesser omentum takes origin along the lesser curvature of the stomach and attaches to the liver 1. Composed of hepatogastric and hepatoduodenal ligaments c. Anterior and posterior surfaces i. On the posterior surface of the stomach runs the splenic artery off of the celiac trunk and in 60-80% of people d. Fundus and cardinal notch i. Fundus is the most superior part of the stomach. It ascends above the gastricesophageal junction. Usually there is an air bubble here. ii. The cardial notch is the region immediately superior to the gastroesophageal junction e. Body and angular incisures i. The body of the stomach is below the Cardia and the Fundus ii. The angular incisures divides the body from the pyloric antrum, it is clearly evident in a deflated stomach f. Pyloric antrum i. Distal to the gastric body is the pyloric antrum g. Pylorus, pyloric sphincter, pyloric canal i. The pyloric canal is a narrowing of the stomach approaching the pyloric sphicter h. Mucous membrane appearance, gastric folds (rugae) i. Rugae are oriented in the direction of flow i. Muscles of stomach wall i. 3 layers whereas the rest of the GI is only 2 ii. Oblique, circular, longitudinal j. Describe relations of stomach with adjacent structures. i. Right side: spleen ii. Above: diaphragm and liver iii. Left: liver iv. Behind: pancreas v. Below: transverse colon k. Describe the blood supply of the stomach. © 2009 Mark Tuttle i. The stomach is supplied by the right and left gastric arteries, (posterior gastric artery), and by the right and left gastro-omental arteries 3. Small Intestine: a. Identify and distinguish the 3 major divisions of the small intestine: Duodenum, Jejunum, and Ilium. Note the major and minor doudenal papillae i. The duodemum is the most proximal part of the intestine, connecting to the stomach. ii. The duodenum’s transition to jejunum occurs at the suspensetory ligament of the duodenum (Ligament of Treitz) iii. There is no clearly defined border between the jejunum and the ileum, but you can tell the difference between the two regions based on structure iv. Jejunum 1. Thicker wall 2. Smaller number of arcardes, longer vasa recta, poorer anastomoses 3. Less fat 4. Numerous plicae 5. Few Peyer’s patches v. Ileum 1. Thinner wall 2. Larger number of arcades, shorter vasa recta, better anastomoses 3. More fat 4. Poorly defined plicae 5. Many Peyer’s Patches b. Describe their locations and relationships to other abdominal structures including mesenteries and peritoneum. i. Superior mesenteric artery supplies the entire small intestine as well as the cecum (ileocolic), ascending colon (ileocolic), and transverse colon (middle colic) ii. The inferior mesenteric artery supplies the descending colon (left colic), the sigmoid colon (sigmoid), and the rectum (superior rectal) iii. The transverse colon, sigmoid colon, and cecum are intraperitoneal, but ascending, descending, are retroperitoneal (secondarily) c. Describe the blood supply of the small intestine, note the distinct features of jejunal and ileal vessel arcades and vasa recta. i. See above. ii. The jejunum has longer vasa recta but a smaller number of arcades than the ileum 4. Large Intestine: a. Identify the various parts including the appendix, their location and relationships to other abdominal structures including mesenteries and peritoneum. i. Ascending and descending colon are retroperitoneal (secondarily) ii. Cecum, transverse colon, and sigmoid colon are intraperitoneal iii. The rectum is retroperitoneal b. Describe the blood supply of the large intestine. © 2009 Mark Tuttle i. See above, 3b c. Identify the appendix and its relationships. i. Retrocecal (64%): posterior to the cecum ii. Subcecal (<1%): just below the cecum iii. Pelvic (32%): sticking into the pelvis iv. Preileal (<1%): Anterior to the distal-most part of the ileum v. Postileal (<1%): Posterior to the distal-most part of the ileum d. Describe the teniae coli, omental appendices, haustra, semilunar folds. i. Teniae coli: 1. Smooth muscle bands 2. 3 layers which correspond to muscularis externa in GI 3. Mesocolic, free, and omental ii. Omental appendices 1. little processes or sacs of peritoneum filled with adipose tissue and projecting from the serous coat of the large intestine, except the rectum; they are most evident on the transverse and sigmoid colon, being most numerous along the free tenia. iii. Haustra 1. Small pouches caused by sacculation, which give the colon its segmented appearance. The taenia coli runs the length of the large intestine. Because the taenia coli is shorter than the intestine, the colon becomes sacculated between the taenia, forming the haustra. In between adjacent haustra are semilunar folds, known as the plicae semilunares. 2. Haustral contractions are slow segmenting movements that occur every 25 minutes. One haustrum distends as it fills, which stimulates muscles to contract, pushing the contents to the next haustrum. iv. Semilunar folds 1. See above e. Understand the location and relations of the colic flexures. i. Right colic flexure (hepatic) (hepatocolic ligament?) ii. Left colic flexure (phrenicocolic ligament) ACCESSORY ORGANS OF THE GASTROINTESTINAL TRACT 5. Liver: a. Define its major function. i. Stores glycogen, secretes bile b. Describe the anatomical and functional lobes of the liver. i. Anatomical 1. Right + left lobes 2. Caudate 3. Quadrate ii. Functional 1. The central area where the common bile duct, hepatic portal vein, and hepatic artery proper enter is the hilum or "porta hepatis". The duct, vein, and artery divide into left and right branches, and the portions of the liver supplied by these branches constitute the functional left and right lobes. © 2009 Mark Tuttle c. Define the relations of the liver to other abdominal structures. i. The liver is on the right side and is adjacent to the stomach ii. Just beneath the liver is the right kidney d. Describe the porta hepatis and its contents. i. On the posterior side of the liver ii. Contains the transmits the hepatic portal vein, the hepatic artery proper, the common hepatic duct, nerves and lymphatics e. Describe the peritoneal ligaments and the bile ducts associated with the liver. i. L + R triangular ligaments ii. Anterior + Posterior coronary ligaments iii. Falciclorm ligament iv. Ligament of teres (remnant of ombilical v.) f. Describe the blood supply of the liver. i. Portal vein (75%) ii. Hepatic aa. (25%) 6. Gall Bladder: a. Describe its location, parts, relationships, functions, and the bile duct system. i. Neck, body, fundus ii. NOT a gland, only a storage reservoir iii. Intimately invested in the liver iv. Spiral Valves of Heister: undulating folds or valves in the proximal mucosa of the cystic duct v. Bile duct dumps bile into the Major Duodenal Papilla (Ampula of Vater) 7. Pancreas: a. Describe its location, relationships, functions and the pancreatic duct system. i. Secondarily retroperitoneal ii. Has exocrine (pancreatic enzymes) and endocrine functions (insulin/glucagon) b. Define its parts. i. Head ii. Uncinate process 1. Formed from the ventral pancreatic bud iii. Neck iv. Body v. Tail c. Describe its blood supply. i. Superior pancreatoduodenal a. branches off of the gastroduodenal artery ii. Inferior pancreatoduodenal a. branching off of the superior mesenteric a. iii. Splenic artery 8. Spleen: a. Describe its location, relationships, and functions. i. Just lateral to the stomach, closely related to the diaphragm ii. Centered at approximately the 9th rib on the left side iii. Secured by the gastrosplenic and splenorenal ligaments iv. Filters blood, removes old blood cells + foreign material v. Protected by a delicate, thin capsule © 2009 Mark Tuttle vi. Is the most frequently injured organ in the abdomen b. Describe its blood supply. i. Highly vascular ii. Supplied by the splenic artery branch of the Celiac Trunk © 2009 Mark Tuttle Development of the GI System 1 - Lane 1. List the three major regions of the embryonic gut and define the boundaries (limits) of each in terms of embryonic structures and definitive structures. a. Foregut b. Midgut c. Hindgut DIGESTIVE SYSTEM - FOREGUT 2. List the structures derived from the foregut. What is the blood supply of the structures derived from the caudal portion of the foregut? a. Structures i. Esophagus and stomach ii. Pharynx + lower respiratory system iii. Duodenum (distal to opening of bile duct) iv. Liver v. Billiary apparatus vi. Pancreas b. The GI structures are supplied by the Celiac Trunk 3. What are the germ layers of origin for the epithelial structures derived from the foregut; the smooth muscle and connective tissue; vascular supply; nerve supply? a. Endoderm forms the lining of the GI b. Mesoderm forms the connective tissue and blood vessels for the GI c. (Neural crest ?) forms the nerves of the GI 4. Describe the development of the dorsal and ventral mesenteries and the formation of lesser sac. a. Ventral mesentery (Degenerates almost entirely) i. Lesser omentum ii. Falciform ligament iii. Coronary/triangular ligaments b. Dorsal mesentery i. Greater omentum ii. Splenorenal ligament iii. gastrocolic ligaments c. Formation of Lesser Sac i. Isolated clefts develop in the mesenchyme forming the thick dorsal mesogastrium. The clefts soon coalesce to form a single cavity, the omental bursa ii. Rotation of the stomach pulls the dorsal mesogastrium to the left, thereby enlarging the bursa iii. The bursa expands transversely and cranially and soon lies between the stomach and the posterior abdominal wall iv. Dorsal mesogastrium continued inferior elongation forms the greater omentum v. Facilitates movements of the stomach 5. Describe the development of the esophagus, stomach and duodenum. What results from the rotation of the stomach? What developmental anomalies are associated with each? a. Esophagus © 2009 Mark Tuttle i. Initially short but elongates quickly ii. Endoderm proliferates so much that the lumen is obliterated for a while, then recanulates iii. Striated muscle of the muscularis externa of the upper 1/3 is derived from mesenchyme of the caudal pharyngeal arches iv. Smooth muscle of the lower 1/3 of the esophagus is derived from the splanchnic mesenchyme b. Stomach i. Starts as a dorsal enlargement of the caudal part of the foregut during the 4th week ii. Differential growth leads to the formation of the greater/lesser curvatures iii. Slowly rotates clockwise 90 degrees, causing the greater curvature to become positioned on the lft side of the stomach c. Duodenum i. Begins to form during the 4th week at the caudal end of the foregut and the cranial end of the midgut ii. Develops a C-shape oriented anterior-posteriorly iii. The C rotates clockwise with the stomach iv. The endoderm of the duodenum proliferates so much that the lumen is oblitered for a while, then recanulates by week 8 (end of the embryonic period) v. Marks the transition between foregut and midgut 6. List the derivatives of the hepatic diverticulum. a. Liver b. Gallbladder c. Billiary apparatus 7. Describe the formation of the liver within the substance of the septum transversum. a. Reflections of the ventral mesentery on to the diaphragm become the coronary and triangular ligaments that surround the bare area of the liver b. Proliferating endodermal cells form cords of hepatic cells and the epithelia cells of the billiary system within the liver c. Hepatic cords anastomose around the endothelium lined spaces that are forming the hepatic sinusoids d. The CT, endothelial cells, hemopoietic tissue and kupffer cells arise form the splanchnic mesenchyme of the ventral mesentery e. Hematopoeisis begins in the liver around week 6. Bile formation begins around week 12 f. Liver represents 10% of the body wight by week 10 g. Gall bladder and cy stic duct forms from the small caudal part of the hepatic diverticulum h. Extrahepatic biliary apparatus is initially solid cords of epithelial cells but later canalized i. Initially the bile duct is attached to the ventral surface of the duodenal loop but rotate nof the duodenum moves it to the posterior surface j. Bile entering the duodenum after the 13th week gives the meconuum a dark green color © 2009 Mark Tuttle 8. Describe the pancreatic buds and their positional changes involved in the formation of the adult pancreas, especially the formation of the definitive biliary and pancreatic duct system as well as related developmental anomolies . a. Dorsal bud: neck, body, tail, most of head b. Ventral bud: part of head, uncinate process c. Endodermal cells form both the exocrine and endocrine pancreatic tissues d. Splanchnic mesenchyme forms the CT elements of the pancreas 9. Define the terms: stenosis, atresia, hernias, polyhydramnios. a. Stenosis: hardening, narrowing of a lumen b. Atresia: hypoplastic, too small/short c. Polyhydramnios: too much amniotic fluid because the fetus is not processing it 10. Describe the development of the spleen in the dorsal mesogastrium. a. No endoderm in spleen b. Arises from DORSAL mesogastrium c. Differentiate to form the capsule, connective tissue, and parenchyma of the spleen d. Begins to develop at week 5 and is initially lobulated Development of the GI System 2 - Lane DIGESTIVE SYSTEM - MIDGUT 1. List the adult structures derived from the midgut. a. Midgut starts DISTAL to the major duodenal papilla b. Distal duodenum c. Jejunu d. Ileum e. large intestine up to and including the proximal 2/3 of the transverse colon f. appendix 2. What is the blood supply and autonomic innervation pattern of the structures formed from the embryonic midgut? a. All derivatives are supplied by the superior mesenteric artery 3. Describe the positional changes that take place during the process of midgut rotation and fixation. a. Rotation i. Herniation 1. By week 6, the midgut elongation nexceeds the capacity of the peritoneal cavity (intraembryonic coelom). This produces a physiological umbilical herniation into the umbilical cord 2. While it is in the umbilical cord, the midgut loop rotates 90 degrees counterclockwise around the axis of the superior mesenteric artery. 3. This brings the cranial limb (small intestine) of the midgut loop to the right and the caudal limb (large intestine) to the left. 4. During rotation, the cranial limb elongates and forms intestinal loops (primordial of jejunum and ileum) ii. Reversal of herniation 1. During the 10th week the intestines return to the abdomen (reduction of the midgut hernia) 2. Small intestine returns first, passing posterior to the superior mesenteric artery and occupies the central part of the abdomen © 2009 Mark Tuttle 3. As the large intestine returns, it undergoes a further 180 degree counterclockwise rotation 4. Later it comes to occupy the right side of the abdomen 5. The ascending colon becomes recognizable as the posterior abdominal wall elongates. b. Fixation i. Results in ascending/descending colon & duodenum being retroperitoneal ii. The enlarged colon presses the duodenum and pancreas against the posterior abdominal wall c. What developmental abnormalities are associated with these processes? i. Malrotation of the midgut 1. Nonrotation of gut (Left side colon) a. 180 degree rotation ndoes not occur b. Colon entirely on the left, small intestine on the right (called left-side colon) 2. Mixed rotation a. Cecum located near pyloris of stomach b. CT bands stretch over/compress duodenum c. Occurs w/volvulus of intestine 3. Reverse rotation (only really a problem if incomplete) a. Colon located posterior to duodenum + superior mesenteric artery b. Superior mesenteric artery is compressed as a result 4. Subhepatic cecum + appendix a. Only a problem if inflated appendix. Often misdiagnosed as gallbladder problem b. Cecum fails to descend, fixes to liver 5. Internal Hernia a. Intestines push into mesentery + creates pocket 6. Mobile cecum a. Most common anomaly (10% of population) b. Problem because it can lead to volvulus (increased risk) ii. Omphalocele 1. Failure of a portion of the intestines to return to the abdominal cavity 2. Stays in umbilical cord 3. Covered by epithelium of umbilical cord iii. Gastroschisis 1. Failure in formation of anterior abdominal wall 2. Due to a defect of lateral folds in week 4 when lateral wall folds are formed 3. Nothing covers herniation iv. Umbilical hernia 1. Successful return to abdominal cavity but umbilicus didn’t seal off properly 2. Covered by skin v. Internal hernia 1. Only a problem if chyme flow is constricted © 2009 Mark Tuttle 4. 5. 6. 7. 8. 2. Loop of small intestine pushes into mesentery of midgut loop vi. Ileal (Meckel) Diverticulum 1. Occurs in 2-4% of population 2. 3-6cm long outpocket of the ileum 3. May be attached to umbilicus 4. Due to persistent yolk stalk that may be attached to umbilicus 5. May contain ectopic gastric or pancreatic tissue Causes ulcers 6. Can result in omphalocenteric fistula (milk squirts out of umbilicus Correlate the organ positional relationships within the abdominal cavity with the developmental history of the region. a. All of the foregut derivatives are supplied by the Celiac trunk b. All of the midgut derivates are supplied by the superior mesenteric artery c. All of the hindgut derivatives are supplied by the inferior mesenteric artery What is a Meckel’s form of ileal diverticulum? Umbilico-ileal fistula? What is the congenital basis of these conditions? a. a remnant of the proximal part of the yolk stalk within the embryo that arises as a fingerlike diverticulum, 3–6 cm long, from the antimesenteric border of the ileum between 40 and 50 cm from the ileocecal junction; it may be attached to the umbilicus. If its mucosa includes gastric tissue, peptic ulceration and bleeding may result (see above) Briefly describe the positional changes that occur in the arteries and veins associated with the caudal foregut and midgut. Briefly describe the formation of enteric autonomic ganglia of the digestive system from neural crest cells a. Sympathetic i. Route 1. Neuronal axon exits the spinal cord via the ventral root and travels along a mixed spinal nerve. 2. Exits the spinal nerve via the white ramus and passes through a paravertebral ganglion w/out synapsing to any cell body 3. Travels via a splanchnic nerve to reach a pre-vertebral ganglion where it synapses with ganglion cell bodies 4. Axons from this ganglion travel through the mesentery to synapse with the target tissues in the gut ii. Migrating neural crest cells are the origin of the sympathetic postganglionic cells that form the para-vertebral ganglia b. Parasympathetic i. Travels via the vagus nerve and innervates the neurons of Auerbach’s Plexus and Meissner’s Plexus ii. NCC give rise to the neurons of the Enteric Nervous System Describe the developmental errors leading to: a. Ailiary atresia b. Anular pancreas i. Messed up rotation of pancreatic buds results in part of the pancreas constricting the duodenum c. Omphalocoel, Hiatal and umbilical hernias i. See above d. Segmental duplication of the intestinal tract © 2009 Mark Tuttle i. Abnormality that occurs when, during the solid stage of development, there is uneven canalization of the lumen resulting in a two lumens, one of which does not communicate with the rest of the GI tract. ii. In the cystic type, it is a localized region iii. In the tubular type, there are parallel tracts for part of the intestine with one being closed off from the main tract e. Malrotations of the midgut resulting in: Subhepatic cecum, Mobile cecum, Volvulus i. See above DIGESTIVE SYSTEM - HINDGUT 9. Define/describe: a. Allantois i. Endodermal evagination of the developing hindgut which becomes surrounded by the mesodermal connecting stalk. The connecting stalk forms the umbilical vasculature. ii. These endodermal and mesodermal tissues together form the human umbilical cord iii. The allantois later becomes the urachus, which removes nitrogenous waste from the fetal bladde b. Cloaca i. The expended terminal part of the hindgut lined by endoderm c. Cloacal membrane i. In contact with surface ectoderm d. Anal pit (Proctodeum) i. Region of the surface ectoderm overlying the cloacal membrane e. Uroretal septum i. During development the cloaca is subdivided by the urorectal septum into a ventral urogenital region nand a dorsal anal-rectal region ii. At week 7 the urorectal septum fuses with the cloacal membrane at the future perineal body and subdivides it into a ventral urogenital membrane and a dorsal anal membrane iii. The ventral part of the cloacal sphincter becomes all the muscles of the UG triangle iv. The dorsal part of the cloacal sphincter becomes the external anal sphincter v. The anal membrane usually ruptures during week 8 f. How do these structures relate to those of the adult colon, rectum, anal canal and urogenital organs? i. See above 10. Describe the process by which the protodeum (anal pit) is formed. a. Occurs during week 4-6 b. Urorectal canal seperates into urinary and anal canals c. Occurs before the 3rd month d. Problems can occur either when it fails to separate or is deviated 11. Define/describe the location of the tissue that will form the urorectal septum. a. Dividedes the cloaca into dorsal and ventral parts by a wedge of mesenchyme, the urorectal septum, that develops in the angle between the allantois and hindgut © 2009 Mark Tuttle b. As the septum grows toward the cloacal membrane, it develops forklike extensions that produce infoldings of the lateral walls of the cloaca c. These folds grow toward each other and fuse, forming a partition d. Occurs by the 7th week (before 3rd month) 12. List the major structures (organs) that are definitively situated anterior to the tissue plane created by the urorectal septum; those situated posterior to the plane. a. Urorectal septum divides the cloacal sphincter into anterior and posterior b. Posterior part becomes the anal sphincter c. The anterior part develops into the superficial transverse perineal, bulbospongiosus, and ischiocavernosus muscles d. This explains why one nerve, the pudendal nerve, supplies all of these muscles 13. Describe the vascular supply (blood and lymphatic) and innervation of the portion of the anal canal derived from the hindgut; the portion of the anal canal derived from the proctodeum. a. The pectinate line divides the anal canal into hindgut endoderm and proctodeum ectoderm b. Above pectinate line i. Autonomic nerves ii. Superior rectal a. c. Below pectinate line i. Somatic nerves ii. Middle/inferior rectal a. 14. Explain: a. congenital megacolon (Hirschprung’s disease) i. 1/5000 ii. Absence of ganglion cells in a variable length of distal bowel iii. Lack autonomic cells in the myenteric plexus distal to the dialated segment of colon iv. Can be a result of failure of neural crest cells to migrate into the colon during the 5th-7th weeks v. Dilation nresults form failure of relaxation nof the aganglionic segment, which prevents movement of the intestinal contents vi. Usually only the rectum and sigmoid colon are involved b. imperforate anus i. 1/5000 ii. More common in males iii. Abnormal development of urorectal septum, resulting in incomplete separation of the cloaca into UG and anorectal portions iv. There is normally a temporary communication between the rectum and anal canal dorsally from the bladder and urethra ventrally, but it should close when the urorectal septum fuses with the cloacal membrane c. fistulae between the rectum and urethra in the male i. incomplete sparatio nby the urorectal septum d. anoperineal fistulae i. Anal canal opens into the perineum e. anal stenosis i. Anal canal is too narrow © 2009 Mark Tuttle ii. Probably caused by a slight dorsal deviation of the urorectal septum as it grows caudally to fuse with the cloacal membrane f. anorectal agenesis. i. Rectum ends superior to the puborectalis muscle when there is anorectal agenesis ii. Results in a fistula to the urethra in males or the vagina in females DIGESTIVE TRACT - CHALLENGE 15. Summarize the vascular supply of each portion of the gut, a. Stomodeum i. ???? b. supradiaphragmatic foregut i. Celiac trunk c. infradiaphragmatic foregut i. Celiac trunk d. Midgut i. Superior mesenteric artery e. Hindgut i. Inferior mesenteric artery 1. Superior rectal a. f. Proctodeum i. Middle/inferior rectal a. 16. Summarize the autonomic innervation of the portions of the gut mentioned above. © 2009 Mark Tuttle GI and Associated Glands – Chiaia 1. List the functions of the liver. a. Storage and filtration of blood b. Vitamin storage and excretion (A, B12, C, D, E, K) c. Synthesis and secretion of bile d. Metabolic i. Protein synthesis (albumin, prothrombin, fibrinogen) ii. Lipoprotein and cholesterol synthesis iii. Carbohydrate metabolism (glycogenesis, glycogenolysis, gluconeogenesis) iv. Metabolism of lipid-soluble drugs and steroids v. Urea formation (from ammonium ions) 2. Identify the components of the portal triad. Identify what the function is of each component. a. Portal vein b. Hepatic a. c. Bile duct d. Nerves e. Lymphatics 3. Describe the models of liver organization including the classic liver lobule, portal lobule and liver acinus. c. Classic lobule i. Based on CT arrangement (indistinct in humans) ii. Hexagonal-shaped parenchymal region bounded by portal tracts at each corner and central vein at each center d. Portal lobule i. Secretory units whose outflow drains into a common interlobular duct ii. So, defined in terms of bile flow (this is the exocrine function of liver) e. Acinus i. Smallest functional unit of liver ii. Diamond shaped mass of hepatocytes lying between two central veins at the apices of its long axis and two portal tracts at the apices of its short axis iii. The meridian of the diamond is tranversed by preterminal branches of a distributing arteriole which suypplies blood to the sinusoids iv. Zones 1. Zone 1 a. Well oxygenated blood and nutrients, minimally exposed to metabolic waste 2. Zone 2 a. Receive only moderately oxygenated blood b. Intermediate exposure to metabolic waste 3. Zone 3 a. Receive poorly oxygenated blood b. Constitutes the primary site of alcohol and drug detox and its hepatocytes are much more vulnerable to toxic damage than those zone 1! 4. Describe the path of both blood flow and bile flow in the liver. © 2009 Mark Tuttle a. b. c. d. 75% of blood supply is Portal v. 25% of blood supply is proper hepatic a. The liver is drained entirely by the hepatic v. Inlet arterioles and venules empty into endothelially-lined sinusoids where separate the plates of hepatocytes in the parenchyma e. The flow toward central vein f. Conducting vein, distributing vein, sinusoid, central veinule, sublobular vein, collecting vein, hepatic vein, IVC g. Bile flows in the opposite direction, from inward out to the bile ducts 5. Describe the histological and functional organization of liver sinusoids including the contribution of Kupffer cells and endothelial cells. f. Plates/cords are continuous arrangement of hepatocytes, endothelially lined g. Linked to hepatic sinusoid via Space of Disse, filled with plasma but no RBCs h. Numberous microvilli i. Perisinusoidal cells of ito i. Irregular cells with long cytoplasmic processes ii. Concentrate vitamin A iii. Function not well understood a. Endothelial cells are discontinuous without a continuous basal lamina i. Riddled with clusters of holes – sieve plates b. Supported by reticular fibers c. Lumen of sinusoid contains large branched Kupffer cells d. Phagocytose damaged RBCs and plasma debris 6. Describe the bile canaliculi and their function. a. Composed of the lateral domain of hepatocytes- that which borders another hepatocyte (as opposed to that which borders the sinusoid) b. Membranes adjacent to this are surrounded by tight junctions which isolate the canniliclus from extracellular space c. Canaliculi empty into the bile ductules (Canals of Herring) which lead to the portal bile ducts d. Lined by cuboidal epithelium e. Transported here via ATP-dependent transporters f. Composed of bile salts + bilirubin 7. Describe the general ultrastructure of the hepatocyte. a. Polygonal shape b. Usually binucleated, centrally located nucleus c. Numerous mitochondria d. Abundant rER and free ribosomes e. Prominent Golgi f. Numerous peroxisomes, lysosomes, endosomes g. Lipid droplets (VLDL h. Abundant sER (drug detox) i. Microsomal mixed function noxidase system responsible for the metabolism of barbiturates antibiotics and toxins ii. Methylation, conjugation, and oxidation nare the most common methods of drug inactivation nand detoxification nperformed in the hepatocyte sER © 2009 Mark Tuttle iii. Cytorchrome p450 is the major enzyme in the liver involved in drug metabolism iv. First pass metabolism: where a drug is removed before it even has the opportunity to work 8. Identify the endocrine and exocrine portions of the pancreas. a. Endocrine: insulin + glucagon (Islets of Langerhans) b. Exocrine: pancreatic enzymes (Acini) i. Intralobular: simple cuboidal-columnar ii. Interlobular duct: low columnar iii. Centroacinar cells: Low cuboidal iv. All are pyramidal shaped v. Secretions 1. Tripsin proenzyme 2. Trypsin inhibitor (protecting pancreas from auto-digestion by trypsin until it reaches duodenum) 3. Pancreatitis can result in lysis of the acinar cells and release of active digestive enzymes into the abdominal cavity causing serious organ damage 9. Describe the histological organization of the islets of Langerhans. List the function of the various cell types. a. Most numerous in the tail of the pancreas b. Ovoid groups of clear endocrine cells scattered throughout the exocrine pancreas 10. Describe the histological organization of the gall bladder and correlate the function to the morphology of this organ. a. Simple columnar epithelium i. Clear cells ii. Brush cells b. Lamina propria c. Muscularis externa i. Smooth muscle of mixed orientation ii. Responsive to CCK d. Perimuscular connective tissue e. Simple squamous epithelium (serosa) © 2009 Mark Tuttle Posterior Abdominal Wall – Lane 1. Describe the skeletal, muscular, and fascial components of the posterior abdominal wall. a. Skeletal i. Lumbar vertebrae ii. Sacral vertebrae (this is more pelvic than abdominal) iii. Inferior thoracic vertebrae iv. Iliac Fossas b. Muscular i. Quadratus lumborum ii. Psoas major iii. Psoas minor iv. Iliacus v. Diaphragm c. Fascial i. Thoracolumbar fascia 1. Fusion of erector spinae + quadrates tendons 2. Components a. Anterior: Just quadratus b. Middle: Quadratus + erector spinae c. Posterior: Just erector spinae 2. Describe the attachments and actions of the psoas major, iliacus and quadratus lumborum muscles. a. Quadratus lumborum i. Attachment 1. Inferior portion of 12th rib 2. TVPs of lumbar vertebrae 3. Iliolumbar ligament ii. Action 1. Unilateral: Bend to same side b. Iliacus i. Attachment 1. Ala of sacrum 2. Superior 2/3 of iliac fossa 3. Anterior Sacroiliac ligaments 4. Lesser trochanter of femur ii. Action 1. Flex hip joint c. Psoas major i. Attachment 1. TVPs 2. IV discs 3. Lesser trochanter of femur ii. Action 1. Flex hip joint 3. Understand the attachments, arches, apertures, components, innervations and blood supply of the diaphragm. a. Attachments © 2009 Mark Tuttle i. 12th rib ii. Medial arcuate ligaments (2) 1. One for each place Psoas mm. pass through 2. On lateral side of each crus iii. Right crus 1. Attaches to L1-L3/L4 vertebral body 2. Wraps around esophageal hiatus iv. Left crus 1. Attaches to L1-L2/L3 vertebral body 2. Ligament of Treitz a. Supports duodenal/jejuna junction b. Suspensory ligament of the duodenum v. Median arcuate ligament (1) 1. Fascia of the diaphragm 2. Wraps around medial aspect of right and left cruses and around the aortic hiatus b. Aperture i. Hiatus for IVC (T8) ii. Esophageal hiatus (T10) iii. Aortic hiatus (T12) 1. Thoracic duct 2. Azygous v. 3. Hemiazygous v. c. Blood supply i. Pericardiacophrenic a. and v. 1. Branches laterally of of the internal thoracic a. ii. Musculophrenic a. and v. 1. Branches medially off of the internal thoracic a. iii. Superior phrenic a. and v. 1. Branches off of the aorta just superior/posterior to the aortic hiatus 2. “outside” the diaphragm iv. Inferior phrenic a. and v. 1. Branches off of the aorta just inferior to the aortic hiatus 2. “Inside” the diaphragm 3. Flows superior laterally d. Innervation i. Efferent 1. Phrenic nn. (C3-C5) ii. Afferent 1. Phrenic nn. (C3-C5) in the center 2. Intercostal nn. (T5-T11) at the periphery 3. Subcostal nn. (T12) at the periphery 4. Be able to describe the relationships of the diaphragm to structures which pass through it. a. See above: “apertures” 5. Describe the course and "paired" branches of the abdominal aorta and inferior vena cava as they travel through the posterior abdomen. © 2009 Mark Tuttle a. Arteries i. Lumbar arteries (4 on each side) 1. Analogous to intercostal aa. ii. Superior mesenteric a. 1. Branches off of abdominal aorta just inferior to celiac trunk (T12) iii. Inferior mesenteric a. 1. Branches off abdominal aorta inferior to SMA iv. Left/Right renal aa. 1. Branch off of abdominal aorta just inferior to celiac trunk v. Left/Right Gonadal (testicular/ovarian) aa. 1. Branch off of abdominal aorta just inferior to SMA vi. Right/Left Common Iliac aa. 1. Branch at the level of the aortic bifurcation (L4) 2. External Iliac aa. a. Deep circumflex aa. i. Branch and run along the inguinal canal and iliac spine superior-laterally b. Inferior epigastric aa. i. Branch and run along the inguinal canal inferior-medially 3. Internal Iliac aa. b. Veins i. Similar to arteries ii. Join with IVC on right 1. Azygous v. 2. Right L1 v. 3. Right gonadal v. 4. Right renal v. iii. Join with LEFT RENAL vein on left 1. Hemiazygous v. 2. Left L1 v. 3. Left gonadal v. 6. Understand the system of lymphatic vessels and nodes located along the posterior abdominal wall. What is the pattern of lymphatic drainage within the abdomen? a. Run concurrently with vasculature b. Flow i. Visceral nodes Parietal nodes Cysternae chyle Thoracic duct 7. Describe the branches of the lumbar plexus, including their courses and innervations. a. Iliohypogastric n. (L1) i. Sensory to parietal peritoneum b. Ilioinguinal n. (L1) i. Sensory to parietal peritoneum ii. Bifurcation point off of L1 from iliohypogastric n is variable c. Genitofemoral n. (L1-L2) i. Cremaster m. in male, sensory for labia in female d. Lateral femoral cutaneous n. (L2-L3) © 2009 Mark Tuttle i. Passes underneath inguinal ligament just medial to ASIS ii. Innervates skin on lateral surface of thigh e. Femoral n. (L2-L4) i. Underneath Psoas Major m. f. Obturator n. (L2-L4) i. Adductors of thigh g. Lumbrosacral trunk (L4-L5) i. Runs over the ala of sacrum ii. Contributes to sacral plexus (ex. sciatic n.) 8. Describe the anatomy, relations, fascial coverings, internal structure, and vascular supply of the kidneys. a. Kidney anatomy i. Thin fibrous capsule ii. Cortex 1. Outer material 2. Glomeruli present iii. Renal columns 1. Glomeruli present iv. Medulla v. Renal pyramid 1. Apex of pyramid is capped by minor calyx vi. Calyx 1. Duct for forming urine out of a section of the kidney vii. Renal pelvis 1. 2-3 major calyxes form this viii. Renal sinus 1. Has a lot of fat within it 2. No urine here 3. Vasculature present here ix. Ureter 1. Only a few millimeters in diameter 2. Renal calculi (kidney stones) easily get lodged here b. Renal coverings i. Fibrous capsule ii. Perirenal fat 1. Underneath Pararenal 2. Immediately surrounds kidney 3. Within renal fascia 4. Continuous with transversalis fascia/Psoas fascia iii. Renal fascia iv. Pararenal fat 1. Outside the renal fascia 9. Know the course of the ureter as it passes along the posterior abdominal wall on its way to the urinary bladder. a. Passes anterior to common iliac a. and v. 10. Describe the anatomy, relations, internal structure, and vascular supply of the suprarenal glands. a. Anatomy © 2009 Mark Tuttle i. ii. iii. iv. b. c. d. e. Immediately superior to kidneys Retroperitoneal Near vertebra L 11 Surrounded by its own fibrous capsule distinct from kidney fibrous capsule v. Surrounded by perirenal fat/renal fascia/pararenal fat Internal structure i. Cortex 1. Produces and secretes corticosteroids and androgens ii. Medulla 1. Chromaffin cells produce and secrete catecholamines (epinephrine + norephinepherine) 2. Chromaffin cells are innervated by preganglionic sympathetic fibers of the greater splanchnic n. Arterial supply i. Superior suprarenal a. 1. Branch off of the inferior phrenic a. 2. Consistent ii. Middle suprarenal a. 1. Branch off of abdominal aorta 2. Inconsistent iii. Inferior suprarenal a. 1. Branch off of renal a. 2. Inconsistent Venous drainage i. Left suprarenal v. 1. Drains into left renal vein ii. Right suprarenal v. 1. Drains into IVC Innervation i. Greater splanchnic nn. © 2009 Mark Tuttle Esophagus, Stomach, Intestines – Howard 1. Describe the overall plan of the alimentary canal. a. Mucosa i. Epithelium ii. Lamina propria iii. Muscularis mucosae b. Submucosa i. Many glands here c. Submucosal plexus of Meissner d. Muscularis i. (OBLIQUE LAYER IN STOMACH ONLY) (innermost) ii. Circular muscle iii. Longitudinal muscle e. Myenteric plexus of Auerbach i. In between circular/longitudinal muscluaris f. Serosa i. Connective tissue ii. Epithelium 2. Describe the features of each layer of the alimentary canal. a. Mucosa i. Epithelium 1. Mostly simple columnar a. Secretes enzymes and absorbs nutrients b. Specialized cells i. Goblet cells: secret mucous onto cell surface ii. Enteroendocrine cells: secrete hormones 2. Stratified squamous (ESOPHAGUS & ANUS ONLY) 3. Lamina propria a. Thin layer of loose CT 4. Muscularis mucosae a. Thin layer of smooth muscle b. USUALLY 2 LAYERS EXCEPT IN ESOPHAGUS b. Submucosa i. Loose CT ii. Contains BV, glands, lymphatic tissue iii. Meissner’s Plexus c. Muscularis externa i. Skeletal muscle in mouth, pharynx, upper esophagus, anus ii. Smooth muscle everywhere else acts via peristalsis 3. Describe the innervation of the alimentary canal. a. All neurons & support cells derived from neural crest b. Myenteric Plexus of Auerbach i. Mostly motor ii. Regulates peristalsis iii. Located between muscle layers in muscularis externa c. Submucosal Plexus of Meissner i. Mainly secretory-motor ii. Release hormones and peptides © 2009 Mark Tuttle iii. Innervates mucosa iv. Located in the submucosa v. Enterochromaffin cells (EC cells) 1. Bolus of food contacts and excites 2. Release serotonin 3. 5HC is released 4. excites submocosal ganglion 5. excites myenteric gangia 6. peristaltic waves d. Autonomic input i. Parasympathetic – ACh increases motility ii. Sympathethic – NE relaxes gut 4. Describe the specializations of each region of the alimentary canal. a. Esophagus i. Sero-mucous gland ii. Serous glands 1. Secrete pepsinogen and lysozyme iii. **Muscularis layer is single and discontinuous here, everywhere else it is double layered and continuous b. Stomach i. ** 3 layers of muscularis externa where there are usually 2. Extra one is oblique layer ii. Chemical 1. HCl 2. Pepsin 3. Rennin 4. Gastric lipase iii. Glands are in the lamina propria 1. Parietal cells a. HCl b. Gastric intrinsic factor (B12 absorption) c. Receptors for i. Gastrin (stretch on EC walls) ii. Histamine (stretch on EC walls) iii. ACh (vagus n., psychological) 2. Chief cells a. Pepsinogen b. Gastric lipase c. Renin d. **NO CHIEF CELLS IN CARDIA 3. Enteroendocrine cells a. Glucagon (released when glucose low) b. Gastric inhibitory peptide (released when glucose high – for absorption/insulin release) c. G cell i. Release more gastric juice ii. Increase gastric motility iii. Relax pyloric sphincter © 2009 Mark Tuttle iv. Constrict esophageal sphincter c. Small intestine i. 20 ft long ii. Villi 1. Surface 5. Describe/list the functions of the alimentary canal by region and cell type. a. See above 6. Describe the function of the specialized cells of the gut, e.g. digestive glands, gastric pits, enterochromaffin cells, paneth cells, mucus neck cells etc. a. Gastric pits i. Surface lining cell 1. Glcocalyx + microvilli 2. Mostly protective ii. Regenerative cell 1. Replaces anything 2. ** Unusual position high up in pit for GI iii. Mucous neck cell iv. Parietal cell v. Chief cell vi. Enteroendocrine cell 7. Describe the structural and functional regions of the esophagus. © 2009 Mark Tuttle Urinary System – Crissman 1. List the organs of the urinary system and give their functions. a. Kidney: Produces urine b. Ureters: Carries urine from kidney to bladder c. Urinary bladder: Storage of urine d. Urethra: Carries urine to exterior of body 2. List and describe the gross external structure of the kidney. a. Pararenal fat b. Renal fascia c. Parirenal fat d. Fibrous capsule 3. List and describe the gross internal structure and organization of the kidney. a. Cortex on the outside and medulla on the interior b. Medulla forms numerous renal pyramids with the apex of the pyramid facing toward the renal sinus c. Surrounding the pyramids are renal columns containing cortical material 4. Define, list and contrast the parts of the subdivisions of the kidney. a. See terms 5. Define, list and contrast the parts of the uriniferous tubule, nephron and collecting duct. a. 6. Describe and contrast the two major types of nephrons based upon their location in the kidney. a. Cortical nephrons are entirely in the cortex and supplied with blood by the peritubular capillaries (80% of nephrons) b. Juxtamedullary nephrons have Loops of Henle that descend into the medulla and are supplied with blood by the vasa recta 7. Describe and relate the morphology of the various parts of the nephron and collecting ducts to their functions. a. See below 8. Describe the structure of the filtration barrier and relate it to its function. a. The filtration barrier consists of a fenestrated capillary endothelium i. Simple squamous epithelium ii. This filters large molecules iii. It is also negatively charged b. Then interdigitated processes of pedicles of podocytes covered by a diaphragm i. Highly modified simple squamous epithelium ii. Filters medium sized molecules iii. Negatively charged 9. Describe and integrate the blood supply to the kidney with its function. a. Kidney is highly vascular and filters 1200ml of blood/min 10. Describe and examine how the circulation to the cortex is different from that of the medulla of the kidney. Relate this to the function of the kidney. 11. Describe the morphology of the ureter and relate the structure to its function. 12. Describe the morphology of the urinary bladder and relate the structure to its micturition function. 13. Describe and contrast the structure of the male and female urethra and relate its structure to function. © 2009 Mark Tuttle Renin Secreted by juxtaglomerular cells as instructed by macula densa cells. Increases blood pressure by increasing sodium and water reuptake. Also secreted by Chief cells in stomach. fibrous capsule Outermost layer of kidney cystitis inflammation of the urinary bladder. More common in women than men because of their shorter urethra. major calyx Where 2-3 minor calices come together minor calyx Apex of pyramid empties into this renal pyramid Section of medulla between two renal columns of cortex renal papilla Apical tip of medullary pyramid area cribrosa That part of the renal crest or renal papilla at which the papillary ducts open into the minor calyx renal columns Cortical tissue that descends down on the sides of medullary pyramids renal lobe Pyramid plus overlying cortical material renal lobule Part of a renal lobe. It consists of the nephrons grouped around a single medullary ray, and draining into a single collecting duct. multi lobar Human kidneys contain multiple lobes (10-12) whereas some animals have unilobar medullary rays Straight portions of proximal & distal tubules as well as collecting tubules renal corpuscle Includes Bowman’s capsule, Bowman’s space, and glomerulus Bowman's capsule The most proximal part of the nephron proximal & distal convoluted tubule These, along with the renal corpuscle form the cortical labyrinth Loop of Henle Composed of the straight portions of the proximal and distal tubules. Also has thick and thin sections. Thick sections more prominent on the ascending side. collecting ducts Convergence several collecting tubules. Not part of the nephron. Second half of the uriniferous tubules. Runs down the medullary ray. Empties into the Papillary ducts of Bellini. papillary ducts The largest collecting duct. Empties into the minor calyx through area cribosa at the apex of the medullary pyramid glomerulus Not part of nephron. Fenestrated capillaries without diaphragms within the Bowman’s corpuscle and the bowman’s capsule surrounded by Bowman’s space. © 2009 Mark Tuttle visceral & parietal layer Parietal layer of the renal capsule is simple squamous epithelium Visceral layer is modified simple squamous epithelium (podocytes) vasa recta The efferent arterioles of the juxtamedullary nephrons. Run straight down into the medullar alongside the collecting ducts. Drain back into arcuate veins. Important because they pick up the reabsorbed water and essential ions from the connective tissue and return back to the body after the unwatned wastes are removed glomerular filtrate Fluid in the Bowman’s space. Leaves capillary of glomerulus because of hydrostatic pressure. Must pass through fenestra of arteriole (large molecules caught) as well as the slit diaphragm of the podocytes (modified simple squamous visceral layer (medium molecules caught) podocytes Modified simple squamous visceral layer. Lines the glomerulus urinary pole Part of the Bowman’s corpuscle where filtrate exits. vascular pole The part of the Bowman’s corpuscle where blood enters and forms the glomerulus afferent & efferent arteriole Pre and post-glomerulus artery. Note that it is still considered an artery post-glomerulus because it still contains oxygenated blood. This does not become a vein until it dumps oxygen into the peritubular capillary Bowman's space Between Bowman’s Capsule and the glomerulus macula densa Part of the JG apparatus where the distal tubule touches the afferent arteriole pedicle Small foot processes that extend from the podocytes (visceral layer) and form the filtration slits Slit pore Space between pedicles juxtaglomerular cells Part of the afferent arteriole. Modified smooth muscle cells. In between the afferent arteriole endothelium and the macular densa of the distal convoluted tubule. Secrete rennin which increases blood pressure J-G complex Junction of the Bowman’s capsule and the distal convoluted tubule. Specifically junction between the afferent arteriole and the distal convoluted tubule. Consists of the macular densa of the distal tubule, JG cells of the afferent arteriole & extraglomerular mesangial cells. diaphragm basal lamina Fused basal lamina between Fenestrated capillary and Podocyte. Negatively charged. mesangial cell Located within JG apparatus. Difficult to identify and differentiate. © 2009 Mark Tuttle Function as support cells thick segment Simple cuboidal epithelium. Proximal portion of descending limb + greater proportion of distal ascending limb. thin segment Simple squamous epithelium. arcuate artery Supplies the glomerulus and then to the peritubular capillary in cortical nephrons or to the vasa recta of juxtaglomerular nephrons interlobular artery Supply the peritubular capillary network of cortical nephrons intralobular artery Run radially between the lobules in the cortex branch off the arcuate arteries Dome cell **Diagnostic of transitional epithelium interlobar artery Supplies the arcuate arteries which in turn supply the afferent arterioles intertubular capillary network pyelonephritis Inflammation of renal pelvis. Type of UTI urethritis Urethra infection. Type of UTI Region Type of epithelium Thick segment of descending limb Simple cuboidal w/microvilli Thin segment of descending limb Simple squamous Thin segment of ascending limb Simple squamous Thick segment of ascending limb Low simple cuboidal Endothelium of glomerulus Simple squamous Podocytes Highly modified simple squamous Straight portion of proximal tubule Simple cuboidal w/microvilli Convoluted tubules Low simple cuboidal epithelium Intercalated cells of cortical collecting ducts Cuboidal Medullary collecting ducts Cuboidal Ureter Transitional Mucosa of bladder Transitional © 2009 Mark Tuttle Perineum – Morse 1. Define the boundaries of the anatomical region known as the perineum. a. The perineum is everything below the pelvic diaphragm. b. Everything between pubic symphysis and the coccyx c. Composed of two triangles i. Urogenital triangle 1. Ischial tuberosities and the pubic symphysis ii. Anal tangle 1. Ischial tuberosities and the coccyx 2. Anal Triangle a. Define the boundaries of the ischioanal fossa. i. The iscioanal fossa exists within the anal triangle and includes the space between levator ani, the ischial tuberosities and the anus b. Describe the course of the pudendal nerve and internal pudendal vessels through the gluteal region and anal triangle. i. Pudendal n. 1. Leaves the sacral plexus and travels out of the Greater Sciatic foramen and then back in through the lesser sciatic foramen through the pudendal canal (formed by fascia of obturator internus) 2. Gives off inferior rectal nn. 3. Gives off the perineal n. a. Superficial branch becomes the posterior scrotal n. b. The deep branch runs in the superficial pouch 4. The pudendal n. becomes the Dorsal n. of the Penis ii. Internal pudendal a. 1. Gives off the inferior rectal a. 2. Gives of transverse perineal a. 3. Gives off the perineal a. (superficial to perineal membrane) 4. Deep artery of penis/clitoris (deep to perineal mem – pierces distally) 5. Dorsal artery of penis/clitoris (deep to perineal mem. – pierces distally) 6. Urethral a. c. Define the location and contents of the pudendal canal. i. The pudendal canal is formed from fascia of obturator internus m. and contains the pudendal n. the internal pudendal a. and the internal pudendal v. d. Describe the course and distribution of the inferior rectal nerve and vessels. i. These are the first branches of their respective parent neurovasicles ii. The nerve supplies levator ani e. Describe the location and divisions of the external anal sphincter muscle. i. The external sphincter is at the external border of the anus and is skeletal muscle f. Define the location and importance of the perineal body. i. The perineal body is the point of attachment of the transverse perineal muscles and is important during childbirth because it may be cut in order to prevent vaginal tearing g. Define the types of hemorrhoids and the vessels involved in each type. © 2009 Mark Tuttle i. Internal hemorrhoids involve the internal venous plexus and aren’t painful while the external hemorrhoids involve the external veinous plexus and are very painful h. Describe the lymphatic drainage of the anal triangle i. The pectinate line divides lymph drainage 1. The top part goes to pelvic lymph nodes 2. The superficial part goes to inguinal lymph nodes i. Understand the importance of the fat in the ischiorectal fossa. i. The fat here must be able to accommodate distension of the rectum during defecation 3. Urogenital Triangle a. Describe the fascial reflections in the urogenital triangle and the relationships each layer has to the major subdivisions of the urogenital triangle (superficial and deep pouches). i. Superficial to deep 1. Subcutaneous fascia 2. Superficial Perineal Fascia (Colle’s fascia) 3. Superficial Perineal Pouch 4. Deep Perineal fascia enveloping the corpus cavernosus/spongiosus 5. Perineal membrane 6. Deep pouch 7. UG diaphragm and Levator ani (superficial fascia of UG) b. Define the relationships of the fascia of the urogenital triangle to that on the anterior abdominal wall. i. Dartos Tunic 1. Dartos muscle none 2. Colle’s Fascia Scarpa’s Fascia ii. Coverings of Spermatic cord 1. External spermatic Fascia External oblique 2. Cremaster muscle Internal oblique 3. Internal Spermatic Fascia Transversalis fascia iii. Tunica vaginalis parietal/visceral Peritoneum c. Be able to trace the possible routes of spread for fluids escaping into the potential space between the superficial and deep fascia (superficial pouch) of the urogenital triangle . i. If the urethra is ruptured especially in a male, urine can track into the superficial perineal pouch and even up into the abdomen since it is contained within colle’s fascia d. Describe the contents of the superficial and deep pouches of the urogenital triangle. i. Superficial pouch 1. Ischiocavernosus, Bulbocavernosus mm 2. Superficial transverse perineal mm. ii. Deep pouch 1. Bulbourethral glands 2. Membranous portion of the urethra in males 3. Ischioanal fossa 4. External sphincter © 2009 Mark Tuttle e. Describe the course of the pudendal nerve and internal pudendal vessels (and branches) through the superficial and deep pouches. i. See above f. Describe the role of the autonomic nervous system in the male and female sexual response. i. Male 1. S2,3,4 Keep the penis off the floor 2. Parasympathetic 3. Sympathetic is involved in the refractory period ii. Female 1. Assume similar: Parasympathetic is responsible for clitoral erection g. Describe the arrangement of the erectile bodies for the penis/clitoris. i. Females have two bolbospungiosi h. Define the blood and nerve supply to the penis/clitoris. i. Same ii. Deep a iii. Dorsal a iv. Deep dorsal v v. Supervicial dorsal v. vi. Dorsal n. of penis/clitoris i. Define the position and importance of the muscles in the superficial and deep pouches. i. j. Define the perineal body and list the muscles that attach to it. i. External anal sphincter ii. Bulbospongiosus iii. Superficial transverse perineal muscle iv. Anterior fibers of the levator ani v. Fibers from external urinary sphincter vi. Deep transverse perineal muscle k. Be able to define the following: i. Vulva 1. All the external female genetalia a. Vagina (Vestibule) b. Labia majora/minora c. Clitoris d. Greater/lesser vestibular glands e. Mons pubis ii. Vestibule 1. Space inside the vagina before the cervix iii. Prepuce 1. Foreskin/Clitoral hood iv. Hymen 1. Temporary skin layer over the vaginal orifice v. Episiotomy 1. Cut through theperineal body during childbirth to prevent vaginal tearing vi. Circumcision © 2009 Mark Tuttle 1. Removal of foreskin © 2009 Mark Tuttle Pelvis Walls and Floor – Morse 1. Define the relationship of the tendinous arch to the obturator internus and levator ani muscles. a. Tendinous arch makes the lateral border of: i. Lavator Ani 1. Iliococcygeus m. (mostly) 2. Pubococcygeus m. ii. (Ischio)coccygeus m. b. Tendinous arch forms the medial border of: i. Obturator internus m. 2. Explain the difference in orientation of the pelvic and urogenital diaphragms. a. ????????????????/ 3. Define the parts of the pelvic diaphragm/urogenital diaphragm. a. Pelvic diaphragm (Concave) i. Levator Ani mm. 1. Puboccygeus m. 2. Puborectalis m. 3. Iliococcygeus m. ii. (Ischio) Coccygeus m. b. Urogenital diaphragm i. Fills the space within the pubic arch ii. covers the anterior part of the inferior pelvic aperture (pelvic outlet) iii. Components 1. superficial transversus perineal m. a. a small bundle of muscle fibers that pass along the back border of the urogenital diaphragm and assists other muscles in supporting the pelvic tissues 2. bulbospongiosus m. (male only) a. are united and surround the base of the penis 3. ischiocavernosus m. (male only) a. a tendinous structure that extends down to the margin of the pubic arch and assists the function of #2; and 4. sphincter urethrae m. a. muscles that arch around the urethra and unite with those on the other side. 4. Describe the relationship of the parts of levator ani to pelvic organs. a. Levator Ani has the bladder immediately superior to it (also prostate in males), and the urethra pierces the Lavator Ani via the urethral hiatus b. The rectum pierces the Levator Ani c. In females, the vagina also pierces the Levator ani. 5. Describe the nerve supply to levator ani. a. Book i. Direct branches from sacral plexus (S4) ii. Inferior rectal n. from pudendal n. b. Wikipedia i. pubococcygeus and iliococcygeus mm: 1. levator ani nerve (S4) 2. inferior rectal nerve from pudendal nerve (S3, S4) © 2009 Mark Tuttle 3. coccygeal plexus ii. puborectalis m: 1. S3, S4. 2. levator ani nerve 6. Describe the branching pattern of the internal iliac artery. a. Right Internal Iliac Artery i. R. Umbilical a. ii. R. Obturator a. iii. R. Inferior vesical a. iv. R. Uterine a. v. R. Middle rectal a. vi. R. Internal pudendal a. vii. R. Inferior gluteal a. 7. Describe the distribution of the branches of the sacral plexus. a. 8. Define the subplexuses that are derived from the inferior hypogastric plexus. © 2009 Mark Tuttle Development of the Urinary System – Crissman 1. List the germ layer(s) from which the urinary system develops. a. Intermediate mesoderm 2. List/describe the structures that are contributed to by the pronephros, mesonephros and the metanephros and their respective duct systems. a. Pronephros i. Rudimentary, transitory, nonfunctional ii. Ducts run caudally to cloaca b. Mesonephros i. Mesonephric ducts develop lateral to the degerated mesonephric ducts ii. Mesonephric tubues form (40) in craniocaudal succession iii. Enlarge to form duct iv. Differentiate into rudimentary adult nephrons v. Medial end of tubule forms Bowman’s Capsule vi. Degenerates in females, but part of it is maintained n males to form part of ductus deferens c. Metanephros i. Ureteric bud forms the ureter, renal pelvis, calyces, collecting ducts ii. Metanephric blastema forms nephron 3. Describe the region of the embryonic body in which the mesonephros and metanephros develop. a. Pronephros i. cervical b. Mesonephros i. Upper thoracic to 3rd lumbar c. Metanephros i. AKA sacral metanephric system 4. Define/describe/explain the tissues or structures that combine to form the metanephric kidney. a. Reciporical induction of ureteric bud and metanephric blastema b. WT-1 expressed by blastema, stimulates synthesis of GDNF c. C-ret, a receptor for GDNF on ureteric bud causes bifurcation (into lobes) d. Ureteric bud forms the ureter, renal pelvis, calyces, collecting ducts e. Metanephric blastema forms nephron 5. Be able to list the parts of the uriniferous tubule (nephron & collecting ducts) that are derived from each tissue or structure. a. See above 6. Be able to relate the role of the following substances in the development of the kidney, or in the formation of congenital defects: WT-1, c-ret, PDK-1 & -2,Mox-1, Nmyc, LIM-1, Pax-2, BMP-7,Wnt-4, Wnt-11, Hoxc-9,NGF, IGF, cadherins, laminin, & integrin. a. WT1 i. Expressed in blastema, regulates GDNF ii. Induces ureteric bud formation b. C-ret, receptor i. For GDNF is responsible for branching and ureters & renal agenesis c. Pax 2, BF 2, and Wnt 2 © 2009 Mark Tuttle i. All needed to induce ureteric bud formation & transform mesenchymal cells into epithelial cells d. Mox 1, N-myc, Hoxc-9 i. Required for nephron differentiation & glomerulus formation e. PDK-1 i. Mal-expressio ncauses epithelial hyperplasia & autosomal dominant polycystic kidney disease f. NGF i. Expression in the blastema is necessary for formation nof nephrogenic tubules g. GDNF i. Needed for branching of ureteric bud h. IGF i. Over-expression causes Wilm’s tumors i. Cadherins i. To make tight junctiosn in forming epithelial tubes j. Laminin, integrin i. Necessary for diapedesis to occur as cells migrate 7. Describe the development of the vascular supply to the definitive kidney. Explain the occurrence of "accessory renal arteries". a. Kidney derives its blood supply form the nearest vessels b. First blood supply comes from common iliac arteries c. Vascular supply should change as kidney (relatively) ascends d. Accessory renal arteries i. Polar: inferior/superior renal artery (25%) ii. Obstruction of ureter can occur if inferior polar crosses anterior to ureter iii. Causes hydrophrosis, dilation of pelvis and calyces due to backup of urine 8. Define/describe/explain fetal lobulation of kidney, renal agenesis, and renal duplication, Potter's syndrome. a. Fetal lobulation i. Bifurcation occurs as signaled by c-Ret b. Renal agenesis i. Lack of kidney 1/1000 ii. Probably due to lack of ureteric bud iii. Usually no symptoms due to compensatory hypertrophy of remaining kidney c. Renal duplication i. When two separate systems develop in the same kidney ii. Two ureters d. Potter’s syndrome i. 1/3000 ii. Neither kidney forms iii. Due to failure of ureteric bud or blastema forms 9. Explain the formation of a "horseshoe" kidney and its positional relationships with surrounding organs and vessels. a. 1/500 © 2009 Mark Tuttle 10. 11. 12. 13. 14. 15. b. Inferfior poles fused together to form one U shaped kidney c. Kidney starts to ascend but gets held up by inferior mesenteric artery Define/describe/relate polycystic kidney to it morphology and pathogenesis. a. Malexpression of PDK1 causes this b. Numerous cysts throughout the kidney c. Recurrent infectiosn d. Occurs because of nonfunctional cilia e. The cilium normally directs the flow of fluid through the tubules f. In PCKD, the cilium is non-functional so the epithelial cells divide profusely and form the cysts Explain the formation of the ureters, renal pelvises, and calices. Explain the bifid ureter and common clinical findings associated with it. a. Ureters, renal pelvices, and calices are all progeny of the ureteric bud b. Bifid ureter happens because complete division of the ureteric bud List and describe the developmental history of the 3 portions of the urogenital sinus. What definitive structures are derived from each? a. Vesical i. Superior continuous with allantois ii. In males forms most of bladder iii. In females forms most of bladder b. Pelvic i. Middle portion ii. In females forms complete urethra c. Phallic i. Inferior portion ii. In males forms proximale penile urethra iii. Distal portion is formed by glandular urethral plate iv. In females, forms the vestibule of the vagina Explain how exstrophy of the bladder occurs. a. Septation of the cloaca is occurring, mesonephric ducts with attached ureteric buds are incorporated nto the posterior wall of the forming bladder b. The opened mesonephric ducts continue farther inferiorly to the opening of the urethra Explain the development of the urethra. a. See above Be able to relate the timing and chronology of above events to each other. a. Pronephros early 4th week b. Mesonephros late 4th week c. Metanephros 5th week (functional in 9th week) d. Bifurcation Day 32 (5th week) e. Lobes formed 16th week f. 4 bifurcatiosn 6th week g. Bifurcation stops 32nd week h. Kidneys in normal position: 9th week (T12-L3) © 2009 Mark Tuttle Pelvis (Visceras) – Morse 1. Describe the surfaces of the urinary bladder and the viscera which contacts them. a. The superior and lateral/medial parts of the bladder are covered by parietal peritoneum 2. Describe the pelvic course of the ureters. a. The ureters leave the kidney and travel inferiorly posterior to the gonadal vessels and then anterior to the iliac vessels, anterior to the sacral plexus and then posterior to the deferens (in males) b. The travel obliquely through the detrusor m 3. Define the bladder trigone. a. The two ureturs and the opening of the urethra 4. Describe the pelvic course of the vas deferens. a. The ductus deferens leaves the testes and enteres the superficial inguinal ring and the spermatic cord travel through the deep inguinal ring before leaving and then along the surface of the posterior portion of the bladder before meeting with (R and L separate) the seminal gland 5. Describe the position and gross anatomical structure of the seminal vesicles. a. Reside on the posterior side of the bladder on the superior portion of the vas b. They meet with each side’s respective vas just before forming the ejaculatory duct 6. Discuss the route of a sperm cell during emission and ejaculation. a. passes through the ejaculatory ducts and is mixed with fluids from the seminal vesicles, the prostate, and the bulbourethral glands to form the semen, or ejaculate b. Emission is a parasympathetic activity, but orgasm and ejaculation are predominantly under the control of the sympathetic nervous system. Also the detumescence/Resolution/refractory period are sympathetic 7. Describe the anatomy of the posterior wall of the prostatic urethra. a. The posterior wall of the prostatic urethra contains a crest called the urethral crest b. On the urethral crest there is the prostatic utricle (vaginalis masculina). It is flanked by the two ejaculatory ducts c. All along the urethra in this area are prostatic ducts 8. Define the lobes of the prostate and understand how enlargement effects urine flow and retention. a. The prostate is divided into anterior and posterior lobes by a coronal plane through the urethra b. In men, the posterior lobe is also subdivided into a middle lobe, sectioned off by the ejaculatory ducts 9. Describe the accessory reproductive glands of the male and define the contribution of each to semen. a. Male i. Prostate 1. 30% of semen 2. Alkaline, thin, milky, watery 3. Citrate 4. Phosphate 5. Calcium © 2009 Mark Tuttle 6. Profibrinolysin a. After a few minutes, causes lysis of the mucoid clot of semen ii. Bulbourethral (Cowper’s) 1. Pre ejaculate (not really part of semen) 2. Helps neutralize acid of urine in urethra and vagina 3. Located in the deep pouch 4. Analogous to greater vestibular glands in females (but females’ are located in the superficial pouch) 5. Only component of semen which isn’t stored, just secreted at the time of ejaculation iii. Seminal gland 1. 60% of semen 2. Fructose 3. Citric acid/other nutrients 4. Prostaglandins a. Reacts with cervical mucous to promote sperm movement b. Reverse peristalsis to move sperm toward egg i. Sperm can reach distal tube in 5 min (couldn’t possibly swim this fast) 5. Fibrinogen a. Helps clot to remain mucoid consistency to hold semen in upper vagina iv. Testes 1. Sperm are 10% of semen b. Female i. Greater vestibular gland (Bartholin’s) 1. Produce mucous to lubricate the vagina, but only a minute contribution ii. Lesser vestibular gland (Skene’s) 1. Organ of female ejaculation 2. Develop from the Wolffian duct of the Mesonephric duct a. In the males this develops in to the vas 3. (Homologous to the prostate) 10. Describe the peritoneal reflections on the pelvic viscera in both sexes. a. Reflected over the bladder and rectum in both sexes and in addition the uterus in the female 11. Define the parts of the broad ligament. a. Mesosalphinx i. Between the Fallopian tube and the ovary b. Mesovarium i. Covers the ovary ii. At a 90 degree angle to the other mesenteries c. Mesometrium i. Between ovary and uterus 12. List the structures that lie between the lamellae of the broad ligament. © 2009 Mark Tuttle 13. 14. 15. 16. 17. a. The uterus, the uterine(fallopian) tubes, the ovary, the ligament of the ovary, the ovarian and uterine arteries, and the round ligament of the uterus b. Uterine arteries, ovarian artery c. opoopheron Delineate the parts of the uterus and vagina. Define the normal position of the uterus and the terms anteversion/anteflexion and retroversion/retroflexion. a. The normal position of the uterus is anteversion and antiflexed. Anteversion refers to the angle at the external os being approximately 90 degrees, measured from the angle between the vagina and the cervical canal. b. Anteflexion refers to the angle ate the internal os being approximately 170 degrees, measured from the angle between the uterine and cervical canal. c. Retroversion is the widening of the angle between the vaginal and cervical axis greater than 90 degrees. If the angle of the external os increases and approaches 180 degrees, the uterus is in danger of fall into the vaginal canal. d. Retroflexion is the widening of the angle between the cervical and uterine axis greater than 180 degrees. e. The two angles are independent of each other, and the uterus can possibly be found in any combination of anteversion, retroversion, anteflexion, or retroflexion Define the ligamentous supports for the uterus. a. Transverse Cervical (Cardinal) Ligament i. This is really the major support of the uterus ii. Contains the uterine a. b. Round ligament of uterus i. Remnant of the gubernaculum c. Broad Ligament i. Contains mesosalphinx, mesovarium, and mesometrium d. Ovarian ligament i. Runs from the uterus to the ovary e. Suspensatory ligament of the ovary i. Ovarian (gonadal) a. runs through here Explain the relationships and importance of the pelvic peritoneal pouches. a. Pelvic peritoneal pouches are of physiological importance because they may accumulate blood, ascites, or other abdominal fluids as a result of pathology. For example, in a female, appendicitis may be detected by the presence of ascites in the rectouterine pouch. b. The rectouterine pouch in particular is important because it represents the lowest point of the abdominal cavity when a woman is standing, and fluid in this area can be easily sampled by insertion of a needle through the posterior fornix of the vaginal canal and aspiration of fluid for analysis. Because the inner 4/5th of the vagina contains no somatic innervation, the woman will not feel pain when a needle pierces the posterior vaginal wall. Distinguish between false and true pelvis and understand which organs are located in each. a. The true pelvis is the region inferior to the pelvic brim, bounded inferiorly by the pelvic outlet. Organs found in the true pelvis include i. empty bladder © 2009 Mark Tuttle ii. non-pregnant uterus iii. lower portion of the rectum iv. perineal structures v. external reproductive organs of the male and female. b. The false pelvis is the region superior to the pelvic brim, separated by a physiological line (continuous with the abdominal cavity) indicated by the inferior aspect of the 5th lumbar vertebral body and the anterior superior iliac spines (ASIS). Structures of the false pelvis include: i. the upper part of the rectum ii. the sigmoid colon iii. the gravid uterus (pregnant) iv. the superior aspect of the full bladder v. the prostate in males. 18. Explain the relationships of the vaginal fornices to surrounding structures a. The cervix creates recesses called fornices where it projects into the vagina. Fornices are anterior, posterior, and lateral, being circumferential to the cervix. b. The posterior fornix is the deepest and most closely associated with the rectouterine pouch. c. The anterior fornix lies just posterior to the urinary bladder. © 2009 Mark Tuttle Female Reproductive System – Crissman 1. Describe the process of oogenesis and indicate the embryologic origin of the primordial germ cells. a. Oocytes are derived from Yolk Sac Endoderm b. ~1 million ova present at birth, 200k-400k present at puberty c. Primordial cells (oogonia) migrate from yolk sac endoderm to urogenital ridge d. Follicular cells are derived from mesonephros sex cords (mesoderm) e. Primary oocytes are formed in prenatal life i. Diploid ii. Arrested at prophase by meiosis-inhibiting factor 2. Indicate in which stage of meiosis the oocyte exists prior to ovulation, at ovulation but prior to fertilization, and then following fertilization. a. While dormant in the ovary, oocytes are arrested at prophase b. At ovulation, becomes secondary oocyte i. Completes 1st meiotic division ii. Extrudes 1st polar body iii. Arrested at metaphase of meiosis II iv. Still considered diploid c. At fertilization, completes meiosis II 3. Describe the morphology of the ovary including the surface covering, the capsule, the cortex, and medulla. Identify and contrast the components of each. a. Cortex i. Covered by germinal epithelium (simple cuboidal) ii. Just deep to the epithelium is the tunica albuginea (white coat) 1. Dense irregular CT iii. CT layer w/fibroblasts which look like sm. Muscle b. Medulla i. Mostly stroma, ~dense irregular CT ii. Very vascular iii. Contains helicine coiled arteries 4. Describe and integrate the development and morphology of ovarian follicles, beginning with primordial follicles and ending with Graafian follicles. Relate the follicular components to their origin, sites of hormonal production and describe their effects on the other components of the female reproductive tract. a. Sequence i. Primordial follicles 1. Large cell 2. Light staining 3. Single layer of flattened follicular cells 4. Don’t develop FSH receptors until puberty 5. Under influence of activin secreted by the oocyte ii. Primary follicle 1. **cuboidal epithelial follicular cells diagnostic as opposed to flattened cells in primordial 2. Zona pellucid begins to form a. Intimate with membrane around ovum b. Has glycoproteins secreted by oocyte c. Contains microvilli for exchanging nutrients/wasts © 2009 Mark Tuttle d. Binds spermatozoa, and is required to initiate the acrosome reaction. 3. Theca begins to form outside follicle a. Not under control of FSH, unknown factors instead iii. Secondary follicle 1. Now under FSH control (post puberty) 2. Form small spaces that coalesce to form a single space called the antrum ** diagnostic a. Filled with follicular liquor b. Like plasma c. Contains GAGs, steroid binding proteis d. Help regulate FSH & LH release 3. Ovum now displacd to side of follicle in heap of cells called cumulus oophorus a. Ova b. Zona pelucida c. Corona radiate 4. Theca now well developed a. Externa b. Interna i. Highly vascular ii. **Steroid producing cells that secrete androgens iv. Graafian follicle (mature) 1. 1-2cm 2. Bulges into cortex 3. High estrogen levels in blood now from follicles a. Inhibit FSH release b. Causes LH surge c. Causes meiosis inducing substance 4. Once ovulation occurs, becomes a corpus hemorrhagicus 5. Describe the structure and functions of the theca cells. a. Begins to form in primary follicle b. Matures in secondary follicle i. Forms two layers: Internal and external layer ii. Internal layer is highly vascular & secretes androgens c. When follicle degenerates after ovulation, sometimes thecal cells persist, called interstitial bodies 6. Define and contrast an "atretic follicle" with other follicles. a. At start of cycle, more than one follicle responds to FSH b. 10-20 respond but only 1 is ovulated c. The rest undergo atresia – autolysis, programmed cell death d. Forms small scar 7. Describe the development and fate of the corpus luteum and how it changes when fertilization occurs. Include the theca lutein and granulosa lutein cells, their origin, their function, sites of hormonal production and describe how this affects other components of the female reproductive tract. a. Forms from the corpus hemorrhagicus after ovulation © 2009 Mark Tuttle b. Under the influence of LH c. Temporary endocrine structure d. Granulosal luteal cells develop from granulosal cells (former follicular cells) i. Form 80% of cells in corpus luteum ii. Pale staining iii. ** secrete progesterone iv. Continues to convert androgens secreted by theca luteal cells into estrogen e. Theca luteal cells develop from theca interna i. Form remaining 20% of cells ii. Secrete mostly androgens, but also progesterone iii. Found at periphery f. Progesterone feedback reduces production of LH and stops corpus luteum formation g. However, if pregnancy occur, corpus luteum continues to enlarge, promoted by Human Chorionic Gonadotropin from placenta h. If no pregnancy occurs, corpus luteum degenerates into Corpus Albicans i. Invaded by fine CT forms scar ii. Shrink with age, so largest ones are the youngest 8. Name the four parts of the uterine tube and distinguish their histological differences. Relate how the morphology integrates with its function. a. Infindibulum i. Finger like processes, “fimbriae” 1. Help “grab the ovulation” b. Ampulla i. Expanded region ii. Highly folded iii. Fertilization usually occurs here iv. Greatest number of cilia here 1. Sweep ovulated ovum into and down the ovarian tube c. Isthmus i. Narrow portion d. Intermural i. Portion traversing the uterine wall ii. Few cilia 9. Describe the regions and the layers of the uterus and relate the morphology to its function. a. Perimetrium i. Outermost (deepest) ii. Thin layer of dense CT iii. ** Peritoneum on fundus b. Myometrium i. Thickest layer of wall ii. Smooth muscle cells 1. Subdivided into 3-4 layers (longitudinal, middle=circular) 2. Difficult to discern layers 3. Increase in size during pregnancy 4. Contracts during intercourse or menstruation © 2009 Mark Tuttle 5. Under influence of prostaglandins and oxytocin 6. At cervical region, the muscle is replaced by elastic fibers – to allow more flexibility during childbirth c. Endometrium i. Mucosal layer of uterus ii. **simple columnar epithelium and lamina propria CT iii. Lines tubular glands (uterine glands) iv. Place for implantation of zygote v. Two layers 1. Functionalis layer a. Superficial b. Sloughed off during menstruation c. Composed of compacta (superficial) and spongiosa (deeper, spongey) 2. Basalis layer a. Deep layer b. Not sloughed off c. Epithelium and glands regenerate functionalis from here 10. Identify and contrast the main phases of the menstrual cycle. Describe the morphological changes in the endometrium during each phase of the menstrual cycle and integrate this with its functions. Indicate the principal hormones responsible for the morphology of each phase and from where they arise. a. Menstrual phase i. Days 1-5 ii. Functionalis layer sloughs off iii. Endometrium at thinnest iv. **Diagnostic features 1. Luminal surface is ragged 2. Stroma is full of blood 3. Mostly basalis left b. Proliferative phase(Follicular phase) i. Days 6-14 ii. Growth stage iii. Endometrium is responding to estrogen produced by growing follicles iv. Increase in size of functionalis layer of endometrium v. Increased length of uterine glands vi. Coiled arteries between glands vii. Increased CT viii. **Diagnostic features 1. Narrow lumen 2. Simple columnar epithelium 3. Uterine glands go from straight to wavy c. Secretory phase (Luteal or progravid phase) i. Days 15-27 ii. Uterine glands begin to actively secrete material to support zygote iii. Under influence of progesterone iv. **Diagnostic features © 2009 Mark Tuttle 1. Glands become coiled 2. Stroma CT between glands reduced 3. Gland lumens dilated with secretions 4. Coiled arteries not readily seen v. Functionalis layer may slightly decrease but this is not readily seen 11. Integrate the various hormones that impact and are produced by the female reproductive system and what effects they have on their target organs. Also be able to relate the control mechanism for these hormones. a. Progesterone i. Secreted by follicular layer (granular layer) of follicle and (to a minor degree) Theca luteal cells of corpus luteum ii. Acts on the corpus luteum to decrease leutenizing hormone (LH) 1. Stops corpus luteum formation iii. Maintains thick endometrium iv. Prepares uterus for implantation v. Peaks at day 25 of menstrual cycle vi. Act on receptors of smooth muscle cells in functionalis coiled arteries 1. Keep them open 2. When progesterone drops (natural part of menstrual cycle), coiled arteries close, endometrium functionalis becomes ischemic, sloughs off b. Follicle Stimulating Hormone (FSH) i. secreted by cells in anterior pituitary gland stimulates follicle growth ii. Follicular cells develop receptors for FSH beginning at puberty iii. At beginning of cycle, more than one follicle responds to FSH iv. Follicular Antrum filled with follicular liquor helps regulate FSH release v. Inhibited by high estrogen levels as when follicles are mature vi. Granulosal cells of corpus hemorrhagicus secrete folliculostatin & inhibin 1. act as inhibitors of FSH release c. Leutenizing Hormone (LH) i. Secreted by pituitary gland ii. Causes rupture of follicle, leading to ovulation iii. Causes release of Meiosis Inducing Substance iv. Acts on Corpus Hemorrhagicus to form Corpus Luteum v. Release is regulated by follicular liquor in the follicular antrum vi. Inhibited by progesterone (acts on pituitary gland) 1. When this starts to decrease, either menstrual cycle continues, OR pregnancy has occurred and Human Chorionic Gonadotropin (HCG) takes over and helps maintain corpus leuteum that would otherwise have degenerated d. Estrogen i. Inhibit FSH release ii. Causes LH surge iii. Produced by follicles/corpus luteum 1. Theca interna of secondary follicle produces androgens which are converted to estrogen by adjacent (deeper) granulosal cells © 2009 Mark Tuttle 2. Theca luteal cells also produce androgens which are converted to estrogen by adjacent granulosal luteal cells in corpus luteum 12. Describe the specific type of epithelium and the shape of glands found in the uterine cervix, as well as the epithelial lining of the vagina. Be able to contrast the morphology and function of the vagina with that of the esophagus. a. Cervix i. Lined by simple columnar epithelium (just like the uterus) ii. BRANCHED cervical glands (unlike uterine simple glands) iii. Mucous secreting b. Vagina i. Stratified squamous non-keritinizing epithelium transition here from simple columnar of uterus/cervix ii. NO layered muscularis externa (unlike esophagus circular/longitudinal) iii. NO glands in lamina propria (unlike esophagus) 13. Describe and integrate the blood supply and function of the ovary, endometrium and fallopian tube. a. The ovary is supplied by helicine vessels of the ovarian (gonadal) artery arising directly from the aorta and drained by the ovarian (gonadal) vein. It also supplies the fallopian tubes before anastomosing with the uterine artery i. The ovarian artery runs through the suspensatory ligament of the ovary which is a fold of peritoneum b. The endometrium is supplied by the coiled/straight arteries branching off of the radial arteries which branch off of the arcuate arteries running circumferentially around the uterus which branches off of the uterine artery which is a branch of the internal iliac artery i. The uterine artery runs through the Cardinal Ligament (Transverse cervical ligament) and meets the cervix supravaginally running through endopelvic fascia 14. Identify the components of the breast. Explain how the morphology of the breast changes from the resting state to the active state (lactation). a. Inactive i. Small amounts of glandular tissue/ducts ii. Mostly adipose iii. No milk being produced b. Active i. Mostly glandular tissue producing milk ii. Stimulated by estrogen and progesterone during pregnancy to form alveoli iii. Stimulatd by prolactin secreted by the pituitary gland to produce milk iv. Sucking on nipple sends neural signal to hypothalamus, causes release of oxytocin v. Oxytocin secreted from pituitary lgland causes myoepithelial glands to contract vi. Glandular units form alveoli 1. Lined by simple cuboidal epithelium 2. Wrapped in myoepithelial cells 3. Alveoli produce IgM (clostrum) prior to birth © 2009 Mark Tuttle 15. Be able to relate and integrate the types and modes of secretions from the various female reproductive organs with their functions. a. Ovary i. Cytocrine: whole cell secretion b. Uterus i. Mucoid secretions to help the sperm reach the ovary c. Vagina i. No secretions from glands but non-keritinized stratified squamous so some water can get through 16. Be able to relate where and when fertilization and implantation normally occur. a. Implantation should occur in the endometrium b. Fertilization should occur in the oviduct (Fallopian tube) granulosa cells zona pellucida lactiferous duct antrum cumulus oophorus lactiferous sinus theca interna theca externa colostrum menarche menopause milk ejection reflex germinal epithelium tunica albuginea ectopic pregnancy follicular cells primary & secondary oocyte gonorrhea corpus hemorrhagicus corpus albicans endometriosis coiled arteries straight arteries cervical cancer © 2009 Mark Tuttle Autonomic Innervation of Abdominal and Pelvic Viscera – CBC 1. Review the basic organization of the sympathetic and parasympathetic division of the ANS. a. 2. What is the general organization of sympathetic innervation to abdominal viscera? a. Follows blood supply b. Celiac i. T5-T9 spinal cord level ii. Greater splanchnic n. iii. Synapse at Celiac prevertebral ganglia iv. Postganglionic neuron goes to foregut structures c. Superior Mesenteric i. T10-T11 spinal cord level ii. Lesser Splanchnic n. iii. Synapse at superior mesenteric prevertebral ganglia iv. Postganglionic neuron goes to midgut structures d. Aorticorenal i. T12 spinal cord level ii. Least splanchnic n. iii. Synapse at aorticorenal prevertebral ganglia iv. Postganglionic neuron goes to kidney, gonads, suprarenals e. Inferior Mesenteric 3. Describe the following terms: a. thoracic splanchnic i. All the splanchnic nerves that originate from thoracic spinal cord levels 1. Greater splanchnic (T5-T9) 2. Lesser Splanchnic (T10-T11) 3. Least Splanchnic (T12) 4. NOT lumbar splanchnic b. lumber splanchnic i. Not thoracic ii. L1-L2 origin iii. Inferior mesenteric iv. Hindgut c. prevertebral ganglia i. sympathetic ganglia which lie between the sympathetic chain and the organ of supply d. paravertebral ganglia i. Ganglia along the length of the sympathetic trunk 4. Describe the details for sympathetic innervation for all viscera of the abdomen. a. Follows the blood supply b. Follows embryonic origin 5. What is the distribution of the vagus nerve in the abdomen? Describe the formation and distribution of pelvic splanchnic nerves. a. Vagus n. i. Vagus nerve (CN 10) supplies organs supplied by Celiac Trunk and Superior Mesenteric Artery (Foregut & Midgut) © 2009 Mark Tuttle ii. Appears to run with the postganglionic nerves of the celiac/superior mesenteric ganglia of the sympathetic division iii. ALSO supplies the kidneys + gonads b. Pelvic Splanchnic N. i. Parasympathetic ii. Originate at S2-S4 spinal cord levels iii. Supply the organs of the inferior mesenteric artery iv. Hindgut v. Synapse at terminal ganglia intimate with the effector and give off short branches which make up the pelvic plexus 6. What is the basic organization of sympathetic innervation to pelvic viscera? a. Lumbar splanchnic n. (L1-L2) i. to the aortic plexus, then to the superior hypogastric plexus, then along the Inferior Hypogastric nerve where it synapses at an unnamed ganglia and gives off postganglionic branches in the inferior hypogastric plexus and innervates pelvic structures (i.e. bladder) ii. OR, just run directly to the inferior hypogastric plexus and synapse b. Sacral splanchnic (L1-L2) i. Travels down the sympathetic trunk and synapses at a PARAvertebral ganglion at ~sacral region where it gives off the postganglionic SACRAL SPLANCHNIC n. ii. Travels to the hypogastric plexus where it innervates the bladder. 7. Describe the following terms: superior hypogastric plexus, hypogastric nerve, inferior hypogastric plexus and sacral splanchnic. a. See above 8. What is the basic organization of parasympathetic innervation to pelvic viscera? a. Originates at S2-S4 b. Travels in pelvic splanchnic n. i. Note parasymp splanchnics are named by target region NOT origin c. Travels to terminal ganglia in inferior hypogastric plexus © 2009 Mark Tuttle Gluteal Region and Posterior Thigh – Morse 1. Describe the dermatome pattern for the lower limb. a. Anteriorly, it is mostly L1-S1 i. L1 is all of the UG triangle ii. L4 is most of the thigh and knee iii. L5 comes in across the shin iv. S1 is the lateral parts of the ankle and little toe b. Posteriorly i. S5 is the anus and extending out around the anus in concentric circles is S4 and S3 ii. L5 is the lateralmost parts of the thigh and part of the leg iii. S1 is the middle of the thigh and leg 2. Demonstrate the sacrotuberous and sacrospinous ligaments and describe how they contribute to the formation of the sciatic foramina. a. Sacrotuberous i. Sacrum to ischial tuberosity b. Sacrospinous i. Sacrum to ischial spine c. Greater sciatic foramen i. Greater sciatic notch + sacrospinous lig (+ maybe some sacrotuberous lig) ii. Houses Pisiform m. d. Lesser sciatic foramen i. Lesser sciatic notch + sacrotuberous + sacrospinous 3. Review the anatomy of the bones of the pelvis and the femur. 4. Demonstrate the surface anatomy of the sciatic nerve. a. L4-S3 b. Leaves the greater sciatic foramen just below Piriformis, but above Superior Gamellus i. (superior gamellus does not travel through GSF, instead takes its origin on the outside of the ischial spine) c. Runs down the posterior aspect of the thigh along with the posterior cutaneous n of the thigh i. superficial to superior gamellus, obturator internus, inferior gamellus, obturator externus, quadrates femoris ii. deep to Gluteus Maxiumus d. The Posterior cutaneous n of the thigh dives deep, away from sciatic at about the ischial tuberosity (common origin of hamstrings) e. Dives deep to the long head of biceps femoris f. Splits at the politeal fossa into common fibular and tibial nn. 5. Demonstrate the large gluteal muscles and understand their role in gait as well as their nerve and blood supply. a. Gluteus mm are not heavily used in walking on a flat surface b. They do perform the tipping of the pelvis which is essential to a normal gait while walking c. Gluteal mm. are recruited and used heavily when running, climbing, and rising from a seated position 6. Describe the course structures take from the pelvic cavity to the gluteal region. © 2009 Mark Tuttle a. Out the greater sciatic foramen i. Piriformis ii. Sciatic n iii. Posterior cutaneous n of thigh iv. Superior gluteal a + n (superior to piriformis) v. Inferior gluteal a + n vi. N. to obturator internus vii. N. to quadratus femoris b. Out the lesser sciatic foramen i. Tendon of Obturator internus . c. Obturator canal (through the obturator fascia in the foramen) i. Obturator n. + a. + v. 7. Demonstrate the six lateral rotator muscles of the hip. a. Facts i. All insert on the greater trochanter ii. All innervated by small individual branches of the sacral plexus b. Muscles i. Pisiform m. ii. Superior Gamellus m. iii. Obturator internus m. iv. Inferior Gamellus m. v. Obturator externus m. vi. Quadratus femoris m. 8. Understand the course structures take from the gluteal region to the perineum. a. Out of the pelvis through the greater sciatic foramen, back in to the perineum through the lesser sciatic foramen , then enters the pudendal canal, made up of Obturator Internus fascia before entering the perineum b. Contents i. Internal pudendal artery ii. Internal pudendal veins iii. Pudendal nerve 9. Define the hamstring muscle group and delineate their actions, nerve supply, and blood supply a. Requirements i. Originate on the Ischial Tuberosity ii. Innervated by the Tibial N. © 2009 Mark Tuttle Thigh and Leg – Morse - Identify the bones of the thigh and leg and the major anatomical features of each. a. Thigh i. Femur 1. Head: articulates with the acetabulum of the pelvis 2. Greater trochanter is on the posterolateral side 3. Lesser trochanger is on the posteromedial side 4. Pectineal line: distal attachment of pectinius – runs between lesser trochanter and the linea aspera 5. Gluteal tuberosity 6. Linea aspera runs down the middle of the posterior side and splits into medial/lateral supracondylar lines a. Exposes Popliteal surface 7. Medial/Lateral condyles 8. Adductor tublercle on medial aspect of distal epiphysis b. Leg (FLorida TradeMark) i. Tibia: larger, medial 1. Tibeal plateau articulates with condyles of the femur a. (there are also condyles of tibia) 2. Intercondylar eminence comes up between plateaus 3. Articulates with fibula on lateral condyle 4. Shaft 5. Medial malleolus: process which sticks downward ii. Fibula: smaller, lateral 1. Does NOT articulate with knee 2. Shaft 3. Lateral malleolus: process which sticks downward - Define the boundaries and the contents of the femoral triangle. a. Boundaries i. Inguinal ligament (superior) ii. Sartorius m. (lateral) iii. Adductor longus m. (medial) iv. Iliopsoas m. + pectinius m. (posterior) b. Contents (NAVL – lateral to medial) i. Femoral n. ii. Femoral a. iii. Femoral v. iv. Femoral ln. - Explain the anatomy of a femoral hernia and distinguish it from the inguinal hernias. a. Goes into the femoral triangle and a portion can go through the saphenous opening and because - Demonstrate the course and the primary branching pattern for major vessels and nerves of the thigh and leg. a. Nerves i. Anterior 1. Femoral n. a. Muscular branches innervate i. Iliopsoas m. © 2009 Mark Tuttle ii. Pectineus m. iii. Sartorius m. iv. Quadriceps femoris mm. b. Cutaneous i. Anterior cutaneous branch ii. Saphenous n. (medial part of leg) 2. Obturator n. a. Runs through obturator foramen and superior/superfiscial to obturator externus b. Superficial to adductor brevis, but deep to aductor longus c. Innervates i. Obturator externus ii. Adductor longus iii. Adductor brevis iv. Adductor magnus v. Gracilis vi. Pectineus 3. Lateral cutaneous n. of thigh a. Branches off of Genitofemoral b. Pierces through fascia lata laterally and supplies the skin ii. Posterior 1. Medial cutaneous innervation is provided by dorsal rami of L1,2,3 and S1,2,3 a. Superior/middle/inferior cluneal nn. 2. Superior gluteal n. (L4-L5) a. 3. Sciatic n. and Posterior cutaneous n. of thigh a. run parallel and then posterior cutaneous n of thigh dives deep at about the level of the origin of biceps femoris long head (sciatic also deep to biceps, but not as deep) b. Innervates i. Semitendinosus ii. Semimembranosus iii. Biceps femoris (long head) iv. Adductor magnus (medial part) c. Branches above the popliteal fossa into: i. Tibial n. 1. Along tibia ii. Common Fibular n. 1. Along fibula b. Veins i. Femoral v runs along with femoral a. 1. Small saphenous v. on posterior part of leg runs up and dumps into popliteal vein at the popliteal vossa. ii. Great Saphenous v. parts with femoral v. at saphenous hiatus and runs down the medial aspect of the thigh and the leg 1. runs with saphenous n. in the leg © 2009 Mark Tuttle 2. posterior tibial and fibular vv. run along and meet with popliteal v. and short saphenous before rising superficially through the adductor hiatus becoming the femoral v. - - - - c. Arteries i. Femoral artery 1. Leaves pelvis deep to the inguinal ligament and enters the femoral triangle 2. Gives off the Profunda Femoris A. which supplies the entire posterior compartment of the thigh via perforating arteries 3. Enters the Subsartorial/Adductor/Hunter’s Canal Identify arteries of the lower limb from which a pulse may be palpated. a. Femoral triangle b. Popliteal fossa c. Dorsum of foot between: (on foot between 1 + 2 toes) i. Extensor halicus longus m. ii. Extensor digitorum longus m. Describe the course of the major superficial veins of the lower limb. a. See above List the contents of the subsartorial canal. a. Femoral A + V b. Branches of Femoral N. – most notably the saphenous n. Demonstrate the muscles found in each anatomical “compartment” of the thigh and leg. a. See sheet Describe the nerve and blood supply for muscles of the thigh and leg. a. See above Define active and passive insufficiency as it relates to muscles. a. Active insufficiency i. When a muscle is unable to exert maximal force on a joint because it cannot be shortened enough to cause full range of motion of both of the joints it crosses at the same time b. Passive insufficiency i. When a muscle is unable to exert maximal force on a joint because it cannot be stretched enough to cause full range of motion of both of the joints it crosses at the same time Define the major actions of muscles acting on the hip, knee, ankle and digital joints. a. Hip i. Flex 1. Iliopsoas mm. a. Psoas major b. Psoas minor (accessory) c. Iliacus muscle 2. Anterior compartment of thigh a. Rectus femoris. (Part of the Quadriceps.) b. Sartorius 3. Medial compartment of thigh a. Pectineus b. Adductor longus c. Adductor brevis © 2009 Mark Tuttle d. Gracilis 4. (Tensor fasciae latae) ii. Extend 1. Hamstrings a. Semimembranosus b. Semitendonosus c. Biceps Femoris (long head) 2. Gluteus maximus recruited under certain circumstances iii. ADduct 1. Adductor brevis 2. Adductor longus 3. Adductor magnus 4. Pectineus 5. Gracilis iv. ABduct 1. Gluteus Medius 2. Gluteus Minimus 3. Gluteus Maximus 4. Piriformis 5. Obturator externus v. Medial Rotation 1. Tensor fasciae latae 2. Gluteus medius 3. Gluteus minimus, anterior fibers vi. Lateral Rotation 1. Gemellus superior 2. Gemellus inferior 3. Obturator internus 4. Obturator externus 5. Quadratus femoris b. Knee i. Extend 1. All anterior compartment of thigh a. Quadriceps femors i. Vastus medialis ii. Vastus lateralis iii. Vastus intermedius iv. Rectus femoris b. Sartorious ii. Flex 1. All posterior compartment of thigh a. Hamstring mm. i. Semitendonosus ii. Semimembranosus iii. Biceps femoris (long head) b. Biceps femoris (short head) c. Sartorius 2. Gracilis © 2009 Mark Tuttle 3. Popliteus 4. Gasrocnemius - - - c. Ankle i. Plantarflex 1. Posterior Superficial compartment of leg a. Gastrocnemius b. Soleus c. Plantaris (only weak participation) 2. Posterior Deep compartment of leg a. Flexor hallucis longus b. Flexor digitorum longus c. Tibialis posterior ii. Dorsiflex 1. Anterior compartment of leg a. Tibialis Anterior b. Extensor hallucis longus c. Extensor digitorum longus 2. Peroneus Tertius iii. Evert 1. Fibularis longus 2. Fibularis brevis iv. Invert 1. Tibialis anterior 2. Tibialis posterior Define the boundaries of the popliteal fossa and describe its contents. a. Boundaries i. Superior-lateral: Biceps femoris (both heads) ii. Superior-medial: Semimembranosus, semitendonosus iii. Inferior-lateral: Gastrocnemius iv. Inferior-medial: Gastrocnemius b. Contents i. Popliteal a. + v. ii. Sciatic n. ends and splits here into: 1. Tibial n. 2. Common fibular n. Describe the relationship of muscles, vessels and nerves as they cross the ankle to enter the foot. a. Posterior i. Tom Dick ANd Harry (from medial to lateral) 1. Tibialis Posterior m. 2. Flexor Digitorum Longus m. 3. Posterior Tibial A. 4. Posterior Tibial N. 5. Flexor Hallicus Longus m. Describe the vessels involved in collateral circulation for the hip, knee and ankle. a. Hip i. Lateral circumflex femoral a. (branch of profunda femoris) ii. Medial circumflex femoral a. (branch of profunda femoris) © 2009 Mark Tuttle b. Knee i. Genicular aa. 1. Lateral inferior/superior 2. Medial inferior/superior c. Ankle i. Anterior lateral malleolar a. ii. Anterior medial malleolar a. © 2009 Mark Tuttle Development of the Reproductive System – Crissman 1. Define/describe: Urogenital sinus (three portions) - Mesonephric duct (Wolffian duct) - Paramesonephric duct (Muellerian duct) - Uterovaginal primordium - sinovaginal bulb - Vesicle portion a. bladder Pelvic portion a. Membranous and prostatic urethra Phallic portion a. Penile urethra Males: Develops into everything between testis and prostate Females: degenerates into Epoopheron (homolog of epididymis) Formed during 6th week Females: develop into Fallopian tubes, uterus, and the upper portion of the vagina Males: degenerate into prostatic utricle Develops from fusion of Mullerian (Paramesonephric) ducts Bulge out at sinus tubercle As duct migrates, drags tissue, vasculature with it, forming broad ligament Necessary signals: a. Absence of testosterone b. Absence of Mullerian-inhibiting factor c. Wnt-4 d. Wnt-7a e. Hoxd 10-13 - Where the fused Mullerian ducts meet the uterus and stimulate proliferation of endoderm Canalization moves from posterior to anterior primary sex cords - Thickening of coelomic epithelium In 6th week, primordial germ cells get embedded here Cortical cords (secondary sex cords) - Germ cells become embedded, remain in outer region Oogonia undergo mitosis seminiferous tubule - Formed from gonadal cord ovarian follicle - Ovary at 2 weeks contains ovarian follicles tunica albuginea - Forms around invading germinal cells in gonadal cord In females, forms at the corticomedullary junction of the fetal ovary 2. Describe the situation (location) of the embryonic gonad as it begins its development. What is the origin of the autonomic innervation and vascular supply of the developing gonad (both blood and lymphatic)? © 2009 Mark Tuttle a. Testis formation starts from indifferent gonad in gonadal ridge under the influence of TDF b. This occurs during the 7th week c. Initial descent i. Due to testosterone ii. Cranial suspensory ligament regresses iii. Mesonephric kidney degenerates d. Transabdominal descent i. Testes descend to level of deep inguinal ring ii. Insl-3 + testosterone essential e. Transinguinal descent i. Under influence of testosterone + gubernaculum ii. Through to superficial ring by 26th week f. Innervation i. The nerves of the ovary descend along the ovarian vessels from the ovarian plexus. ii. It is formed from the aortic, renal, and superior and inferior hypogastric plexuses. iii. These nerves supply the ovaries, broad ligaments, and uterine tubes. iv. The parasympathetic fibres in the ovarian plexus are derived from the vagus nerves. 3. Describe the origin and migratory path of the primordial germ cells. a. See #5 4. Explain the roles of the SRY locus, Testis Determining Factor, androgenic hormones, Anti-Muellerian Factor (or Muellerian Inhibiting Substance), in development of the reproductive systems. a. SRY locus i. Results in expression of TDF (testis-determining factor) which is essential for male gonad development b. Anti-Mullerian factor i. Secreted by fetal Sertoli cells ii. Causes involution of female ducts 5. Describe the migration of coelomic epithelial (mesothelial) cells into the mesenchyme of the gonad to produce the primary sex cords in the testes and the primary and secondary sex cords in the ovary. What ultimately develops from each generation of cords? a. Germ cells migrate into urogenetal ridge during 5th week b. Originate from endoderm of yolk sac c. Coelomic epithelium proliferates and forms Primary sex cord d. During 6th week, germ cells are embedded into gonadal cords e. Germ cells proliferate to up to millions f. LIF, STEEL signal proliferation g. TDF signals testis formation h. All mature male structures develop from primary gonadal cords i. If TDF is absent, females form cortical cords (Secondary gonadal cord) j. Germinal cells become embedded in outer region, undergo mitosis k. Female mature structures develop from secondary gondal cords © 2009 Mark Tuttle 6. What are the components and origin of each component of the seminiferous tubule, straight tubules, rete testes, efferent ductules, ductus epididymis, ductus deferens? a. Seminiferous tubule Outer gonadal cord b. Straight tubule, Rete testes Inner portion of gonadal cord c. Epididymis Mesonephric duct d. Efferent ductules, vas deferens Mesonephric duct 7. Describe the formation of the seminal vesicle and the prostate. a. Testosterone is essential b. Secreted by interstitial cells of Leydig c. Induces distal mesonephric duct to become highly convoluted to form Epididymis as well as Ductus Deferens, Ejaculatory Ducts & Seminal Vesicles d. Hox genes play role in transformation 8. What is the origin of the interstitial cells of the testis, theca interna of the ovarian follicle, interstitial gland of the ovary? a. Leydig i. Mesenchyme differentiates into Interstitial Cells of Leydig that lodge between the seminiferous tubules ii. Appear about 8th wk b. Theca interna i. Forms as follicle becomes tertiary c. Interstitial gland of ovary i. Forms from the theca interna of an atretic follicle. Secretes androgens to become estrogen 9. What is the primary determinant of genotypic (genetic) and phenotypic (morphologic) sex in humans? a. Genetic: Y chromosome b. Phenotypic: TDF (testis determining factor) 10. What substance (hormones) does the embryonic testis produce? What does each substance do in the body? a. Testosterone secreted by fetal Leydig cells, stimulated by human chorionic gonadotropin b. Mullerian inhibiting substance (MIS) secreted by sertoli cells causes involution of female ducts c. Meiosis inhibiting factor (MIF) secreted by sertoli cells, slows spermatogenesis i. Essential for sertoli cells to receive Sox-9 for this to happen. Otherwise, ovary forms 11. Why does the testis use a duct system and the ovary does not? a. Far larger number of sperm are produced, and produced continuously 12. Describe the site of formation and the method of formation of the paramesonephric ducts. a. Formed during 6th week b. Longitudinal invagination of coelomic mesothelium on surface of urogenital ridge lateral to the mesonephric duct c. Grows caudally to reach urogenital sinus between entrance of mesonephric ducts d. Initially doesn’t open into urogenital sinus 13. Describe the path or route of development of the paramesonephric ducts. a. See above © 2009 Mark Tuttle 14. Describe the formation and fate of the a. uterovaginal primordium i. Two mullerian (paramesonephric) ducts fuse together ot form this ii. Gives rise to both uterus and vagina b. sinus tubercle i. Bulge into the urogenital sinus from above structure c. sinovaginal bulbs i. 2 of these form from the proliferation of endoderm at the urogenital sinus at the point of the sinus tubercle (Mullerian ducts [paramesonephric]) met at this point d. vaginal plate i. Fused sinovaginal bulbs ii. Canalization of this moves posterior to anterior, forms single vagina e. Hymen i. Seperates urogenital sinus from the lumen of the vagina 15. Define/describe: a. labioscrotal swellings (genital swellings) i. Flank the genital folds laterally ii. Part of the indifferent external genetalia iii. Indifferent period lasts until 7th week b. urogenital folds (urethral folds) i. 2 of these surround the clocal membrane ii. Covered by urogenital sinus endoderm iii. Penile urethra formed by fusion of folds iv. Surface ectoderm covers closure c. genital tubercle i. develops from the genital eminence ii. Forms the primordial Phallus d. phallic portion of urogenital sinus i. Under influence of testosterone, forms penis e. cloacal membrane i. Remains intact until 8th week f. urogenital membrane i. Urorectal septum fuses with cloacal membrane at end of 6th week ii. Divides clocal membrane into anterior urogenital membrane, and posterior anal membrane iii. Occurs during 6th week iv. Both membranes degenerate the following week 16. Describe the complete formation of the male urethra. a. Urogenital folds enlarge under the influence of testosterone and dihyrotestosterone to form lateral walls of urethral groove b. Covered by urogenital sinus endoderm c. Grooves fuse posterior to anterior d. Surface ectoderm covers closure e. Urethral seam forms f. Solid plate recanalizes and loses its connection to surface (forms hole) g. Corpus cavernosa/spongiosa develop from mesenchyme 17. Define: © 2009 Mark Tuttle 18. 19. 20. 21. 22. a. true hermaphrodite i. Have barr bodies (sex chromatin positive) ii. Have both ovarian and testicular tissue that is non-functional iii. Extremely rare iv. Can be XX, XY, XX/XY mosaic b. Pseudohermaphrodite i. Can be male of female ii. Female/male determined by sex chromatin barr bodies and genotype iii. Female pseudo have enlarged clitoris iv. Male pseudo have low testosterone 1. Lack of MIS causes perseverance of female ducts c. What are several causes of pseudohermaphrodism? i. Female pseudo 1. Excessive androgens as in congenital adrenal hyperplasia (CAH) ii. Male pseudo 1. Low levels of testosterone and MIS Define/describe the condition known as testicular feminization. Developmental error? a. Chromatin negative b. XY c. Female external gentalia, uterus ends in blind pouch d. Have female secondary sex characteristics i. Estrogen from conversion of androgens produced by adrenal cortex. Conversion occurs in adipose tissue e. Defect in androgen receptors in genital tubercle, urogenital, labioscrotal folds f. However, uterus, oviducts missing due to successful secretion of MIS by testis Define/describe the condition of hypospadias; epispadias. Developmental error for each? a. Hypospadia i. Most common anomaly of penis 1/300 ii. Opening of external urethral orifice on ventral surface iii. Inadequate production of androgens b. Epispadia i. Same thing but when it occurs down the entire length of penis Describe the underlying developmental errors leading to complete or partial duplication of the uterus and/or vagina. a. Incomplete fusion of Mullerian (paranephric) ducts leads to double uterus b. Incomplete recanalization of sinovaginal plate yields to double vagina Describe the formation of the inguinal canal. a. Inguinal canal forms in both sexes at indifferent stage of development, 7th week b. Created by gubernaculum Describe the process and path of migration of the testis and ovary a. Testis i. See #2 b. Ovary i. They descend along the posterior abdominal wall. ii. On reaching the pelvic brim, the ovarian arteries cross over the external iliac vessels and enter the suspensory ligaments. © 2009 Mark Tuttle Male Reproductive System – Crissman 1. List the organs and ducts of the male reproductive system. a. Organs i. Penis ii. Testes b. Ducts i. Straight tubules ii. Rete testis iii. Efferent ducts iv. Ductus epidydimus v. Ductus deferens vi. Ejaculatory duct vii. Urethra 2. Describe and integrate the components and their morphology of the testis with the function of the testis. a. Lined by germinal epithelium contains spermatogenic cells b. Sertoli cells form the blood-testis barrier c. Straight tubules drain the seminiferous tubules and are lined by simple cuboidal epithelium d. Same in rete testis e. Effecret ductules goes from rete testis to head of epididymis i. Cogwheel lumen ii. Contains ciliated cells to move immotile sperm iii. Contains non-ciliated cells to resorb water f. Epididymis contains Pseudostratified columnar epithelium (transitions to cuboidal toward tail) i. Tall columnar cells with stereocilia ii. Stem cells for principle cells (above) iii. Smooth muscle here moves sperm since stereocilia are immotile g. Ductus deferens i. Stellate lumen ii. Pseudostratified low columnar epithelium iii. Thick lamina propria iv. 3 layer muscularis (long, circular, long) 3. Describe the process of spermatogenesis and indicate how it differs from oogenesis. Distinguish "spermatogenesis" from "spermiogenesis". a. Spermiogenesis is the transition from spermatids to spermatozoa (last step) b. Spermatogenesis is the whole process c. Spermatogenesis does not get arrested at a certain stage like oogenesis does 4. Describe and identify the adluminal and basal compartments of the seminiferous tubules a. Adluminal i. Everything adjacent to lumen of ST b. Basal i. Contains spermatogonia ONLY 5. Describe, in detail, the morphology and function of the epithelium in the seminiferous tubules including the different germ cells and the Sertoli cell. Identify the phases of spermatogenesis. © 2009 Mark Tuttle 6. 7. 8. 9. a. Spermatogonia i. **Located on basement membrane of tubule (on basal side of blood-testis barrier) ii. Darker is stem cell b. Primary spermatocytes i. Most common cell ii. **See clumped chromosomes iii. Diploid c. Secondary spermatocytes i. Haploid d. Spermatid i. **round, solid, dark chromatin pattern e. Spermatozoa i. **head & long tail ii. Still embedded in cell but near lumen of ST f. Sertoli cells i. Provide physical/nutritional support for developing sperm ii. Joined by tight junctions iii. Tall columnar iv. Rest on basement membrane and reach lumen of ST v. Produce large volumes of testicular fluid to wash immobile spermatozoa out of tubule vi. Phagocytose excess cytoplasm from spermatids Explain what is meant by the "cycle of seminiferous epithelium". a. Cross-section of a tubule showing the proliferation that is occurring b. Waves are looking down the length of the tubule Describe and integrate the hormonal secretions that control the development and maintenance of the normal male reproductive system. a. Anterior pituitary i. FSH 1. Targets sertoli cells to produce Androgen Binding Protein (ABP) which targets testosterone to make it persist 2. Inhibin is produced by sertoli cells and feedsback on the anterior pituitary to reduce release of FSH ii. LH 1. Targets Leydig cells to produce more testosterone 2. Testosterone feedsback and inhibits Leydigs Describe the specific epithelial lining of the tubuli recti, rete testis, efferent ductules, epididymis, ductus deferens and ejaculatory duct. Identify examples of each and be able to integrate their morphology with their function. a. See #2 Describe and integrate the morphology and function of the seminal vesicles, prostate and bulbourethral glands. Be able to list characteristics necessary to distinguish one from the other. Explain the clinical significance of the mucosal glands, submucosal and main glands of the prostate. a. Seminal vesicle i. **numerous cavities of varying sizes – honeycomb ii. Low pseudostratified columnar (like proximal efferent ductules) © 2009 Mark Tuttle iii. Testosterone-dependent iv. Makes up 70% of ejaculate b. Prostate i. Mucosal glands 1. Drain directly into urethra 2. Located directly proximal to urethra 3. Undergo hypertrophy in BPH ii. Submucosal glands 1. Drain into prostatic sinus iii. Main glands 1. Most peripherally located 2. Makes up most of gland 3. Most prostatic cancer arises here c. Bulbourethral glands (Cowper’s glands) i. Simple cuboidal epithelium that secretes viscous mucus d. Glands of Littre i. Mucus-secreting glands along the penile urethra 10. Describe the morphology of the penis including the fascial layers, erectile tissue, blood vessels, as well as, the site and epithelial lining of the penile urethra. Be able to relate and integrate the morphological components of the penis in the flaccid and erect condition. a. Unnecessary – know this well 11. Be able to trace the normal pathway of sperm secretion. Be able to describe the morphology of the pathway and how it relates to the specific function of each part. a. Seminiferous tubules b. Straight tubules c. Rete testis d. Efferent ductules e. Epididymis (head) f. Vas deferens g. Ejaculatory duct (meet with secretions of seminal vesicle) h. Prostatic urethra (meet with secretions of prostate) 12. Describe the process of ejaculation and integrate it with the function of the various male reproductive components. a. Bulbourethral i. Part of pre-ejaculate to help neutralize acidity and clean out penile urethra b. Prostate i. Lipids ii. Proteolytic enzymes iii. Citric acid iv. Acid phosphatase v. pH near 7 (raises pH of vagina) c. Seminal vesicle i. Fructose tunica albuginea (testis & penis) - Dense CT covering covers entire testis Surrounds each erectile body in penis tunica vaginalis - Covers tunica albuginea everywhere except when in contact with © 2009 Mark Tuttle epididymis and where vessels enter mediastium testis - CT which supports the rete testis germinal epithelium - In males, the epithelium lining the STs with the range of sperm development and sertoli (support) cells androgen-binding protein - Sertoli cells secrete this in response to FSH from the anterior pituitary. Helps testosterone persist thereby raising the circulating level of testosterone, aiding in spermatogenesis Spermatogonia - The first stage of sperm development Diagnostic on the basement membrane, outside of the bloodtestes barrier primary & secondary spermatocytes - Primary spermatocytes are diploid and display clumped chromosomes Secondary spermatocytes are haploid and are hard to distinguish Spermatids - Round, solid dark chromatin pattern Don’t have flagella yet Spermatozoa - Have flagella now seminal colliculus - In the fore part of the urethral crest, containing o Ejaculatory ducts o Prostatic ducts o Prostatic utricle Cowper’s glands - AKA bulbourethral glands Component of pre-ejaculate that helps clean out the urethra Utricle - AKA vagina masculine Remnant of Mullarian duct (Paramesonephric duct) pampiniform plexus - Plexus of veins which help cool the blood going to the testicle to maintain it at an optimal temperature. Work by cooling the adjacent arterial blood. blood testis barrier - Formed by Sertoli cells Leydig cells - AKA interstitial cells Foamy appearance because of secreting steroid testosterone Vasectomy - Cutting the vas prostatic hypertrophy - Benign hypertrophy occurs in the middle lobe prostatic concretions - Diagnostic for an older prostate Composed of layered bodies, red staining Impotence - Unable to achieve errection Sterile - Less than 20 million sperm/ml Normal is 66-100 million sperm/ml Ejaculation 1. Bulbourethral, prostatic secretions 2. Emission – seminal vesicle contracts 3. Bulbospongiousus muscle contracts © 2009 Mark Tuttle Foot – Morse 1. Demonstrate the relationship of extrinsic foot muscles to nerves and vessels of the foot. a. Dorsum i. Extensor Hallucis Longus tendon 1. Deep fibular n. innervates the skin between toes 1 & 2 2. Anterior tibial a. b. Plantar i. Flexor digitorum longus tendon 1. Tibial n. 2. Posterior tibial a. (entire plantar foot) a. Lateral plantar a. b. Medial plantar a. c. Notable absences i. Fibular a. doesn’t do shit in the foot 2. Understand the function of intrinsic foot muscles. Adductor hallucis (oblique head) Keep the toes from splaying Adductor hallucis (transverse head) Abductor digiti minimi m. ABduct 5th toe Abductor hallucis m. ABduct 1st toe Flexor hallucis brevis m. Flex 1st toe Quadratus plantae m. Redirect pull of Flexor hallucis longus to just flex toes, not invert Lumbrical mm. Flex metatarsals Extend intermetatarsal joints Dorsal interosseous mm. ABduction Plantar interosseous mm. ADduction 3. Define the arches of the foot and understand how each is maintained. a. Lateral longitudinal arch i. Less prominent than medial ii. Deltoid ligament (Medial collateral ligament) 1. Tibiocalcaneal lig. 2. Anterior tibiotalar lig. 3. Posterior tibiotalar lig. 4. Tibionavicular lig. b. Medial longitudinal arch i. Components: calcaneus, the talus, the navicular, the three cuneiforms, and the first, second, and third metatarsals ii. Lateral Collateral 1. Posterior talofibular lig. 2. Calcaneofibular lig. 3. Anterior talofibular lig. © 2009 Mark Tuttle 4. 5. 6. 7. c. Transverse arch i. Adductor halucis (transverse & oblique heads) prevents toes from splaying d. Factors in arch strength i. Intrinsic muscle strength Tie beam (spreads weight) ii. Extrinsic muscle strength Suspension cable iii. Ligament strength Staples iv. Talus strength Keystone Define the role of the plantar aponeurosis. a. Helps maintain integrity of the arch of the foot b. Acts as a tie beam c. Tear of this leads to plantar fasciitis d. Divides the sole of the foot into lateral, intermediate, and medial compartments Understand the communication of dorsal and plantar arteries of the foot. a. The dorsal a. of the foot gives off a deep plantar a. which dives deep to the sole between the 1st and 2nd toes b. Deep plantar a. supplies the dep plantar arch Identify the retinacula of the ankle region. a. Superior Extensor retinaculum i. Extensor digitorum longus ii. Extensor hallucis longus iii. Fibularus tertius iv. Tibialis anterior v. Anterior tibial a. + v. vi. Deep Fibular n. b. Inferior extensor retinaculum c. Flexor retinaculum d. Fibular retinaculum i. Covers fibularis longus and brevis as they come into the foot ii. Brevis stops and attaches the the tuberosity of the 5th digit Describe the sensory innervation for the foot. a. Dorsum i. Superior fibular n. ii. Deep fibular n. b. Planta i. Medial plantar n. (Tibial n.) ii. Lateral plantar n. (Tibial n.) c. Lateral i. Sural n. (Follows short saphenous v.) d. Medial i. Saphenous n. (Follows long saphenous v.) © 2009 Mark Tuttle Joints of the Lower Limb 1. Identify the major extra and intracapsular ligaments for the hip, knee and ankle. a. Hip i. Intracapsular 1. Ligament of head of femur (Fovea) a. A. of head of femur (Obturator a.) runs here ii. Extracapsular 1. Iliofemoral lig. (Y-ligament) 2. Ischiofemoral lig. 3. Pubofemoral lig. b. Knee i. Intracapsular 1. Patellar lig. 2. Tibial (medial) collateral lig. (MCL) 3. Fibular (lateral) collateral lig. a. Intrinsic only b/c it is intimate with the capsule at the superior portion. Popliteus tendon is deep to it at lower portion 4. Oblique politeal lig. 5. Arcuate popliteal lig. 6. Anterior cruciate ligament (ACL) 7. Posterior cruciate ligament (PCL) 8. Lateral meniscus 9. Medial meniscus 10. Transverse ligament of knee ii. Extracapsular c. Ankle i. Deltoid ligament (medial) 1. Anterior tibiotalar lig. 2. Posterior tibiotalar lig. 3. Tibiocalcaneal lig. 4. Tibionavicular lig. ii. Lateral collateral ligament 1. Anterior fibulotalar lig. 2. Posterior fibulotalar lig. 3. Fibulocalcaneal lig. 2. Explain the movements possible in each major joint of the lower limb. a. Hip i. Flexion ii. Extension iii. ABduction iv. Adduction b. Knee i. Flexion ii. Extension c. Ankle i. Dorsiflexion ii. Plantarflexion © 2009 Mark Tuttle iii. Inversion iv. Eversion 3. Explain the position of each major joint of the lower limb when it is most vulnerable to injury. a. Hip i. ?????????????????// b. Knee i. Locked in full extension c. Foot i. Plantarflexed 4. Demonstrate the simple clinical tests to determine integrity of the support structures for the knee joint. a. Drawer test i. Determine if PCL or ACL are injured by pushing leg anteriorly or posteriorly. Should not move at all, if it does, there is a tear in the ligament