Potential Nursing Diagnoses
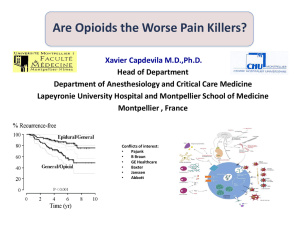
advertisement

NURSING PROCESS FOCUS: Patients Receiving Lidocaine (Xylocaine) Assessment Potential Nursing Diagnoses Prior to administration: Aspiration, risk for, related to effects of anesthesia Obtain complete health history including allergies, drug history and possible drug Comfort, impaired, related to source of interactions. condition requiring surgery Assess for presence/history of the following Injury, risk for, related to loss of disorders: Stokes-Adams syndrome, severe sensation during anesthesia cardiac problems, and/or decreased liver Knowledge, deficient, related to lack of function. This medication is contraindicated previous experience with local for those with this disorder. Assess for anesthesia allergies to amide-type local anesthetics Check for the presence of broken skin, infection, burns and wounds where medication is to be used. Assess for character, duration, location, and intensity of pain where medication is to be used Planning: Patient Goals and Expected Outcomes Patient will: Demonstrate absence of pain during surgical procedure Demonstrate absence of side effects/adverse reactions Demonstrate knowledge of drug action and potential side effects Avoid physical injury while anesthetic is in effect Implementation Interventions and (Rationales) Patient Education/Discharge Planning Instruct patient to: Observe for proper use (to avoid injury, or improper absorption of drug). Swish and spit out if using for relief of mouth discomfort or pharyngeal discomfort Avoid applying to broken or abraded skin Avoid contact of medication with eyes Instruct patient to: Monitor for cardiovascular problems. (Could indicate toxicity) Report any unusual heart palpitations. See their health care provider regularly if using medication on a regular basis.. Observe skin or mucous membranes for Instruct patient to report irritation or infection or inflammation. (Condition could increase in discomfort in areas be worsened.) medication used. Monitor length of effectiveness (Lidocaine Instruct patient to report any discomfort is effective for 1-3 hours. Injury could during procedure. occur during period of anesthesia.) Provide patient safety. ( Injury may occur to Instruct patient that he/she will have no affected area due to lack of sensation) feeling in anesthetized area, so must take extra caution to avoid injury, including heat-related injury. Observe for return of gag reflex. (Xylocaine Instruct patient: viscous may interfere with swallowing Not to eat within 1 hour of reflex.) administration Not to chew gum while any portion of mouth or throat is anesthetized to prevent biting injuries Use cautiously in patients with CHF, renal Instruct the patient to notify the health disease, or respiratory depression. care provider at the first sign of any changes in health condition. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). NURSING PROCESS FOCUS: Patients Receiving Nitrous Oxide Assessment Potential Nursing Diagnoses Prior to administration: Anxiety, related to upcoming surgery, loss of control secondary to anesthesia Obtain complete health history, including allergies, drug history and Gas exchange, impaired, risk for, related to possible drug interactions. respiratory depression Assess for presence/history of severe Knowledge, deficient, related to no prior respiratory, cardiac, renal or liver surgical or anesthesia experience disorders Nausea, related to after-effects of Obtain baseline vital signs, especially anesthesia blood pressure, pulse and respirations Sensory perception, disturbed, related to Obtain blood work: complete blood CNS depression secondary to anesthesia count and chemistry panel Assess for hypersensitivity Assess patient’s knowledge of procedure and level of anxiety Planning: Patient Goals and Expected Outcomes Patient will: Demonstrate adequate anesthesia during surgical procedure Have no side effects or adverse reaction to anesthesia Demonstrate understanding of perioperative procedures Maintain adequate ventilation during surgical procedrue Implementation Interventions and (Rationales) Patient Education/Discharge Planning Monitor for cardiovascular disease, Teach patients about possible side effects. especially along with increased intracranial pressure. (Hypnotic effects of nitrous oxide may be prolonged or potentiated) Obtain history of myasthenia gravis. Advise patient of the importance of (Patient may need extra support during complete disclosure of medical history, to surgery and longer monitoring after, to ensure maximum safety. ensure adequate respiratory function nitrous oxide may cause respiratory depression. Hypnotic effects of nitrous oxide may be prolonged or potentiated.) Monitor for respiratory difficulty. Instruct patient to report any breathing (Monitor more closely for adequate O2difficulty. CO2 exchange, and for elimination of nitrous oxide.) Monitor emotional state. (Patients who Teach patient stress reduction techniques are fearful, extremely anxious may have such as deep breathing, imagery, and a more difficult time becoming distraction. anesthetized and staying anesthetized.) Monitor post-operative recovery, i.e. Advise patients about routine and possible LOC, nausea and vomiting, and pain. side effects. Evaluate knowledge level prior to Advise patient what is necessary for him to surgery. (Determine what patient already have a satisfactory surgical experience. knows about pre and post-op procedures and how much is accurate information) Evaluation of Patient Outcomes Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”) NURSING PROCESS FOCUS: Patients Receiving Thiopental (Pentothal) Assessment Potential Nursing Diagnoses Prior to administration: Anxiety related to impending surgery Obtain complete health history including Aspiration, risk for, related to increased allergies, drug history and possible drug secretions, respiratory depression interactions. Breathing pattern, ineffective, risk for, Assess for presence/history of related to side effects of anesthesia respiratory and cardiac disorders, Knowledge, deficient, related to lack of seizure disorders, increased intracranial prior experience with surgery or general pressure, myxedema, pregnancy, and anesthesia underlying neurological disorders. Use with Sensory perception, disturbed, related to caution CNS depression secondary to anesthesia Obtain baseline vital signs, esp. blood pressure, pulse and respirations Obtain blood work: complete blood count, liver studies Assess for hypersensitivity Assess patient’s knowledge of procedure and level of anxiety. Planning: Patient Goals and Expected Outcomes Patient will: Experience no pain during surgery Demonstrate no side effects during post-operative period Maintain adequate ventilation during surgery Avoid injury during surgical procedure Implementation Interventions and (Rationales) Observe for anxiety. (Anxiety prior to surgery is not uncommon. Patient may need sedative, anti-anxiety medication prior to immediate pre-op period.) Monitor for side effects. (Shivering and trembling are most common. Patient may also experience nausea/vomiting, headache, and somnolence.) Monitor LOC and for adverse reactions called emergence delirium postoperatively. (Symptoms include hallucinations, confusion, excitability.). Report immediately. Monitor vital signs initially every 3-5 Patient Education/Discharge Planning Educate patient concerning pre and post-op care. Inform patients to report to the health care provider any side effects. Inform patients of possible side effects. Advise patient to report to the health care minutes, then every 4 hours. (May lead to provider any side effects. dysrthythmias, tachycardia, bradycardia, myocardial depression, and respiratory depression so severe patient may need ventilatory assistance.) Observe for allergic response. Teach patient any signs and symptoms of (Symptoms include hypotension, side effects and to report to the health care bronchospasm, hives, facial edema). provider any side effects. Report immediately. Monitor for thrombophlebitis. (As an Inform patients to report immediately to intravenous anesthetic, extravasation may health care provider of symptoms of cause thrombophlebitis.) thrombophlebitis Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). NURSING PROCESS FOCUS: Patients Receiving Halothane (fluothane) Assessment Prior to administration: Obtain complete health history including allergies, drug history and possible drug interactions. Assess for presence/history of pregnancy, diminished hepatic functioning, cardiac disorders hypotension Assess for the use of the same anesthesia use within 21 days Assess other medications patient is taking. May influence effectiveness of gas or increase respiratory depression Obtain baseline vital signs, especially. blood pressure, pulse andrespirations Obtain blood work: complete blood count, liver studies Assess for hypersensitivity Potential Nursing Diagnoses Breathing pattern, ineffective, risk for, R/T side effects of halothane Cardiac output, decreased, risk for, R/T side effects of halothane Gas exchange, impaired, risk for, R/T respiratory depression secondary to halothane Knowledge, deficient, R/T no prior experience with surgery or general anesthesia Nausea, post-operative, risk for, R/T aftereffects of halothane Sensory perception, disturbed, related to CNS depression secondary to anesthesia Planning: Patient Goals and Expected Outcomes Patient will: Experience no pain during surgery Report no side effects of halothane during peri- or post-operative period Demonstrate understanding of the perioperative phase of their surgical experience Maintain adequate ventilation during the surgical procedure Implementation Interventions and (Rationales) Patient Education/Discharge Planning Obtain history of previous use of halothane. (If used within 14-21 days, halothane cannot be used. Too frequent use of halothane may lead to halothane hepatitis, potentially fatal adverse reaction which is more common in elderly or obese patients; not seen in children.) Monitor vital signs during procedure and post-operatively, esp. for hypotension, bradycardia, and dysrhythmias. (Halothane can decrease blood pressure. Sensitizes myocardium Instruct patient: To recognize warning signs of halothane hepatitis including unexplained rash, fever. Symptoms of halothane hepatitis usually occur within two weeks of use To obtain follow-up lab studies Advise patient regarding possible side effects. to effects of catecholamines or sympathomimetics, which could lead to serious dysrhythmias.) Monitor for decreased hepatic functioning. (Halothane is metabolized in the liver. Halothane has an increased risk of causing hepatic toxicity.) Monitor for nausea/vomiting post-op. (Common side effects with use of halothane.) Monitor LOC post-op. Advise patient to keep all appointments for lab work. Advise patient to immediately report side effects. Instruct patient not to drive or do activities requiring mental alertness for at least 24 hours after surgery. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”).