safety and sedation during endoscopic procedures
advertisement

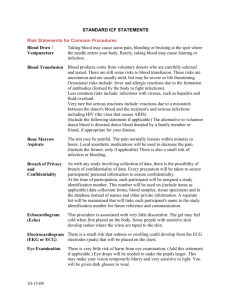
1 SAFETY AND SEDATION DURING ENDOSCOPIC PROCEDURES SUMMARY OF RECOMMENDATIONS 1. Safety and monitoring should be part of a quality assurance programme for endoscopy units. (C) 2. Resuscitation equipment and sedation reversing/antagonist drugs must be available in the endoscopy room and recovery area. (C) 3. Drugs and equipment necessary for the maintenance of airway, breathing and circulation should be present in the endoscopy room and recovery area and be checked regularly. (C) 4. A qualified nurse trained in endoscopic techniques and rescusitatory techniques should monitor the patient’s condition during procedures. (C) 5. Staff of all grades and description should be familiar with resuscitation methods and undergo periodic re-training. (C) 6. Prior to endoscopy, risk factors should be identified in both out-patients and in-patients. (C) 7. Endoscopy is sometimes an emergency procedure, so high-risk patients should be resuscitated as much as possible before attempting the procedure. (C) 8. a). Dosage of benzodiazepines and opiates should be kept to a minimum to achieve sedation and should be within the manufacturers guidelines. (C) b) Opioids should, whenever possible, be given before benzodiazepines and their effect observed before proceeding. (B) c) Most endoscopic practices recommend that 5 mg of Midazolam should usually be the maximum dose given and that elderly patients are given 1-2 mg initially with a sensible pause to observe effect. Doses in excess of Pethidine 50mg or Fentanyl 100 mcg are seldom required and elderly patients will require dose reduction (usually below 50%) when these drugs are used. (C) 9. All sedated patients must have a flexible (not “butterfly” ) intravenous cannula in situ throughout the procedure and recovery period. (C) 10. Oxygen should be given to all sedated patients and selected unsedated patients throughout the procedure and recovery period. (C) 2 11. The endoscopist is responsible for the health and safety of the patient throughout the procedure and is not just a technician. (C) 12. Pulse oximetry monitoring should be used in all sedated patients and ECG and blood pressure monitoring should be readily available for high risk patients. (C) 13. Clinical monitoring must be continued into the recovery area. (C) 14. Records of management outcome and adverse events should be taken as part of the patient plan and kept and used for audit of departmental practice. (C) Grading of Evidence (A) Meta analysis,large randomised controlled trials (B) Good evidence from trials,but less convincing e.g. smaller number in trials (C) Specialist opinion There has been considerable progress in sedation practice during endoscopic procedures since the last guidelines were published over 10 years ago. Audits by Daneshmend 1991(1), Quine 1995 (2) and Bowles 2001 (3) revealed that the culture has changed substantially from that of the late 1980’s and early 90’s. However, there is no room for complacency, and at the time of writing there is no evidence to suggest that the 30 day mortality of 1:2000 reported by Quine (1995) has improved significantly. This may be partly explained by the almost total lack of structured training in safe sedation across the profession. A recent report has again highlighted the problem (4) and suggested that each hospital nominate two Consultants, one Anaesthetist and one a user of Sedation (usually a Gastroenterologist) to collaborate in the local implementation of guidelines and the provision of a specialist service for patients with particular problems. The guidelines below have been mainly drawn from the Recommendations for Standards of Sedation and Patient Monitoring during Gastrointestinal Endoscopy, published by the Endoscopy Section Committee Working Party . The report of the Working Party on guidelines for Sedation by Non-anaesthetists, published by The Royal College of Surgeons of England, June 1993, and Implementing and ensuring safe sedation practice for healthcare procedures in adults, the report of an intercollegiate working party chaired by the Royal College of Anaesthetists 2002 (4). Where possible the original wording of the documents has been retained and the documents updated Although some endoscopic procedures such as routine diagnostic upper GI endoscopy can be carried out without sedation, many other endoscopic procedures are unpleasant and sedation as an adjunct to good pain relief and sympathetic patient management can improve both patient tolerance and acceptance and increase the technical success 3 of the procedure. The fact that the procedure can be performed without systemic medication increases the pressure to use sedation safely. Endoscopists should recognise that any drug which depresses the central nervous system has the potential to impair respiration, circulation or both. Conscious sedation has been defined as “a technique in which the use of drug or drugs produces a state of depression of the central nervous system enabling treatment to be carried out, but during which verbal contact with the patient is maintained throughout the period of sedation. The drug and techniques used to provide conscious sedation should carry a margin of safety wide enough to render loss of consciousness unlikely”. If verbal responsiveness is lost the patient requires a level of care identical to that needed for general anaesthesia. Sedatives and anxiolytics such as Benzodiazepines have no analgesic properties when conventional doses are given systemically, and attempts to use them to control pain will result in significant overdose. Pain control requires the administration of specific analgesic agents. The most popular of these agents are Fentanyl and Pethidine and should whenever possible, be given before the Benzodiazepine, and their effect observed before the administration of the Benzodiazepine. Safety will only be optimised if practitioners use defined methods of sedation for which they have received formal training. The Endoscopists Role Only trained and competent endoscopists should assume the responsibility both for sedating the patient and carrying out the examination. Trainees must be adequately instructed in IV sedation techniques and closely supervised until competent The patient’s clinical condition should be observed by a dedicated registered nurse and by the endoscopist. Drugs and equipment necessary for resuscitation are the responsibility of the consultant endoscopists and the nurse in charge of the unit and should be available immediately when required. Checking procedures should be carried out prior to each endoscopy list. Equipment available in the Endoscopy room and recovery area (if separate) should include the basic drugs and equipment necessary for the maintenance of airway, breathing and circulation as well as a source of oxygen, suction and a tipping trolley. Staff of all grades and disciplines should be familiar with resuscitation methods and undergo periodic retraining. Regular practice in simulated emergencies is recommended. 4 The Role of the Endoscopy Assistants A minimum of two endoscopy assistants, of whom at least one is a qualified nurse, must be present at each endoscopy. The assistant dedicated to patient care has a key role in monitoring the patient’s safety, comfort and well-being and in communicating significant changes to endoscopists. All endoscopy assistants must be capable of helping the endoscopists in the case of emergency such as cardiac or respiratory arrest, and adequate training and periodic retraining should be made available. It is the responsibility of the nurse in charge of the area and the endoscopists to make sure that all equipment for resuscitation is immediately available and regularly checked. Checking procedures should be carried out prior to each endoscopy list. At Risk Patients Many endoscopies are carried out on elderly patients who may have significant comorbidity and even in younger patients, the presence of heart disease, cerebrovascular disease, lung disease, liver failure, anaemia, shock and morbid obesity may indicate dangerous risk factors. Current medication needs to be determined and evaluated as to its possible effects on the sedation process. A pre-endoscopy patient record compiled by the dedicated nurse is especially helpful in identifying risk factors pertinent to the endoscopy. Sedation Techniques The majority of endoscopies are carried out using some form of sedation, usually with a benzodiazepine. There is still no tradition of formalised training in sedation in the United Kingdom. The exact doses needed to achieve safe sedation with benzodiazepine are variable, but it is both sensible and safer to use the minimum amount of drugs within the manufacturers’ guidelines to ensure patient comfort and the success of the endoscopy. Elderly patients and patients with significant comorbidity such as cardiac or renal failure will require smaller doses as the drugs take effect more slowly, and there is a longer recovery period. Other Sedative Drugs Drugs such as Propofol, Ketamine and analogous compounds require specialist knowledge, skills and equipment and should never be used without the presence of a trained anaesthetist. Certainly these drugs cannot at the present level of knowledge be considered safe for use by the operator sedationist (5) Entonox Entonox is a 50/50 mixture of nitrous oxide and oxygen with good analgesic but little hypnotic effect. It is best stored at room temperature and given by mask or mouthpiece via a demand valve. Careful instruction is important to ensure compliance but compliance, and therefore inhalation, ceases as sedation approaches making it a safe analgesic in the majority of patients. It is not safe for use in patients 5 who have compromised respiratory function or pneumothorax. It is perhaps best used for moderately painful procedures such as colonoscopy or flexible sigmoidoscopy and recovery is rapid with a “washout time” of five to ten minutes. Difficult Patients Patients occasionally become restless or even violent following sedation. This situation can sometimes be salvaged by reversing the sedation which may allow the endoscopy to proceed but when such difficulty can be anticipated general anaesthesia is usually the best option. Alcoholics and regular benzodiazepine users are notoriously difficult to sedate and their response may be unpredictable or even paradoxical on occasions. In these circumstances the prior administration of an opioid can be useful. Children These guidelines are intended for adult endoscopy only. The Endoscopy Working Party of the Paediatric Section of the B.S.G. are currently reviewing the guidelines for safe sedation in children and these will be published in due course Special Circumstances In Colonoscopy and ERCP Benzodiazepine sedation is usually supplemented with opioids such as pethidine and Fentanyl. The dose requirement is sometimes predictable, but synergism between these drugs may lead to an increase in cardiorespiratory events. If the use of an opioid is anticipated (for example, by a previous difficult procedure) then it should be given first and the benzodiazepine dose titrated carefully with an up to four-fold decrease in total. (7) Specific antagonists for benzodiazepines and opioids should be available at all times in the endoscopy unit and recovery area but their presence should not encourage over dosage of the sedative drugs. Administration of an antagonist does not alter the requirement to monitor vital functions where depression of these has occurred. Flumazenil may take several minutes to completely reverse benzodiazepine respiratory depression. The duration of action of both opiods and benzodiazepines is longer than that of their antagonist and reversal may be short-lived, needing repeat administration. It is essential that all patients undergoing intravenous sedation have a cannula placed in the vein for reliable, continuous venous access during the procedure. A flexible plastic cannula with an introduction needle that is removed after insertion must be employed. This cannula must be left in place until recovery is complete. Clinical Monitoring, pre-oxgenation and supplemental oxygen Oxygen desaturation can occur during endoscopic procedures where sedation is used, especially when the patient has been over sedated remembering that a reading below 90% is dangerous and requires immediate intervention. The Endoscopists is responsible for the well being and clinical observation of the patient undergoing endoscopy in conjunction with another individual. This individual should be a 6 qualified nurse trained in endoscopic techniques or another medically qualified practitioner. Preoxygenation with oxygen enriched air (2 litres per minute ) is safe even in chronic obstructive pulmonary disease and greatly diminishes or prevents hypoxaemia. This should be used routinely in all at-risk patients. Pulse oximetry should always be used during endoscopy, as clinical observation is a poor method of determining respiratory depression and hypoxia. Alarm systems may alert the endoscopist in the event of deterioration in the patient’s clinical condition but there is no evidence that the routine use of monitoring equipment will reduce the morbidity and mortality associated with Endoscopy. However the following recommendations should ensure high quality patient care and reduce the risk of cardio-pulmonary events: The use of monitoring devices and alarms should not distract the endoscopists and assistant from basic clinical observations Pulse oximetry should be combined with continuous ECG monitoring in those patients who are at high cardiac risk. In the event of desaturation, encouraging the patient to breathe deeply with supplemental oxygen, termination of the procedure, assisted ventilation and pharmacological reversal of either the benzodiazepine and/or the opioid may remedy this. Patient Recovery Clinical monitoring must be continued into the recovery period and supplemental oxygen and pulse oximetry may be needed and it is worth remembering that respiratory complications such as aspiration pneumonia may present many hours or even days after the endoscopy. The endoscopists is still responsible for the post endoscopy recovery period and should give clear instructions to the recovery nursing staff or ward, especially when an adverse event has occurred. Day cases should be accompanied home by a responsible adult who should then stay with them for at least 12 hours if they live alone. Clear written instructions should be given to this person as to what to do and whom to contact in event of problems arising. It is recommended that patients who have been sedated with an intravenous benzodiazepine do not drive a car, operate machinery, sign legal documents or drink alcohol for 24 hours. This irrespective of whether their sedation has been reversed with flumazenil. Records and Audit The endoscopic records should include a patient-specific record of the procedure (paper or electronic, or preferably both). This will include the pre-endoscopic state of the patient, the drugs used during the procedure and any adverse events encountered. 7 Audit should be an integral part of the records of every endoscopy department. Appropriate use of this technique is essential in evaluating the frequency of adverse events related to both the procedure and to the sedation employed. References 1. Daneshmend TK, Bell G D, Logan R F A , Sedation for Upper Gastrointestinal Endoscopy: results of a national survey, GUT 1991; 32: 12-15 2. Quine M A, Bell G D, McCloy R F, Charlton J E, Devlin H B, Hopkins A A. Prospective audit of upper Gastrointestinal Endoscopy in two regions of England: Safety, staffing and sedation methods. Gut 1995;36:462-467. 3. Bowles C J A, Leicester R, Swarbrick E, Williams C B, Romaya C, Epstein O, GUT 2001; 48 (Supplement 1): A21 4. Implementing and ensuring Safe Sedation Practice for Healthcare Procedures in adults. Report of a Working Party established by the Royal College of Anaesthetists, www.aomrc.org.uk November 2001 5. Bell G D, Charlton J E, Editorial – Colonoscopy – is Sedation necessary and if so does IV Propafol have a role? Endoscopy 2000;32:264-267 6. Ben Shlomo I, Adb-el-Khalim H, Ezry J, Zohar S, Tverskoy M, Midazolam acts synergistically with Fentanyl for induction of anaesthesia, British Journal of Anaesthesia 1990:64:45-7 Acknowledgements Mrs Diane Campbell and Professor Duncan Bell kindly gave of their time to review this manuscript. 8 This paragraph should be on the inside front cover. This report was originally published in 1991 and has been updated by Dr Robin Teague on behalf of the Endoscopy Section Committee of the British Society of Gastroenterology.