Surgical Site Marking Policy

Surgical Site Marking Policy
Version 01
Name of responsible (ratifying) committee CHAT Governance Committee
Date ratified 30 October 2014
Document Manager (job title)
Date issued
Review date
Electronic location
Related Procedural Documents
Key Words (to aid with searching)
Consultant Anaesthetist, Theatre Governance Group
22 January 2015
01 October 2017
Clinical Policies
See Section 9 of this policy
Surgical Site Marking, Surgical Mark, Procedure Site
Marking
Version Tracking
Version Date Ratified
1 30.10.2014
Brief Summary of Changes
New policy
Author
Dr S Kerr
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 1 of 11
CONTENTS
QUICK REFERENCE GUIDE
1. INTRODUCTION
2. PURPOSE
3. SCOPE
4. DEFINITIONS
5. DUTIES AND RESPONSIBILITIES
6. PROCESS
7. TRAINING REQUIREMENTS
8. REFERENCES AND ASSOCIATED DOCUMENTATION
3
4
4
4
5
5
6
7
8
9. MONITORING COMPLIANCE WITH, AND THE EFFECTIVENESS 10
OF PROCEDURAL DOCUMENTS
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 2 of 11
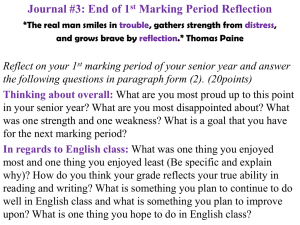
QUICK REFERENCE GUIDE
For quick reference the guide below is a summary of actions required. This does not negate the need for those involved in the process to be aware of and follow the detail of this policy.
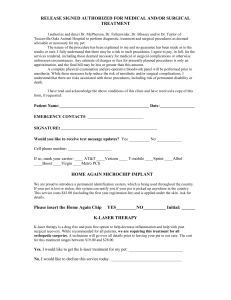
Marking the operative site
Is a vital part of the preoperative verification process to prevent wrong site surgery with the core steps:
The consent process in accordance with Royal college Surgeons Good Surgical
Practice 2009 Guideline (Section 4.1)
Surgical site marking (covered in this policy)
Preoperative verification checklist (Theatre Checklist in the PHT surgical integrated record)
WHO surgical safety checklist (specifically the Time Out)
1. Who makes the mark? The person responsibility for making the mark is the surgeon performing the procedure who is familiar with the patient, or a deputy also present as part of the team for the procedure. Therefore the surgeon who makes the mark should also be present at the specific procedure.
2. Specialties can designate other members of staff to mark in collaboration with the surgeon under their governance structure e.g. stoma nurses
3. When, prior to the patient transfer to the operating department or equivalent area. In order to ensure that the surgical mark supports the check in process/WHO checklist and can be corroborated against the consent and the patient ID band.
4. How, the mark should be made using a marker that is sufficiently permanent to remain visible after completion of the skin preparation.
5. Make the mark at or near the incision site preferably with in 6 inches of the incision. Do NOT mark any non-operative site(s) unless necessary for some other aspect of care.
6. The mark should be an arrow where possible.
7. The mark should be positioned to be visible after the patient is prepped and draped.
8. The site for all procedures that involve incisions, percutaneous punctures or insertion of instruments must be marked.
9. At a minimum, mark all cases involving laterality, multiple structures (fingers, toes, lesions), or multiple levels.
10. Final verification of the site mark should take place during the "sign in" of the WHO checklist .
11. A defined process should be in place for patients who refuse site marking.
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 3 of 11
1. INTRODUCTION
The best available evidence (international) puts the incidence of wrong-site surgery at 1-2 per
100,000 procedures (disturbingly high number for a never event)
“The training, competence and good intention of the surgeon, doctor,
Dentist or health care professional alone are not sufficient to prevent
wrong si te procedures.”
Prevention therefore requires an active process by the entire surgical team, not just by the operating surgeon, utilizing a standardized peri-operative process designed to prevent such never events. Portsmouth Hospitals NHS Trust the core steps are:
The consent process in accordance with Royal college Surgeons Good Surgical
Practice 2009 Guideline Section 4.1
Surgical site marking (covered in this policy)
Preoperative verification checklist (Theatre Checklist in the PHT surgical integrated record)
WHO surgical safety checklist (specifically the Time Out)
This policy has been formulated in response to the recommendations made by the National
Patient Safety Agency (NPSA) and is designed to complement the World Health Organisation
(WHO) checklist implemented on 1 June 2009.
.
2. PURPOSE
The purpose of this policy is to clarify and inform a universally acceptable method within
Portsmouth Hospitals NHS Trust (the Trust), by which patients undergoing a surgical procedure will have their operative site marked appropriately and accurately. In addition how the surgical site marking is part of the series of checks and to prevent wrong site surgery in accordance with the WHO checklist prior to incision.
It will:
Support the verification process for checking the surgical site
Guide when the marking should be undertaken.
Define Who should mark the surgical site
Minimize the risk of surgery on the wrong site or wrong patient
Minimize the risk of the wrong procedure being performed
Inform and guide the operating surgeon as to the method used to mark the skin and operative site
Where anatomically the site will be marked
3. SCOPE
To whom the document applies.
This policy applies to all permanent, locum, agency and bank surgeons or their deputies who work in Portsmouth Hospitals NHS Trust, the MDHU (Portsmouth) and who are responsible for the identification and marking of a patient’s surgical site.
‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 4 of 11
4. DEFINITIONS
Integrated Surgical Pathway
Integrated care pathway/paperwork is the structured multidisciplinary care plan which details essential steps and documentation for the care and preparation of patients for surgical/medical procedures in theatre areas.
World Health Organisation (WHO) Checklist: a checklist developed by the WHO and collaborators at the Harvard School of Public Health, the checklist identifies key safety steps during perioperative care that should be accomplished during every single operation no matter the setting or type of surgery. It has been shown to significantly reduce complications and deaths from surgery.
Time Out Section of WHO Checklist: a momentary pause taken by the team just before skin incision in order to confirm that several essential safety checks are undertaken and involves everyone in the team.
5. DUTIES AND RESPONSIBILITIES
Director of Clinical Standards (Medical Director)
The Director of Clinical Standards has ultimate responsibility for ensuring that appropriate processes are in place for the safe management of surgical patients, including preoperative marking.
Clinical Directors
Clinical Directors in each specialty have responsibility for ensuring their surgeons mark patients’ accordingly and carry out the instructions within this policy.
Operating Surgeon (or deputy)
It is the responsibility of the operating surgeon or deputy to mark the operative site in accordance with this policy
Anaesthetist
The anaesthetist is formally responsible for the “Sign In” section of the WHO checklist it is one of there duties to ensure the marking and consent are correct
Anaesthetist’s are responsible for checking the site of any proposed local/regional block using the surgical mark and the “Stop before you block” process.
Who (who is responsible ?)
The operating surgeon is responsible for ensuring that each individual patient has been marked appropriately prior to arrival in theatre.
The Operating Theatre Team
The operating theatre team carries out the WHO Checklist has joint responsibility for ensuring that the correct site has been identified prior to commencement of surgery.
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 5 of 11
6. PROCESS
Marking the operative site
Vital part of the preoperative verification process to prevent wrong site surgery with the core steps prior to starting a procedure:
1) The consent process in accordance with Royal college Surgeons Good Surgical Practice
2009 (Guideline Section 4.1)
2) Surgical site marking (covered in this policy)
3) Preoperative verification checklist (Theatre Checklist in the PHT surgical integrated record)
4) WHO surgical safety checklist (specifically the Sign In / Time Out) before the start of a surgical intervention e.g. skin incision.
6.1 Who makes the mark?
The principle should be that the surgeon/operator who makes the mark is then present during the procedure.
6.1.1
The person who is ultimately responsibility for making the mark is the surgeon performing the procedure , who should be familiar with the patient.
6.1.2
Marking may be delegated to a deputy who will be present as part of the team for the procedure. However the responsibility remains with the lead surgeon. If marking is delegated to another doctor, they must be permitted through a training program to participate in/perform the procedure.
6.1.3 Specialties can designate other members of staff to mark in collaboration with the surgeon. This must be defined under their governance structure and include appropriate training and processes to support good practice e.g. stoma nurses
6.2 When to make the mark
The mark should be made prior to the patient transfer to the operating theatre. This ensures that the supporting steps in the check in process confirming correct procedure and site, specifically the
WHO checklist, can then occur in the theatre (or equivalent) areas.
6.3 How to make the mark
6.3.1
The surgeon should verify the operation to be undertaken, matched against the patient ID band leading to making of the mark.
This should be a process of checking the records, including diagnostic imaging results (e.g. X-rays, scans and other electronic imaging) and other diagnostic test results (e.g. biopsies) with the consent form. The patient should be involved, (prior to any sedative pre-medication) including confirmation against their ID band, to verify the site/sites to be marked.
6.3.2 The mark should be made using a marker that is sufficiently permanent to remain visible after completion of the skin preparation.
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 6 of 11
6.3.3
Make the mark at or near the incision site preferably with in 6 inches of the incision . Do NOT mark any non-operative site(s) unless necessary for some other aspect of care.
6.3.4
The mark should be an arrow and where possible include an indication of the procedure. (e.g. use a description of procedure)
6.3.5
The mark should be positioned to be visible after the patient is prepped and draped.
6.3.6
The site for all procedures that involve incisions, percutaneous punctures, or insertion of instruments must be marked.
Including:
The surface, level, specific digit or lesion to be operated on.
Laterality. For procedures involving laterality of organs that have an incision or approach from the midline or natural orifice the site should be marked and laterality marked.
Stomas
6.3.7
At a minimum; mark all cases involving laterality, multiple structures (fingers, toes, lesions), or multiple levels.
Final verification of the site mark should take place during the "time out" of the WHO checklist.
6.4 Exceptions to Site Marking
6.4.1 Exemptions:
Single organ cases (e.g., Cesarean section, cardiac surgery, gastrectomy, cystectomy).
Interventional cases for which the catheter/instrument insertion site is not predetermined (e.g.,
cardiac catheterization).
Teeth BUT, indicate operative tooth name(s) on documentation OR mark the operative tooth
(teeth) on the dental radiographs or dental diagram.
Premature infants, for whom the mark may cause a permanent tattoo.
Cases where the side or site of surgery needs to be confirmed by examination or exploration under anaesthetic (EUA).
Cases where anatomically difficult or technically difficult to mark (e.g. perineum, acute burns)
6.4.2 For any sites not marked, the proposed operation/procedure must be reviewed to verify patient and procedure at the ‘Time Out’ part of the WHO Safety Checklist. This must be undertaken in conjunction with a review of all relevant documentation, including: the patient’s notes; appropriate charts; diagnostic imaging (correctly oriented); and a ‘double person’ check of all information. The procedure must not commence without this review having occurred.
6.4.3 Patients refusing to have a mark must have this clearly documented in their notes and the process for any sites not marked section 6.4.2 followed.
6.5 Specialty Specific instructions (not otherwise covered above)
6.5.1 Urology
When access to high resolution radiology (PACS) to confirm the side/site of surgery is unavailable in the admission areas then the PACS equipment in theatre may be used.
Provided.
1) All alternative options for the standard marking process have been excluded
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 7 of 11
2) Provided that the surgical site is confirmed and marked to the standards described in the Royal College Surgeons Good Surgical Practice 2009 (Guideline
Section 4.1).
3) The mark is made prior to the WHO check in processes.
6.5.2 Ophthalmic Surgery
For single eye surgery a small mark should be made either on the
forehead above the correct eye, or on the lateral aspect of the eye
between the lateral canthus and the ear, pointing to the correct
eye for treatment.
The exception is for planned bilateral procedures on both eyes (such as bilateral squint surgery), but the laterality of such procedures should be well documented.
The marking of a child’s head/face must be assessed at the time of preassessment by the surgeon as to its psychological appropriateness. If no mark is made, then the procedures referred to at 6.4.2 must be adhered to.
6.5.3 Bilateral Treatment
Whilst this policy focuses on laterality, specific anatomical sites, levels and areas, surgeons must consider that it is possible to perform the wrong bilateral procedure(s). Therefore site marking for bilateral, identical, procedures is not required. If no mark is made, then the procedures referred to at 6.4.2 must be adhered to.
6.5.4 ENT Surgery
There may be occasions where marking the patient’s skin to ‘point’ to the correct site for surgery may be inappropriate e.g. bilateral tonsillectomy/adenoidectomy, laryngectomy. In these cases section 6.4.2 for any site not marked apply. For ENT surgical sites where a skin incision is made on a specific side i.e. surgery on the external pinna and tympanotomy these should be marked with an arrow accordingly.
6.5.5 Burr Holes
Incidents have been reported to the NPSA of wrong side burr-holes being carried out as a result of and failure to mark the appropriate side for surgery before the patient arrives in theatre. It is now acceptable practice to mark the side of the burrhole to be carried out in the usual manor as directed by the Royal College of
Surgeons, Neuro-anaesthesia Society and the Society of British Neurological
Surgeons.
6.5.6 Digital Surgery
Each and every digit to be operated on must have an individual arrow pointing to and as close as possible to the respective digit.
6.5.7 Anaesthetic Role and Local/Block Procedures
The Anaesthetist is formally responsible for the “Sign In” section of the WHO checklist and it is one of there duties to ensure the marking and consent are correct
The site of the local/block procedure should use the surgical mark and a formal verification using the “Stop before you block” process prior to block insertion.
6.6 STERILITY OF MARKING
Research has been carried out to ascertain whether the use of a permanent ink marker to mark a surgical site, affec ts the sterility of a patient’s skin after it has been cleaned with surgical preparation solution.
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 8 of 11
The results showed that no growth was seen in the cultures of swabs taken on both the control group (un-marked) and on the experimental group (marked). Pre-operative marking of surgical sites in accordance with the Joint Commission protocol did not affect the sterility of the surgical field, therefore providing support for the safety of surgical site marking (Cronen, et al . 2005).
7. TRAINING REQUIREMENTS
Training of all surgeons and junior doctors must be carried out at their induction covering the
WHO Checklist and the guidelines for surgical site marking. The training will be supervised/responsibility of the clinical teams providing induction for new members of their surgical teams. This will be directed by the specialty Clinical Director.
8. REFERENCES AND ASSOCIATED DOCUMENTATION
Internal
WHO checklist policy, as adapted for use in Portsmouth Hospitals NHS Trust
External
World Health Organisation (WHO) – Implementation manual, Surgical Safety Checklist
1 st Ed (2009)
National patient safety Agency (NPSA) – Patient safety Alert 06 – Correct site surgery, making your surgery safer (2005)
Good Surgical Practice (2008) The Royal College of Surgeons of England
Guide To Surgical Site Marking High 5s CEPPRAL http://www.has-sante.fr/portail/upload/docs/application/pdf/2013-
05/guide_to_surgical_site_marking.pdf
AfPP Correct Site Surgery http://www.afpp.org.uk
How to guide to the five steps to safer surgery (NPSA) http://www.nrls.npsa.nhs.uk/resources/?EntryId45=92901
9. EQUALITY IMPACT STATEMENT
Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds.
This policy has been assessed accordingly
Our values are the core of what Portsmouth Hospitals NHS Trust is and what we cherish. They are beliefs that manifest in the behaviors our employees display in the workplace.
Our Values were developed after listening to our staff. They bring the Trust closer to its vision to be the best hospital, providing the best care by the best people and ensure that our patients are at the centre of all we do.
We are committed to promoting a culture founded on these values which form the ‘heart’ of our
Trust:
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 9 of 11
Respect and dignity
Quality of care
Working together
No waste
This policy should be read and implemented with the Trust Values in mind at all times.
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 10 of 11
10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS
The compliance with this polic y will be responsibility of the Clinical CSC’s, and the Specialty Clinical Directors. Monitoring of compliance will be the responsibility of the CSC and specialty governance groups and will involve:
Minimum requirement to be monitored
Lead Tool Frequency of
Report of
Compliance
Reporting arrangements Lead(s) for acting on
Recommendations
Audit via the WHO
Safety Checklist Audit of all patients who have procedures in Theatres.
Evidence of completed training by staff involved in surgical site marking.
See above
See above
Policy audit report to:
Trust
Committee
Governance
Policy audit report to:
Trust
Committee
Governance
See above
See above
Evidence of collection of adverse incident reports and discussion at mortality and morbidity meetings
Documentary evidence of inclusion in staff induction.
See above
See above
Policy audit report to:
Trust
Committee
Governance
Policy audit report to:
Trust
Committee
Governance
See above
See above
This document will be monitored to ensure it is effective and to assurance compliance.
In the event of a major flu epidemic or major incident compliance with this policy may be difficult or impossible and will require a risk assessment of the ability to provide safe sedation for procedures carried out by the department.
Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds.
This policy has been assessed accordingly
Title of Policy : Surgical Site Marking Policy
Issue Number: 1
Issue Date: 22 January 2015 Review date: 01 October 2017 (unless requirements change)
Page 11 of 11