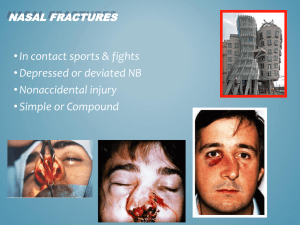
Nasal fracture is the most common facial fracture, and the third most
advertisement

Nasal-Septal Fracture Francis B. Quinn, M.D. Herve’ J. LeBoeuf, M.D. Nasal fracture is the most common facial fracture, and the third most common fracture of the skeleton overall. However, because many fractures are subclinical and many others are associated with multiple trauma, a high percentage are not diagnosed or treated at the time of injury. These often lead to chronic nasal obstruction and account for many of the septoplasty procedures performed for obstruction and septal deviation. Most facial fractures can be restored to their preoperative state with proper early intervention. The following synopsis is a look at the early diagnosis and treatment of nasal fractures with the goal being the prevention of these late complications. Anatomy The external nose is a triangular pyramid composed of cartilaginous and osseous structures that support the skin, musculature, mucosa, nerves, and vascular structures. The upper third of the nose is supported by bone, and the lower two-thirds gains its support from a complicated interrelationship of the upper and lower lateral cartilage’s and the nasal septum. The skin in the upper portion of the nose is freely movable and thin; in the lower portion the skin is thick and has prominent sebaceous glands. In the distal nose the attachment of the skin to the underlying cartilaginous structures is more intimate. The entire nose has an excellent blood supply, which permits extensive dissection with safety and results in early, rapid healing. The supporting framework of the nose is made up of semirigid cartilaginous structures that are attached to the solid and inflexible bone structure of the nose. The cartilaginous tissues include the lateral nasal cartilages, the alar cartilages, and the septal cartilage. There are several sesamoid cartilages in the lateral portions of the ala and in the base of the columella. The cartilaginous structures support the overlying subcutaneous tissue, skin, mucosa, and lining of the nose. The cartilages are intimately attached to the bony structures, which consist of the frontal process of the maxilla, the nasal spine of the frontal bone, the pair of nasal bones, and the bones of the septum, the vomer, and the perpendicular plate of the ethmoid. The paired nasal bones articulate in the midline with each other, and are supported laterally by the frontal processes of the maxilla and superiorly by the “nasal spine” of the frontal bone. The lower third of the nasal bone is thin and broad. In the proximal position the nasal bones are thicker and narrow in their articulation with the frontal bone. The thin portion of the nasal bones is subject to fracture, whereas the thicker portions are more difficult to injure. The nasal bones seldom fracture in the upper portions, but fractures often occur in the lower half. In the upper portions the bones are also firmly supported by an intimate articulation with the frontal bone and frontal process of the maxilla. 1 Pathogenesis Many different and often complex methods of classifying nasal-septal fracture have been proposed. However, the most clinically pertinent understanding of a given nasal fracture lies in each individual patients history. When predicting the amount of damage a patient may have sustained, attention should be given to the patient's age, the instrument they were struck with and the force and direction of the instrument. The fracture patterns seen vary distinctly with the application of frontal and lateral forces. Stranc and Robertson found that lateral forces account for most nasal fractures. They proposed a classification system based on direction and intensity of the blow to the nose in order to estimate structures which may be injured (Appendix I).2 They also found that younger patients tend to have fracture-dislocation of larger segments, whereas older patients (with brittle dense bone) tend to have comminuted fractures. Because of the intimate associations of the bony and cartilaginous portions of the nose with the nasal septum it is unusual to observe fractures to either structure without damage to the other. A common mistake in reduction of nasal fractures is to reduce the bony fracture without attention to the septum, which leads to progressive nasal obstruction as the septum heals with fibrous scar tissue. Septal fractures tend to activate interlocked stresses, and during the process of healing by fibrosis they may produce septal twisting of various configurations (C-shaped, S-shaped, or spurs). Fracture lines are commonly vertical when located anteriorly and horizontal when located posteriorly.3 Septal fractures also are frequently associated with a “telescoping” of the fractured edges causing a retruded appearance of the cartilaginous portions of the nose. Diagnosis With any trauma to the midface, the clinician should be suspicious of the possibility of a nasal fracture. A careful history should be taken of the nature of the incident, whether or not there was any bleeding from the nose, and if the patient notes any external deformity. A nasal fracture is almost certain under these circumstances . The clinician should also inquire about prior nasal obstruction and fracture so as not to confuse pre-existing deformities with an acute injury. A thorough physical exam by an experienced practitioner will reveal most nasal-septal fractures, although patients presenting after 3-6 hours may have significant edema which obscures the fracture. Signs of a fracture include deformity, deviation, abnormal contour, lacerations, mucosal rents, ecchymosis, and hematoma. Signs of more severe fractures include lid edema, scleral chemosis, periorbital ecchymosis, subconjunctival hemorrhage and subcutaneous emphysema.3 2 The exam should begin with topical decongestion of the nasal mucosal after careful debridment of intramucosal blood. Palpation of the bony and cartilaginous structures should be performed both externally and internally for crepitance and dislocation. The tip should be pressed posteriorly and cephalically to ascertain the degree of loss of cartilaginous support. Sharp has found that use of routine x-rays to be financially inefficient and unnecessary.4 Previous studies have shown that nasal films fail to reveal nearly 50% of clinically evident fractures. Furthermore, old fracture lines cannot be differentiated from acute minimally displaced fracture lines. It is noteworthy that some authors continue to advocate nasal films for legal documentation purposes in the absence of an emergency room evaluation by an otolaryngologist. For more severe trauma, such as naso-orbital fractures, nasofrontal ethmoid fractures, or possible cribform plate fractures, axial and coronal computed tomography scans should be obtained. Photographic documentation of the injury should be considered an essential part of the evaluation. Pre injury photographs should also be obtained to understand the patients baseline anatomy. Mayell has noted that approximately 30% of patients with a nasal fracture have pre-existing nasal deformities. Also of note is the high incidence of patient dissatisfaction (25-50% in some studies) with their postreduction outcome. The acute injury phase photographs are helpful to remind the patient of the extent of their deformity prior to surgical intervention. Intervention There are three major considerations in the plan for reduction of a nasal fracture. The first is whether to perform open reduction or closed reduction. Some authors advocate the attempted closed reduction of all but the most severely comminuted nasal fracture if seen within the first two to three weeks post-injury. Even if the patient will need subsequent rhinoplasty, closed reduction assists in both minimizing the extent of rhinoplasty needed, and in the patient's comfort while awaiting rhinoplasty. Bailey lists his recommendation for open and closed reduction in his text. He states the indications for closed reduction as: 1) unilateral or bilateral fracture of the nasal bone; 2) fracture of the nasal-septal complex with nasal deviation less than one half the width of the nasal bridge. The indications for open reduction are stated as: 1) Extensive fracture-dislocation of the nasal bones and septum; 2) nasal pyramid deviation exceeding one half the width of the nasal bridge; 3) fracture dislocation of the caudal septum; 4) open septal fractures; 5) persistent deformity after closed reduction.3 One could also add nasal-septal fractures seen three weeks or more post-injury to this list. The second consideration is the issue of the use of local or general anesthetic. There are a number of articles from England (where OR time is precious) comparing the two techniques.5,6 Various endpoints of reduction were compared, including cosmesis and residual nasal obstruction. The consensus is that both the patient and the physician perceived outcome is statistically insignificant between the two methods. Also of note is that >90% of the patients 3 compared the pain under anesthesia as being equivalent to having dental work done. In this era of cost-containment this is significant, and perhaps more reductions should be performed under local anesthesia. The third major consideration is that of the timing of reduction. If the patient presents in the first 3 to 6 hours (prior to significant distorting edema) , the closed reduction should be performed immediately. After this, most authors advocate delaying the procedure 3-7 days to allow for recession of the edema so that proper realignment may be attained. Most patients do not heal significantly before three weeks and therefore closed reduction may be attempted any time in the first 2-3 weeks. After 3 weeks the fracture has healed such that it cannot be reduced easily and open reduction must be performed. Because of the maturing scar tissue and fibrosing cartilage, rhinoplasty must be delayed 3-6 months to obtain optimal results. Closed Reduction The nose is anesthetized using 4% cocaine as an intranasal solution (maximum adult dose 8ml) with 1:100,000 epinephrine soaked pledgets. This shrinks the nasal mucosa sufficiently to allow adequate intranasal examination. This is supplemented with external nasal field blocks using 2% lidocaine with 1:100,000 epinephrine along the nasal dorsum, lateral to the nasal pyramid, and at the base of the anterior septum. The patient may also be given oral or intravenous sedation to enhance the anesthesia. Although the anesthesia is effective almost immediately, fifteen minutes should be given to maximize the vasoconstrictive property of the medication. The use of EMLA cream has been proposed, but this increases the patient's preoperative preparation time by an hour, and may not be as effective as the previously mentioned regimen. Few instruments need be at hand for fracture reduction. These include Asch and Walsham forceps, a large Kelly clamp with protective rubber tubing over the blades, Boies or Ballenger elevators, intranasal specula and a head light. Almost all nasal fractures can be reduced by upward and outward forces with an instrument placed in the nose under the nasal bone. The instrument is inserted intranasally to a point 1cm caudal to the nasofrontal angle. The depressed fragment is elevated by exerting force in the direction opposite to the fracturing force, usually anterolaterally. If the opposite nasal bone is displaced laterally, that bone is moved medially to its normal position. The Asch or Walsham forceps may be used by inserting one blade in each nostril or by placing one blade in the nose under the nasal bone and the other on the overlying skin. Pressure should not be exerted too high in the nose (under the thick nasal bone near the nasofrontal suture) as this area is rarely fractured and mucosal tears and bleeding can be produced. Reduction can usually be accomplished with the fragments remaining in position, but digital molding may be necessary in some patients. Inadequate reduction of the nasal septum prevents satisfactory repositioning of the external nose in the case of bilateral pyramid fracture-dislocation. Reducing the nasal bone fragments first often reduces the septum simultaneously; if not, the Asch or Walsham forceps usually 4 permit gentle elevation of the nasal pyramid while pressure is applied over the displaced septal region.3 If a septal fracture-dislocation does not reduce easily, the perichondrium may be elevated unilaterally to expose an overriding cartilage fracture that requires sequential resection. If the nasal bones are comminuted or loose, they may be supported with an intranasal antibiotic soaked gauze packing. The septum may by stabilized with silastic splints but the routine use of nasal packing for stable fractures is debatable. A small catheter may be placed along the floor of the nasal vault prior to packing to enhance patient comfort permitting equalization of pressure in the nasopharynx during swallowing, and preventing discomfort of negative pressure in the middle ear. An external splint of placed, consisting of steristrips and mastisol, followed by a heat activated thermal polymer to conform to the patient's nose and an other layer of steristrip. The packing may be removed in 2-3 days, and the splints in 10 days. Fracture stability is checked at the 10 day postoperative visit and if there is instability the external splint should be replaced for another week, otherwise it may be discarded. Because incomplete greenstick fractures of the septum and nasal bones can account for later deviations, Manson recommends that fracture lines be completed prior to reduction. Some authors perform submucous resection on C-shaped septal fractures, but this may cause a loss of nasal height. Dorsal nasal humps can result from this slight loss of dorsal height. A safer method is to attempt closed reduction and warn the patient of possible need for future rhinoplasty.1 If the fracture cannot be reduced by closed reduction, the operation should be immediately converted to an open reduction. For this reason many authors advocate the use of the operating room for all closed reductions. Open Reduction The nose is anesthetized and prepared in the same manner as for closed reduction. The operative procedure chosen is dictated by the patient's type of fracture-dislocation. Most cases needing open reduction are due to an interlocked segment of cartilage and/or bone. The septum is approached though a hemitransfixion incision on the side of dislocation (complete transfixion incisions predispose to lower tip height and introduce additional structural instability). Further access to the fracture line is gained through lateral intercartilaginous incisions. The dorsal skin is elevated off the upper lateral cartilage’s and the periosteum is elevated from the nasal bones. Piriform aperture incisions provide access to the lateral fracture lines. Common findings are dislocation of the quadrangular cartilage off the maxillary crest, or a Cshaped fracture of septal cartilage and bone, as described by Murray and associates.3 The cartilaginous segments are exposed and reduced. Sometimes a segment of cartilage must be resected adjacent to the fracture. A Cottle elevator is used to excise small strips of cartilage, allowing the septum to swing like a "trapdoor" back into its normal position. A small chromic stay suture may be placed through the periosteum near the anterior nasal spine and the inferior 5 portion of the cartilaginous septum to maintain its reduction. Often a displaced maxillary crest must be removed entirely. Radical resection of cartilage or bone is avoided to preserve support and limit fibrosis and contracture. After septal surgery of this type, satisfactory reduction can almost always be accomplished.3 Depressed comminuted fractures should be exposed by judicious periosteal elevation. Overaggressive elevation of the periosteum may cause devitalization of the bone with subsequent necrosis and/or malunion. The fragments may be elevated into position and maintained with fine wires (28 gauze) and a minidrill. There has been some use of miniplates with these fractures, but extrusion of the plate, wound breakdown, and unsightly appearance of the dorsal nasal skin over the plates have limited their utility thus far. The wound is closed in 3 layers- periosteum, subcutaneous tissue, and skin. Packing is rarely necessary to support the fixation. Properly placed wires should not be palpable through the skin, as the ends of the wire may be twisted through a hole or between fragments. Prophylactic antibiotics are administered for five days.1 Mathog also describes an older method of external lead plate fixation of these types of fractures. Septoplasty and rhinoplasty techniques for delayed repair is a broad topic covered in previous grand rounds. Nasal Fracture in Children It is thought that many septal deformities in adults are due to minor trauma as a child or neonate that went unrecognized. As the slight deviation matures, progressive nasal obstruction and deformity occurs. A child’s nose differs from that of an adult in several ways. Specifically, the underdeveloped nose has less frontal projection, is largely composed of cartilage, and possesses several growth centers. As a result, pediatric nasal trauma often presents a unique diagnostic and therapeutic dilemma. The immature nose is more likely to be associated with other fractures of the face because the nasal projection is much less prominent. A blow to the face is, in general, distributed to the adjacent maxilla. Since the child’s nose is more cartilaginous than its adult counterpart, it is easily compressible and absorbs little of the energy from the striking force as it passes across the face. The resultant edema spreads over the face and tends to disguise the extent of the nasal involvement in the pediatric age group. Palpation at the onset of the injury should be attempted; however, the pediatric patient is usually apprehensive, especially shortly after trauma. As a result, the immature patient is likely to be uncooperative and an exacting examination may not be possible. In addition, the large amount of attendant edema with facial trauma, and the lack of rigidity of the nasal skeleton tend to produce a less than optimal situation for evaluation, even in the cooperative patient. An external and intranasal examination should always be performed. The cartilaginous structures of the nose tend to buckle and twist with the trauma rather than to fracture. Operative intervention is indicated for a displaced nasal fracture that results in either a cosmetic deformity or noticeable airway obstruction. 6 Management of nasal fractures in children differs from that in adults in that general anesthesia is usually required. The prevailing method of managing pediatric nasal fractures is closed reduction. The nose with splayed nasal bones and no impactions can be reduced with bilateral digital compression on the dorsum for ten to 15 minutes. Often, nasal deviation to one side can also be reduced by digital compression on the side of the deviation. A difficulty with closed reduction in children is that clear cut end point is difficult to appreciate. The cartilaginous elements do not move into place as readily, and when they are mobilized, they do into ”snap” into place as do adult dislocations. The bony elements frequently are involved in a greenstick fracture and may be resistant to maintenance of the desired postion. Although many nasal surgeons have advocated immediate repair of all septal deviations secondary to birth trauma, correction is necessary only in the case of nasal airway obstruction, as newborns are obligate nasal breathers. 7,8 In one study, nasal fracture was noted to be associated with nasofacial disproportion, especially a long nose, in 21% of the patients who were followed long-term. A long nose deformity was observed to develop during puberty, normally a time of rapid growth for the nose. These findings correlate closely with the observations of Grymer and colleagues,9 who described three periods of nasal development: age 1 to 6 years (rapid growth), 6 to11 years (slow growth), and 12 to 16 years (rapid growth). They recommended that nasal surgery be performed between the ages of 6 to 11 years when practical.3 Early Complications Septal hematoma may develop either as a result of the injury or of the repair and is often bilateral. The fracture allows blood to pass into both mucoperichondrial planes, undrained. This may lead to fibrosis or to organization as a thick obstructive section of septal cartilage. If the hematoma is under excessive pressure, necrosis and perforation are likely results. Loss of septal support will cause collapse of the cartilaginous dorsum with a resultant saddle-nose deformity. If a hematoma is suspect, palpation for fluctuance may be done with cotton-tipped swabs followed by needle aspiration. Treatment is by horizontal incision at the base of the septum so as to produce dependent drainage. Bilateral hematomas are treated with a unilateral offset incisions with preservation of the septum. Silastic splints, light packing, or mattress sutures for 2-3 days will prevent reaccummulation. Edema, ecchymosis, and epistaxis usually resolve spontaneously. Persistent epistaxis should be dealt with in the usual fashion. Infection is a rare complication, but antibiotic prophylactics should be used in immunocompromised patients and those who have hematoma. CSF rhinorrhea is associated with more severe trauma and indicates fracture of the posterior frontal sinus table or the cribriform plate. Diagnosis is easily made by glucose measurements of the rhinorrhea and serum. Neurosurgery should be consulted and the patient observed closely for 6 weeks. Occasionally a lumbar drain or bone grafting may be necessary. Emphysema of the face and neck may also occur and usually resolves spontaneously with avoidance of increases in upper airway pressure. 7 Late Complications Untreated hematomas of the nasal septum may become organized, resulting in subperichondrial fibrosis and thickening with partial nasal airway obstruction. The septum may be as thick as 1cm, and in cases of repeated trauma the cartilaginous septum may be largely replaced with calcified or chondrified material. Submucous resection of the thickened portion of the nasal septum may be required, and in some patients a partial turmbinectomy may be advisable. Synechiae may form between the septum and the turbinate in areas where soft tissue lacerations occur and the tissues are in contact. If bothersome, these may be treated by division followed by the placement of nonadherent, petrolatum-impregnated material between the cut surfaces for a period of five days. During this time, epithelization occurs. Obstruction of the nasal vestibule may occur as a result of malunited fractures of the piriform margin or scar tissue contracture from loss of vestibular lining. Osteotomy of the bone fragments corrects the former; however, the contracture due to loss of soft tissue or scar contraction may require excision of scar, and replacement with skin or composite grafts within the nasal vestibule. Residual osteitis is seen occasionally in compound fractures of the nose or in fractures associated with infected hematomas. Rarely a portion of the bony nasal framework may be lost as a result of infection and may require late replacement with bone grafts. In these cases, appropriate debridement and antibiotics constitute the preferred regimen of treatment. Slight malunion of nasal fractures is common after closed reduction, since the exact anatomic position of the fragments can be difficult to detect by palpation alone, especially in the presence of edema. Residual deviation also occurs owing to release of “interlocked stresses” following fracture of the cartilage. If troublesome, the resulting external deformities may require reconstructive rhinoplasty.1 8 References 1. Manson PN. Facial Injuries. In: Plastic Surgery Volume 2 (Joseph G. McCarthy, ed.) Philadelphia: W.B. Saunders Company,1990. 2. Stranc MF Robertson GA. A classification of injuries of the nasal skeleton. Ann Plast Surg 2:468, 1979. 3. Bailey BJ. Nasal Fractures. In: Head and Neck Surgery - Otolaryngology Volume 1. (Byron J. Bailey. ed) Philadelphia: J. B. Lippincott Company, 1993. 4. Sharp JF, Denholm S. Routine x-rays in nasal trauma: the influence of audit of clinical practice. J Royal Soc Med 87:153-154, 1994. 5. Cook JA, Duncan R, McRae R, Irving RM, Dowie LN. A randomized comparison of manipulation of the fractured nose under local and general anesthesia. Clin Otolaryngol 15:343-346, 1990. 6. Owen GO, Parker AJ, Watson DJ. Fractured-nose reduction under local anesthesia. Is it acceptable to the patient? Rhinology 30:89-96, 1992. 7. Stucker, FJ, Bryarly RC, Shockley, WW. Management of Nasal Trauma in Children. Arch Otolaryngol 110 (1):190-196, 1984. 8. McGraw-Wall BL. Facial fracture in children. Fac Plastic Surg 7(3):198-205, 1990. 9. Pollock RA. NASAL TRAUMA. Pathomechanics and surgical management of acute injuries. Ad Craniomaxillofacial Frac Man 19(1):133-147, 1992. 10. Renner GJ. Management of nasal fractures. Otolaryngol Clin of N Am 24(1):195213, 1991. 11. Pitcock JK, Bumsted RM. Nasal Fractures. In: Oral and Maxillofacial Trauma, Volume 1 (Raymond J. Fonseca, Robert V. Walker, eds.) Philadelphia: W.B. Saunders Company, 1991. 12. Haug RH, Prather JL. The closed reduction of nasal fractures: an evaluation of two techniques. J Oral Maxillofac Surg 49:1288-1292, 1991. 13. Verwoerd CD. Present day of nasal fractures: closed versus open reduction. Fac Plast Surg 8(4):220-223, 1992. 14. Holt GR. Nasal septal fractures. In: English G, ed. Otolaryngology, Vol.4. Philadelphia: JB Lippincott, 1989. 15. Nahum AM. The biomechanics of maxillofacial trauma. Clin Plast Surg 2:59, 1975. 16. Grymer LF, Gutierrez C, Stoksted P. The importance of nasal fractures during different growth periods of the nose. J Laryngol Otol 99:741, 1985. 17. Mathog RH. Nasal Fractures. In: Atlas of Craniofacial Trauma. (Robert H. Mathog, ed)) Philadelphia: W.B. Saunders Company, 1992. 18. Murray JA. Preface. Fracture of the nasal bones. Fac Plas Surg 8(4):3p, 1992. 19. Kurihara K, Kim K. Open reduction and interfragment wire fixation of comminuted nasal fractures. Ann Plast Surg 24(2):179-185, 1990. 9