Lecture: Renal Physiology
advertisement
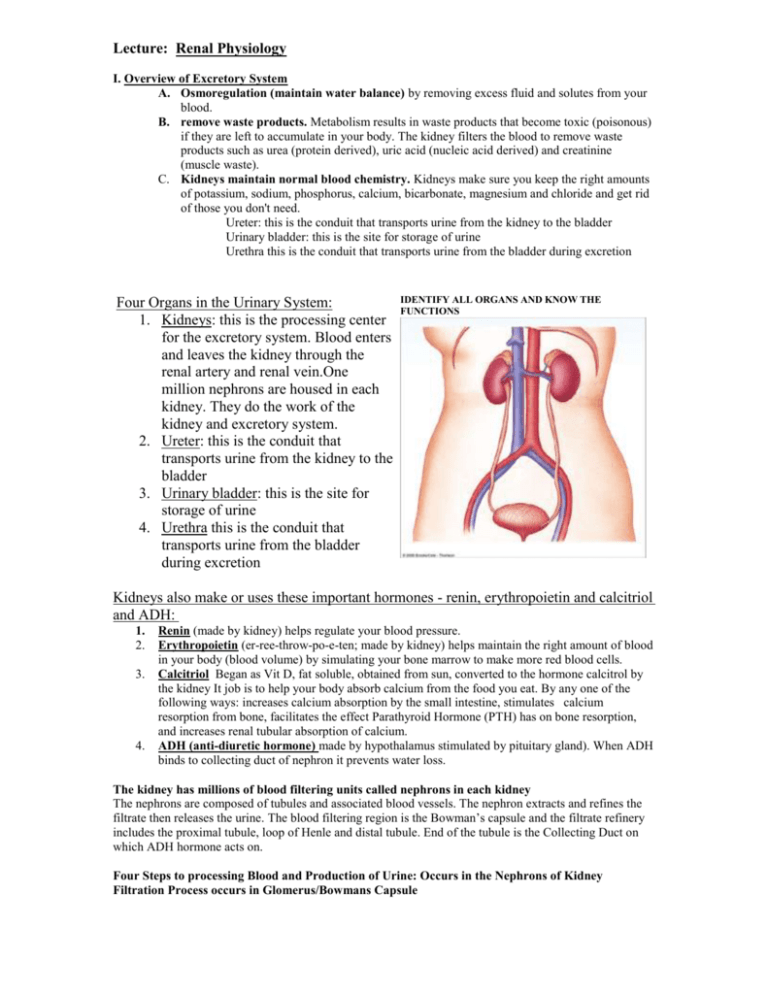
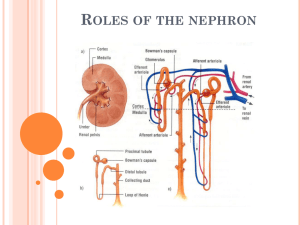
Lecture: Renal Physiology I. Overview of Excretory System A. Osmoregulation (maintain water balance) by removing excess fluid and solutes from your blood. B. remove waste products. Metabolism results in waste products that become toxic (poisonous) if they are left to accumulate in your body. The kidney filters the blood to remove waste products such as urea (protein derived), uric acid (nucleic acid derived) and creatinine (muscle waste). C. Kidneys maintain normal blood chemistry. Kidneys make sure you keep the right amounts of potassium, sodium, phosphorus, calcium, bicarbonate, magnesium and chloride and get rid of those you don't need. Ureter: this is the conduit that transports urine from the kidney to the bladder Urinary bladder: this is the site for storage of urine Urethra this is the conduit that transports urine from the bladder during excretion Four Organs in the Urinary System: 1. Kidneys: this is the processing center for the excretory system. Blood enters and leaves the kidney through the renal artery and renal vein.One million nephrons are housed in each kidney. They do the work of the kidney and excretory system. 2. Ureter: this is the conduit that transports urine from the kidney to the bladder 3. Urinary bladder: this is the site for storage of urine 4. Urethra this is the conduit that transports urine from the bladder during excretion IDENTIFY ALL ORGANS AND KNOW THE FUNCTIONS Kidneys also make or uses these important hormones - renin, erythropoietin and calcitriol and ADH: 1. 2. 3. 4. Renin (made by kidney) helps regulate your blood pressure. Erythropoietin (er-ree-throw-po-e-ten; made by kidney) helps maintain the right amount of blood in your body (blood volume) by simulating your bone marrow to make more red blood cells. Calcitriol Began as Vit D, fat soluble, obtained from sun, converted to the hormone calcitrol by the kidney It job is to help your body absorb calcium from the food you eat. By any one of the following ways: increases calcium absorption by the small intestine, stimulates calcium resorption from bone, facilitates the effect Parathyroid Hormone (PTH) has on bone resorption, and increases renal tubular absorption of calcium. ADH (anti-diuretic hormone) made by hypothalamus stimulated by pituitary gland). When ADH binds to collecting duct of nephron it prevents water loss. The kidney has millions of blood filtering units called nephrons in each kidney The nephrons are composed of tubules and associated blood vessels. The nephron extracts and refines the filtrate then releases the urine. The blood filtering region is the Bowman’s capsule and the filtrate refinery includes the proximal tubule, loop of Henle and distal tubule. End of the tubule is the Collecting Duct on which ADH hormone acts on. Four Steps to processing Blood and Production of Urine: Occurs in the Nephrons of Kidney Filtration Process occurs in Glomerus/Bowmans Capsule The blood vessels of the nephron include a ball of capillaries called glomerus. In the glomerus blood pressure forces water and small solutes (salt, Urea, some sugar)out of the blood and into the nephron tubule. Blood capillaries surround the Nephron . They helps refine the filtrate. Reabsorption of solutes occurs mainly in the Proximal tubules and water in the Loop of Henle: In this process water and solutes still valuable to the body are reclaimed from the filtrate. NaCl and H 2O are reabsorbed by the filtrate in the proximal and distal tubules. The reabsorption of water and Ions (Na and Ca) is under hormonal control (ADH, renin/aldosteron, calcitrol). Secretion: excess ions, drugs and toxins are secreted from the blood into the nephron tubule. Reverse of reabsorption. Excretion: urine passes from the kidney to the outside by way of the urinary bladder and urethra. RENAL DISORDERS Kidney failure: Failing kidneys cannot get rid of excess fluid. Urine output goes down causing a rise in blood pressure, shortness of breath and swelling in many areas of the body. Waste products accumulate. The buildup of waster products in the body results in uremia. Detected by an elevated serum Creatine, (anemia results), abnormal blood pH or abnormal levels of K, Na, Ca. Hematuria (blood in urine) or uremia (urine in blood), high blood pressure, anemia (due to underproduction of erythropoitin) Uremia is "urine in the blood." Uremia affects all the systems in the body When drugs and diet are no longer effective, patients need treatment to do the work of their failed kidneys. If you lose close to 90% of kidney function, they need to start dialysis or have a kidney transplant to stay alive. Dialysis means "to clean the blood." Dialysis removes the waste products and excess water from the body, and stabilizes blood chemistry. Overview of Nephron Structure and Function C. Fluid Processing in the Kidneys 180 liters of blood fluid processes each day 1.5 liters of urine produced each day II. Glomerular Filtration not for Bio 2 Influenced by . Filtration Membrane and Net Filtration Pressure – NFP = glomerular hydrostatic pressure NFP = 55 mm Hg NFP = 55 mm Hg – – (glomerular osmotic pressure ( 30 mm Hg + ( 45 mm Hg ) + capsular ) hydrostatic pressure 15 mm Hg ) NFP = net filtration pressure = 10 mm Hg [This is the NET forces pushing fluid/solutes OUT of blood] Glomerular Filtration Rate (GFR):= milliliters of blood fluid filtered by glomerulus each minute Factors effecting the GFR: total filtration surface area, membrane permeability to fluid/solutes, Net Filtration Pressure. Normal GFR = 125 ml/min (7.5 L/hr, 180 L/day) NFP – primary factor controlling GFR 1. bleeding – NFP drops as blood pressure drops dehydration – NFP dropsas blood pressure drops. --------------------------------------------------------------RENIN-ANGIOTENSIN MECHANISM: Remember this hormone system serves to increase blood volume usually to increase pressure. Drop in blood pressure stimulate glomerular cells to secrete Renin. renin -> anigiotensinogen -> angiotensin I -> (Angiotensin Converting Enzyme (ACE))-> angiotensin II -> global vasoconstrictor (rise in blood pressure) -> aldosterone (reabsorption of more Na+) Factors causing release of Renin: 1. Intrinsic Controls: Reduced stretch of juxtaglomerular cells 2. Extrinsic Controls: Fight or flight (fear and anxiety)– cause increased release of renin epinephrine – causes increased vasoconstriction .;Tubular Reabsorption: is Reabsorbing the Glomerular Filtrate into Blood 1. filtrate - all fluid and its solutes pushed into the capsule 2. urine - filtrate minus reabsorbed substances 3. most sugars and amino acids are reabsorbed 4. water and ion reabsorption depends on hormonal control (see below) A. General Nephron Structure: glomerular filtration. tubular reabsorption, tubular secretion glomerulus – site of filtration from areterial blood ; is this structure a, b, or c? b) proximal tubule– closest to the glomerular capsule most reabsorption occurs here. all glucose & amino acids, 75-80% of water and Na+ a) Loop of Henle – U-turn connecting proximal & distal tubules; Regulates Total water retained or lost; descending limb – relatively impermeable to solutes but freely permeable to water; ascending limb – very permeable to solutes, but not to water d) distal tubule – most secretion from blood e) collecting duct – urine from many nephrons: most affected by hormones ADH, ANH f) peritubular capillaries – “around” the “tubes” (what color yellow or pink) c) Active (energy needed) Tubular Reabsorption: glucose, amino acids, lactate, vitamins, ions a. diabetes mellitus – lower Tm (glucose lost) Passive Tubular Resorption: Na+ driven into interstitial space actively (above) HCO3 and Cl- follow Na+ into the space Non-reabsorbed Substances urea, creatinine, uric acid – most is not reabsorbed because of the following reasons Tubular Secretion Movement from Capilaries to Tubular Cells 1. K+, creatinine, ammonia, organic acids, drugs 2. Primary functions of tubular secretion: moving drugs into the urine,moving more urea & uric acid into urine, removing excess K+ from blood, regulating pH (H+ ion removal) Regulation of Urine Concentration & Volume Osmolarity – Number of Solute particles in 1 Liter water 1. milliosmol (mosm) = 0.001 osmol 2. normal body fluids = 300 mosm Learn from this fig by answering these questions: 1. What color represents the blood vessel and what color is the nephron? 2. Where is blood squeezed out of the capillaries? 3. Where is blood filtrate pushed into? 4. What is happening at b? 5. What nephron structure is b? 6. What is the process call that returns substances from blood to nephron? 7. Where in the nephron does the majority of secretion occur (name nephron structure)? 8. What don't you understand? Formation of Dilute Urine 1. When water removal is needed, no ADH is released, so that the Distal and Collecting Tubules will not actively transport Na+ out; no water moves out 2. Urine may be as low as 50 mosm 3. Diuretics (Stimulate Water Loss) 4. alcohol – inhibits action of ADH 5. caffeine – causes renal vasodilation; increases GFR 6. Prevent Na+ reabsorption say for example a patient with hypertension needs to reduce the blood presssure Formation of Concentrated Urine (Water Conservation) 1. antidiuretic hormone (ADH) – stimulates reabsorption of water in the Distal and Collecting Tubules How to calculate Renal Clearance Not for bio 2 Renal Clearance (RC) – the rate at which the kidney can remove a substance from the blood RC = U/P X V U/P V concentration of substance in urine (mg/ml) = -------------------------------------concentration of substance in plasma (mg/ml) = rate of the formation of urine (ml/minute) (normal = 1 ml/minute) D. Glomerular Filtration Rate = 125 ml/minute; (determined by challenge with “Inulin”) 1. 2. RC < 125 – reabsorption is occurring RC > 125 – tubule cells secrete into the urine Characteristics and Composition of Urine A. Physical Characteristics (Urine should not contain blood (RBC or WBC), proteins, sugars, nitrates, ketones (biproduct of fat metabolism) bilirubin or urobilinogen (breakdown products of hemoglobin via bile) illegal drugs. 1. color – clear to yellowish; influenced by diet, drugs, and health state 2. odor – slightly aromatic; influenced by diet, drugs, and health state 3. pH (H+ conc.) – usually acidic, about pH 6; changes in diet can effect the pH 4. specific gravity – compared density to distilled water; urine slightly heavier (with solutes) B. Chemical Composition 1. 95% water 2. 5% solutes – urea (breakdown of amino acids); uric acid; creatinine Glucose and Ketones are signs of Diabetes Bilirubin and urobilinogen are signs of liver disease Blood and blood cells, either menstruation, bacterial infection, kidney damage WBC bacterial infection (UTI) Proteins suggest kidney damage