Surgical Anesthesia (CA 1)
advertisement

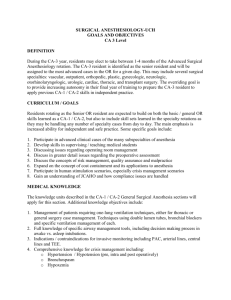
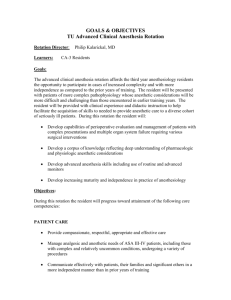
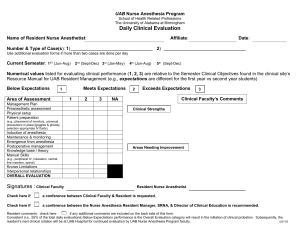
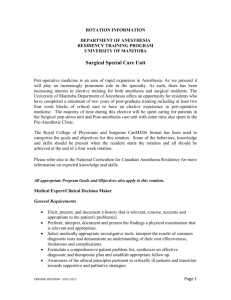
SURGICAL ANESTHESIOLOGY- UCH GOALS AND OBJECTIVES CA 1 Level DEFINITION This is a four month rotation for CA-1 residents, which includes anesthesia for several surgical specialties to include general, orthopedic, plastic, gynecologic, neurologic, otorhinolaryngologic, and urologic surgery. There is one month dedicated as the general OR advanced airway rotation. CURRICULUM/GOALS Residents rotating through the general operating room in their CA-1 year are expected to be introduced to the basic fundamentals of anesthetic care of the patient undergoing surgery. This includes clinical expertise and cognitive management of the perioperative needs of the surgical patient undergoing routine procedures found in community and tertiary care hospitals. Introduction to and competence in performing the basic functions of the anesthesiologist including preoperative assessment, medical optimization, anesthetic selection, maintenance of homeostasis, and postanesthetic care are expected for this rotation. Participation in human stimulation scenarios, especially crisis management scenarios will be utilized. MEDICAL KNOWLEDGE At the conclusion of this rotation, the resident should be able to: 1. Assess the functional status of the patient’s health including a comprehensive review of major organ systems. 2. Describe the physiologic effects and impact on anesthesia of medications used for acute and chronic illness 3. List the American Society of Anesthesiologists (ASA) Physical Class categories and the key features of each 4. Describe the Mallampatti classification of airway assessment and the implications of each thereof 5. Discuss the major forms of anesthesia (general, regional, local) and know the common complications associated with each and the relative risk 6. Describe the basic function and design of the anesthesia machine and other anesthesia delivery systems including knowledge of inherent safeguards and the sequence of the functional check-out procedure 7. Understand the composition and physiologic consequences of various intravenous fluids used during surgery 8. Discuss the expected fluid needs of the patient as it relates to preoperative preparation/fasting and intraoperative changes. 9. List the ASA guidelines for preoperative fasting as pertains to solids, liquids, and abnormal gastric function 10. List those factors which predispose patients to postoperative nausea and vomiting, and the possible solutions to this problem 11. Understand the pharmacodynamics and pharmacokinetics of the intravenous and volatile agents used in surgery 12. Understand the pharmacodynamics and pharmacokinetics of sedative and anxiolytic medications used in the preoperative period. 13. Discuss the pharmacodynamics and pharmacokinetics of opioid analgesics used in the perioperative period 14. Have a basic understanding of the proper positioning of patients to prevent injury during surgery 15. List the physiologic changes associated with anesthesia, surgery, and positioning. 16. List the indications for blood transfusions and the risks of blood products 17. Know the minimum alveolar concentration (MAC) of common volatile anesthetics 18. Understand the pharmacodynamics, pharmacokinetics, and physiology of neuromuscular blocking agents and neuromuscular function 19. Discuss pulmonary physiology in respect to the maintenance of proper ventilation of the patient and the appropriate timing of extubation 20. Discuss the various stages of anesthesia and anesthetic depth and the assessment thereof PATIENT CARE At the conclusion of this rotation, the resident should be able to: 1. Perform a comprehensive preanesthetic history and physical examination, and assess the adequacy of preparation to include appropriate laboratory testing 2. Determine if the patient’s chronic medical conditions are stable and optimally managed 3. Assign an ASA Physical Classification number to the patient 4. Determine if the patient has met the criteria for preoperative fasting or will need a rapid sequence induction 5. Prepare an operating room for a case to include proper selection of induction medications, set up of intravenous fluids, and function check the anesthesia machine 6. Perform induction of anesthesia with minimal assistance for ASA Class I and II patients 7. Intubate the trachea using direct laryngoscopy after proper mask ventilation 8. Identify the patient with a potentially difficult airway 9. Properly select induction medications and maintenance agents based on the patient’s comorbid conditions, type of surgical case, and anticipated length of surgery 10. Select and administer the proper type and amount of intravenous fluids based on the patient’s needs due to comorbid conditions, preoperative volume status, and type and length of surgical procedure 11. Properly manage neuromuscular blockade for a variety of patients and surgical procedures 12. Manage an anesthetic to permit and rapid and smooth emergence from anesthesia, and correctly assess when a patient is ready for tracheal extubation 13. Properly perform intravenous and arterial cannulation including central venous access (with assistance) 14. Assess the need for blood product administration and safely deliver the infusion, and recognize complications associated with specific products 15. Properly (safely) position a patient for surgery in the supine, lateral decubitus, and prone positions, and recognize potential injurious situations. 16. Make a rational choice of medications to use intraoperatively and postoperatively to provide for adequate analgesia 17. Provide appropriate anesthesia for the wide variety of routine operations seen in the community and tertiary care settings 2 INTERPERSONAL AND COMMUNICATION SKILLS At the conclusion of the rotation the CA-1 resident will: 1. Be able to form a rational plan, in consultation with the attending anesthesiologist, for anesthesia for a routine surgical procedure, communicate that plan to the patient, and obtain informed consent 2. Inform the attending anesthesiologist of any changes in patient condition, or progress of the procedure which may affect patient condition, that occur during anesthesia care 3. Cooperate with the preoperative holding area nursing staff and surgeons to assure proper preparation of the patient for the planned surgical procedure and coordination of preoperative testing 4. Be able to interact effectively with the patient, family members, and nursing staff to insure patient satisfaction with their care PROFESSIONALISM At the conclusion of the rotation the CA-1 resident must: 1. Demonstrate adherence to procedures designed to protect patient privacy 2. Demonstrate effective sensitivity to cultural, racial, and religious issues of importance to their patient and the patient’s family 3. Be able to achieve a smooth and safe intraoperative anesthetic course for the surgical patient 4. Anticipate common intraoperative problems associated with routine surgical cases 5. Confirm the safety of their patient in the postanesthesia setting as well as adequate analgesia and satisfaction with their care 6. Be prepared, in a timely fashion, to manage their cases PRACTICE BASED LEARNING AND IMPROVEMENT At the conclusion of the rotation the CA-1 resident will gain an understanding of the following: 1. 2. 3. 4. 5. 6. 7. 8. 9. The role of evidence based medicine techniques and how they apply to anesthesiology Statistical analysis Randomized, controlled trial studies Limitations of RCTs in regards to anesthesia practice Cochrane database and other meta-analyses The necessity of electronic based media and its utilization The role of continuing medical education The role of maintenance of certification processes The role of life long learning and self-assessment and its implications regarding selfimprovement SYSTEMS BASED PRACTICE 3 The CA-1 resident will gain an understanding of the following regarding systems based practice: 1. The Institute of Medicine’s core competencies in regard to the delivery of health care, namely that care is to be: o safe o timely o effective o efficient o equitable o patient-centered 2. Anesthesia billing and collection modules 3. Staffing and the implications of running an operating room 4. The role of physician extenders in anesthesiology such as ○ CRNA ○ anesthesia assistants ○ anesthesia technicians 5. Medicare teaching rules and regulations, especially in regards to supervision and billing 6. Malpractice and risk assessment 7. Quality improvement and the role of the Center for Clinical Effectiveness (CCE) at this institution 8. Anesthetic costs, pharmaceutical and equipment Evaluation Tools: 1. 2. 3. 4. 5. 6. AKT-1, AKT-2, AKT-6 to evaluate medical knowledge of the CA-1 resident in training Self – evaluation process Direct observation by faculty with monthly written performance evaluations. 360° Evaluations by nursing / OR staff. “Mock” Oral Exams given by faculty Mentoring system: Each resident will select a mentor during their first CA-1 year to help direct training based on the results of the above evaluations. Rev. 7/ 2009 4