WHITE BLOOD CELLS DISORDERS
advertisement

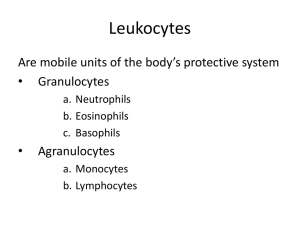
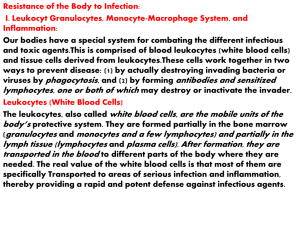
WHITE BLOOD CELLS DISORDERS. Abnoramilities of white blood cells may involve changes in their blood counts, in the normal content of young and mature forms, or emergence of the immature precursors in the peripheral blood. Abnoramilties may also concern the function of leukocyte. Disorders of white blood cells may be classified into two broad categories: proliferative disorders and leukopenias. Proliferation of white cells may be reactive and neoplastic. Normally there are from 4 to 9 х 109 leukocytes/L in the peripheral blood. The table 1. Differential count (per cent) of leucocytes Basophils Eosinophils Neutrophils Monocytes Lymphocytes Metamyelytes band segmented 0-1 2-4 0 3-6 51-67 2-8 20-40 54-73 The leucocytes of the peripheral blood are of 2 main varieties, distinguished by the presence or absence of granulocytes. These are: granulocytes and nongranular leucocytes. The granulocytes, according to the appearance of nuclei, are subdivided into polymorphonuclear leucocytes and monocytes. Depending upon the colour of granules, polymorphonuclear leucocytes are further of 3 types: neutrophils, eosinophils and basophils. The nongranular leucocytes are lymphocytes. (see table) GRANULOPOIESIS. Site of Formation and Kinetics. All forms of granulocytes are produced in the bone marrow and are termed 'myeloid series'. These are: myeloblast (most primitive precursor), promyelocyte, myelocyte, metamyelocyte, band forms and segmented granulocyte (mature form). The myeloblast, promyelocyte and myelocyte form a 'proliferative or mitotic pool', while the latter series i.e. metamyelocyte, band forms and segmented granulocytes make up a 'mature or post-mitotic pool'. It takes about 12 days for formation of mature granulocytes from the myeloblast. Normally the bone marrow contains more myeloid cells than the erythroid cells in the ratio of 2:1 to 15:1 (average 3:1), the largest proportion being that of metamyelocytes, band forms and segmented neutrophils. Normally, the bone marrow storage compartment contains about 10-15 times the number of granulocytes found in the peripheral blood. Following their release from the bone marrow, granulocytes spend about 10 hours in the circulation before they move into the tissues, where they perform their function of phagocytosis. Granulocytes in the peripheral blood commonly adhere to the vascular endothelium (margination). Thus, the blood pool of granulocytes consists of 2 components of about equal size - the circulating pool that is included in the blood count, and the marginating pool that is not included in the blood count. Granulocytes spend about 4-5 days in the tissues before they are either destroyed during phagocytosis or die due to senescence. To control the various compartments of granulocytes, a 'feed-back system' exists between the circulating and tissue granulocytes, and the marrow granulocytes. The presence of a humoral regulatory substance, 'granulopoietin' analogous to erythropoietin has also been identified by in vitro studies of colony-forming units (CFU) and is characterised as G-CSF (granulocyte colony-stimulating factor) and GM-CSF (granulocyte-monocyte colony-stirnulating factor). The kinetics of monocytes is less well understood than that of other myeloid cells. Monocytes spend about 20-40 hours in the circulation after which they leave the blood to enter extravascular tissues where they perform their main function of active phagocytosis. The extravascular life span of tissue macrophages which are the transformed form of blood monocytes, may vary from a few months to a few years. Myeloid Series. The development of myeloid cells from myeloblast takes place in the following sequence (see Figure 1.) Blood cell maturation. Figure 1. Blood cell maturation. 1. MYELOBLAST. The myeloblast is the earliest recognisable precursor of the granulocytes, normally comprising about 2% of the total marrow cells. The myeloblast varies considerably in size (1018 µm in diameter), having a large round to oval nucleus nearly filling the cell, has fine nuclear chromatin and contains 2-5 well-defined pale nucleoli. The thin rim of cytoplasm is deeply basophilic and devoid of granules. The myeloblasts of acute myeloid leukaemia may, however, show the presence of rod-like cytoplasmic inclusions called Auer's rods which represent abnormal derivatives of primary azurophilic granules. The nuclei of successive stages during their development from myeloblast become progressively coarser and lose their nucleoli and the cytoplasm loses its blue colour. As the cells become mature the granules appear; firstly non-specific azurophilic granules appear which are followed by specific granules that differentiate the neutrophils, eosinophils and basophils. 2. PROMYELOCYTE. The promyelocyte is slightly larger than the myeloblast (12-18 µm diameter). It possesses a round to oval nucleus, having fine nuclear chromatin which is slightly condensed around the nuclear membrane. The nucleoli are present but are less prominent and fewer than those in the myeloblast. The main distinction of promyelocyte from myeloblast is in the cytoplasm which contains azurophilic (primary or nonspecific) granules. 3. MYELOCYTE . The myelocyte is the stage in which specific or secondary granules appear in the cytoplasm, and accordingly, the cell can be identified at this stage as belonging to the neutrophilic, eosinophilic or basophilic myelocyte. Primary granules also persist at this stage but formation of new primary granules stops. The nucleus of myelocyte is eccentric, round to oval, having somewhat coarse nuclear chromatin and no visible nucleoli. The myeloid cells up to the myelocyte stage continue to divide and, therefore, comprise mitotic or proliferative pool: 4. METAMYELOCYTE. The metamyelocyte stage is 10-18 µm in diameter and is characterised by a clearly indented or horseshoeshaped nucleus without nucleoli. The nuclear chromatin is dense and clumped. The cytoplasm contains both primary and secondary granules. The metamyelocytes are best distinguished from the monocytes by the clumped nuclear chromatin while the latter have fine chromatin. 5. BAND FORMS. Band form is juvenile granulocyte, 10-16 µm in diameter, characterised by further condensation of nuclear chromatin and transformation of nuclear shape intoband configuration of uniform thickness. 6. SEGMENTED GRANULOCYTES. The mature polymorphonuclear leucocytes, namely: the neutrophils, eosinophils and basophils. 7. Polymorphonuclear neutrophil, commonly called polymorph or neutrophil, is 12-15 μm in diameter. It consists of a characteristic dense nucleus, having 2-5 lobes and pale cytoplasm containing numerous fine violet-pink granules which are predominantly secondary granules which appear at the myelocyte stage. Both primary and secondary granules are lysosomal in origin and contain myeloperoxidase, acid phosphatase and other acid hydrolases, while the secondary granules contain alkaline phosphatase and lysozyme. Monocyte-Macrophage Series. The monocyte-macrophage series of cells, though comprise a part of myeloid series along with other granulocytic series, but are described separately here in view of different morphologic stages in their maturation. 1. MONOBLAST. The monoblast is the least mature of the recognisable cell of monocytemacrophage series. It is very similar in appearance to myeloblasts except that it has ground-glass cytoplasm with irregular border and may show phagocytosis as indicated by the presence of engulfed red cells in the cytoplasm. However, differentiation from myeloblast at times may be difficult even by electron microscopy and, therefore, it is preferable to call the earliest precursor of granulocytic series as 'myelomonoblast'. 2. PROMONOCYTE. The promonocyte is a young monocyte, about 20µm in diameter and possesses a large indented nucleus containing a nucleolus. The cytoplasm is basophilic and contains no azurophilic granules but may have fine granules which are larger than those in the mature monocyte. 3. MONOCYTE. The mature form of monocytic series is described on, while the transformed stages of these cells in various tissues (i.e. macrophages). LYMPHOPOIESIS. Sites of Formation and Kinetics. The lymphocytes and the plasma cells are immunocompetent cells of the body. In man, the bone marrow and the thymus are the primary lymphopoietic organs where lymphoid stem cells undergo spontaneous division independent of antigenic stimulation. The secondary or reactive lymphoid tissue is comprised by the lymph nodes, spleen and gut-associated lymphoid tissue (GALT). These sites actively produce lymphocytes from the germinal centres of lymphoid follicles as a response to antigenic stimulation. Lymphocytes pass through a series of developmental changes in the course of their evolution into lymphocyte subpopulations and subsets. It includes migration of immature lymphocytes to other organs such as the thymus where locally-produced factors act on them. Functionally, the lymphocytes are divided into T and В lymphocytes depending upon whether they are immunologically active in cell-mediated immunity or in humoral antibody response respectively. In man, the В cells are derived from the bone marrow stem cells, while in birds they mature in the bursa of Fabricius. After antigenic activation, the В cells proliferate and mature into plasma cells which secrete specific immunoglobulin antibodies. The T cells are also produced in the bone marrow and possibly in the thymus. Lymphoid Series. 1. LYMPHOBLAST. The lymphoblast is the earliest identifiable precursor of lymphoid cells and is a rapidly dividing cell. It is a large cell, 10-18 µm in diameter, containing a large round to oval nucleus having slightly clumped or stippled nuclear chromatin. The nuclear membrane is denser and the number of nucleoli is fewer (1-2) as compared with those in myeloblast (2-5). The cytoplasm is scanty, basophilic and non-granular. 2. PROLYMPHOCYTE. This stage is an intermediate stage between the lymphoblast and mature lymphocyte. These young lymphocytes are 9-18 µm in diameter, contain round to indented nucleus with slightly stippled or coarse chromatin and may have 0-1 nucleoli. 3. LYMPHOCYTE. The mature lymphocytes are described below. TYPICAL DISORDERS. Leukocytosis and leucopenia. Typical disorders of white blood cell represent on figure 2. Leukocytosis is an elevation in the number of white blood cells (WBCs) that exceeds the upper limitю All types of WBCs may be increased, or only one type. (See WBC types and functions.) Respectively, the specific types of leukocytosis are neutrophilia, lymphocytosis, monocytosis, eosinophilia, or basophilia. The blood count may raises due to: a. Redistribution within the blood, eg, mobilization from the marginal pool. b. Release of neutrophils from the bone marrow. These two processes produce only а temporary rise in the number of white blood cells, without immature cells in blood. c. Increased formation and release from the bone marrow: blood contains immature cells. А sustained neutrophilia саn result only from increased production, as in acute infection and inflammation. Figure 2 Leucocytosis may be physiological and pathological Physiological Leucocytosis Physiological leucocytosis has nо clinical significance, as it is not accompanied by eosinopenia which is а feature of leucocytosis due to inflammation. Also, there are nо immature cells in the blood, since, in most cases, there is mobilization from the marginal pool. It is seen in the following conditions: Newborn infants: The count, which may be high as 15000 to 20,000/mm3, returns to normal by the age of 1 year Food intake and digestion ("digestive leucocytosis") Physical exercise The leucocytes are mobilized from the marginal pool Mental stress Pregnancy: The count may be 12000-15000/mm3. Parturition possibly due to tissue injury, physical stress, pain, hemorrhage Exposure to sun, and to very low temperature Pathological Leucocytosis Pathological Leucocytosis is a rise in the number of WBCs due to disease. Leukocytosis is a normal physiologic response to infection or inflammation. It is seen in Acute bacterial infections with pyogenic (pus forming) organisms: The infection may be localized-boils, abscess, tonsillitis, appendicitis, or generalized, as in septicemia and pyemia, bronchitis and pneumonia, peritonitis, meningitis, etc. Myocardial infarction: The count rises 2-3 days after the coronary thrombosis. Acute hemorrhage: Maximum response in 8-10 hours; return to normal in 8-10 days. Burns: Maximum response in 5-15 hours; return to normal in 23 days. Amebic hepatitis Malignancies: High counts in half the cases; secondary infection enhances the count. Surgical operations: A post-operative rise is seen in all cases (due to tissue injury). The opposite shift beyond the lower limit is designated as leukopenia. The specific types of leukopenia are called neutropenia, lymphopenia, monopenia, eosinopenia etc, depending on the type of cells involved. Physiological leucopenia A decrease of leukocytes under normal conditions is unusual and rare. Exposure to extreme cold, even under arctic conditions and in spite of acclimatization, may reduce the count to only slightly below the 4000/mm3 level. Pathological leucopenia Leucopenia due to disease is almost always due to a decrease in neutrophils (neutropenia), and is seen in the following: Infections with non-pyogenic bacteria: Typhoid and paratyphoid fevers, and sometimes in the protozoal infection malaria. Viral infections: Influenza, mumps, small рох, AIDS (acquired immtlno-deficiency syndrome). Drugs Chloramphenicol, sulphonamides, aspirin, peniclllins, cyclosporins, phenytoin, phenothiazine, etc. Cytotoxic drugs used in treating malignancies may also cause leucopenia by depressing the bone marrow (other blood cells may also decrease). Repeated exposures to X-rays and radium: These are used as radio therapy in cancers. Cheirlical poisons which depress bone marrow: Arsenic, dinitrophenol, antimony, and others. Deficiency of vitamin В12 and folate, malnutrition, starvation, extreme weakness and debility Hypoplasia (partial depression) and aplasia (complete depression) of bone marrow: ie, failure of stem cells due to autoimmunity, and other factors. Pre-leukemic stage of leukemins N'ote it is important to remember that leucopenia due to any cause makes а person more likely to get pyogenic and other infections. Prolonged neutropenia (> 15 days) increases the risk of many other irnfections (consult next experiment for neutropenia). Leukocytosis and leukopenia are not discrete nozological entities, and they are often used as indices of the extent and course of various pathologic processes. Thus, leukocytosis and leukopenia are typical pathologic processes. Compare: High counts of leukocytes also occurs in bone marrow disorders (leukemia), but leukemias are а group of malignant neoplasms (commonly called blood cancer) resulting from an uncontrolled proliferation of hemopoietic stem cells of leucocytes in the bone marrow and lymphoid tissues. Leukemia will be discussed in next chapter. Polymorphs (Neutrophils). The normal functions of neutrophils are as under: 1. Chemotaxis or cell mobilisation in which the cell is attracted towards bacteria or at the site of inflammation. 2. Phagocytosis in which the foreign particulate material is phagocytosed by actively motile neutrophils. 3. Killing of the microorganism is mediated byoxygen-dependent and oxygen-independent pathways. Pathologic variations in neutrophils include variations in count, morphology and defective function. Variation in count. An increase in neutrophil count (neutrophil leucocytosis or neutrophilia) or a decrease in count (neutropenia) may occur in various diseases. Neutrophil leucocytosis. An increase in circulating neutrophils above 7,500/µl is the commonest type of leucocytosis and occurs most commonly as a response to acute bacterial infections. Some common causes of neutrophilia are as under: Acute infections, local or generalised, especially by cocci but also by certain bacilli, fungi, spirochaetes, parasites and some viruses. For example: pneumonia, cholecystitis, salpingitis, meningitis, diphtheria, plague, peritonitis, appendicitis, actinomycosis, poliomyelitis, abscesses, furuncles, carbuncles, tonsillitis, otitis media, osteomyelitis etc. Other inflammations e.g. tissue damage resulting from burns, operations, ischaemic necrosis (such as in MI), gout, collagen-vascular diseases, hypersensitivity reactions etc. Intoxication e.g. uraemia, diabetic ketosis, eclampsia, poisonings by chemicals and drugs. Acute haemorrhage and haemolysis Disseminated malignancies. Miscellaneous e.g. following corticosteroid therapy, idiopathic neutrophilia. Neutropenia. When the absolute neutrophil count falls below 2,500/µ1, the patient is said to have neutropenia and is prone to develop recurrent infections. Some common causes of neutropenia (and hence leucopenia) are as follows: 1. Certain infections e.g. typhoid, paratyphoid,brucellosis, influenza, measles, viral hepatitis, malaria, kalaazar etc. 2. Overwhelming bacterial infections especially inpatients with poor resistance e.g. military tuberculosis, septicaemia. 3. Drugs, chemicals and physical agents which induce aplasia of the bone marrow cause neutropenia, e.g. antimetabolites, nitrogenmustards, benzene, ionsing radiation. Occasionally, certain drugs produce neutropeniadue to individual sensitivity such as: anti-inflammatory (amidopyrine, phenylbutazone),antibacterial (chloramphenicol, co-trimoxazole), anticonvulsants, antithyroids, hypoglycaemics and anti-histaminics. 4. Certain haematological and other diseases e.g.pernicious anaemia, aplastic anaemia, cirrhosisof the liver with splenomegaly, SLE, Gaucher'sdisease. 5. Cachexia and debility, 6. Anaphylactoid shock. 7. Certain rare hereditary, congenital or familialdisorders e.g. cyclic neutropenia, primary splenic neutropenia, idiopathic benign neutropenia. VARIATIONS IN MORPHOLOGY. These are as under: 1. Granules. Heavy, dark staining, coarse toxic granules are characteristic of bacterial infections. 2. Vacuoles. In bacterial infections such as insepticaemia, cytoplasmic vacuolation may develop. 3. Dohle bodies. These are small, round or oval patches, 2-3 um in size, in the cytoplasm. They are mostly seen in bacterial infections. 4. Nuclear abnormalities. These include the following: Sex chrontatin is a normal finding in 2-3% of neutrophils in female sex. It consists of a drumstick appendage of chromatin, about 1 µm across, and attached to one of the nuclear lobes by a thin chromatin strand. Their presence is indicative of 2X chromosomes. A 'shift-to-left' and a 'shift-to-right' (see below). Pelger-Huet anomaly is an inherited disorder in which majority of neutrophils have decreased number of nuclear segments (1-2) and coarsely staining chromatin. The nuclei appear rod-like, dumb-bell or spectacle-like. DEFECTIVE FUNCTIONS. The following abnormalities in neutrophil function may sometimes be found: 1. Defective chemotaxis e.g. in a rare congenital abnormality called lazy-leucocyte syndrome; following corticosteroid therapy, aspiriningestion, alcoholism, and in myeloidleukaemia. 2. Defective phagocytosis due to lack of opsonisation e.g. in hypogammaglobulinaemia, hypocomplementaemia, after splenectomy, in sickle cell disease. 3. Defective killing e.g. in chronic granulomatous disease, Chediak-Higashi syndrome, myeloid leukaemias. Shift to the Left and shift to the right Shift to the left is a term used to describe an increased proportion of immature leukocytes (usually neutrophils) seen in the blood of an individual fighting an infection. Neufirophils enter the blood mostly as bilobed cells, but the number of lobes increases to 5 or more by the end of their short life span of 8-10 hours. The immature neutrophils are frequently referred to as bands or stabs, in the peripheral blood a few myelocytes may presence. Neutrophilic nuclear shift to the left is called regenerative shift and is estimate according to number band form, metamyelcytes and myelcytes in the blood. - hyporegenerative shift is increase quantity of band form (Metamyelcytes and myelcytes are not present) -regenerative shift is except for increase band form, there are metamyelcytes (young forms) in the peripheral blood. -hyperregenerative shift is occurrence of metamyelcytes. It may be seen after a long period of stimulated hematopoiesis, and reflects the exhaustion of the bone marrow. Shift to the right (degenerative shift) is disappearance of younger cells (band form), or/and appearance more segmented form (more then 5 segmentes) Cooke-Arneth count is another method of determination of the shift. The result of counting expresses in the number of lobes of nuclei (younger cells have fewer lobes) is called Cooke-Arneth count. The normal count is shown below: (N1) The nucleus is shaped like the letter C, 5-10% (NZ) The 2 lobes 20-30 (N3) 3 lobes 40-50 (N4) 4 lobes 10-15 (N5-6) 5 lobes or more (N6 = > 6 lobes) 3-5 "Left shift" ("regenerative shift") = N1 + N2 + N3 > 80% indicates hyperactive bone marrow. "Right shift" ("degenerative shift") = N4 + N5 + N6 > 20% indicates hypoactive bone marrow. What is and what is its clinical significance? In a shift to the left, neutrophils will be released from the bone marrow before their final maturation, when the demand for white blood cells is excessive. As the infection or inflammation begins to recede, the release of immature neutrophils stops and mature neutrophils again dominate a blood smear. The 3-lobed cells are fully mature and functionally the most efficient. Thus, presence of younger cells (shift to the left) or more mature cells (shift to the right) in the blood саn provide important information about the rate of formation and release of neutrophils from the bone marrow. Shift to the left or shift to the right may be as at normal amount of leukocyte sach at leukocytosis and leucopenia. Table.Variations in Neutrophil Parameters. Normal numbers of neutrophils Shift to the left Leukoerythroblastic anemia (Physical replacement of normal marrow by fibrosis or neoplasms) Primary neoplasms: early preleukemic myeloid leukemia shift to the right Megaloblastic anemias: folate antagonists 1 Neutrophil leukocytosis Without shift After intake of food, at muscular work, hemorrhage, at easy infections Mild left shift (Mainly mature segmented forms); left shift with high proportion of less mature cells Neutropenia May occur alone or may accompany lymphopenia, thrombocytopenia, anemia Metabolic diseases (uremia, gout); drugs (phenacetin, digitalis); postnecrosis (myocardial infarction, burns); postsurgery; acute infections (pyogenic cocci, Escherichia coli, Proteus, Pseudomonas, less often typhus, cholera, diphtheria) Very severe acute infections, especially in child Infections: many viral infections (hepatitis, measles); some rickettsial infections rare bacterial infections (typhoid fever, brucellosis); malaria; any very severe infection (septicemia, miliary tuberculosis) Acute leukemia Drugs (Sulfonamides analgesics, many others). Marrow aplasia. Including drug–induced Vitamin B12, folate deficiency Autoimmune diseases; (Felty's syndrome) 1 As a rule, the degree of shift amplifies at increase of severety of illness. Lymphocytes. MORPHOLOGY. Majority of lymphocytes in the peripheral blood are small (9-12 µm in diameter) but large lymphocytes (12-16 µm in diameter) are also found. Both small and large lymphocytes have round or slightly indented nucleus with coarsely-clumped chromatin and scanty basophilic cytoplasm. Plasma cells are derived from В lymphocytes under the influence of appropriate stimuli. The nucleus of plasma cell is eccentric and has cart-wheel pattern of clumped nuclear chromatin. The cytoplasm is characteristically deeply basophilic with a pale perinuclear zone. Plasma cells are normally not present in peripheral blood but their pathological proliferation occurs in myelomatosis. Reactive lymphocytes (or Turk cells or plasmacytoid lymphocytes) are seen in certain viral infections and have sufficiently basophilic cytoplasm that they resemble plasma cells. The functions of T and В lymphocytes are in cell-mediated and humoral immune mechanisms respectively: 1. T lymphocytes are associated primarily with 2 main functions: i) Cellular immune reactions mediated by its subsets such as cytotoxic (killer) T cells, and hypersensitivity reaction. ii) Immunoregulatory function by helper cells by regulating the function of other T cells, В cells and haematopoietic stem cells. 2. В lymphocytes as well as their derivatives, plasma cells, are engaged in synthesis of specific immunoglobulin antibodies. PATHOLOGIC VARIATIONS. A rise in the absolute count of lymphocytes exceeding the upper limit of normal (above 4,000/µl) is termed lymphocytosis, while absolute lymphocyte count below 1,500/µl is referred to as lymphopenia. Lymphocytosis. Some of the common causes of lymphocytosis are as under: 1. Certain acute infections e.g. pertussis, infectious mononucleosis, viral hepatitis, infectious lymphocytosis. 2. Certain chronic infections e.g. brucellosis, tuberculosis, secondary syphilis. 3. Relative lymphocytosis is found in viral exanthemas, convalescence from acute infections, thyrotoxicosis, conditions causing neutropenia. Lymphopenia. Lymphopenia is uncommon and occurs in the following conditions: 1. Most acute infections. 2. Severe bone marrow failure. 3. Corticosteroid and immunosuppressive therapy. 4. Widespread irradiation. Monocytes. MORPHOLOGY. The monocyte is the largest mature leucocyte in the peripheral blood measuring 12-20 µm in diameter. It possesses a large, central, oval, notched or indented or horseshoe-shaped nucleus which has characteristically fine reticulated chromatin network. The cytoplasm is abundant, pale blue and contains many fine granules and vacuoles. The main function of monocyte is phagocytosis. Tissue macrophages of different types included in RE system are derived from blood monocytes. PATHOLOGIC VARIATIONS. A rise in the blood monocytes above 800/ml is termed monocytosis. Some common causes of monocytosis are as follows: 1. Certain bacterial infections e.g. tuberculosis, subacute bacterial endocarditis, syphilis. 2. Viral infections. 3. Protozoal and rickettsial infections e.g. malaria,typhus, trypansomiasis, kala-azar. 4. Convalescence from acute infection. 5. Malignancies e.g. cancer of the ovary, stomach, breast. 6. Granulomatous diseases e.g. sarcoidosis, inflammatory bowel disease. 7. Collagen-vascular diseases. Eosinophils. MORPHOLOGY. Eosinophils are similar to segmented neutrophils in size (12-15 µm in diameter), and have coarse, deep red staining granules in the cytoplasm and have usually two nuclear lobes. Granules in eosinophils contain basic protein and stain more intensely for peroxidase than granules in the neutrophils. Eosinophils are involved in reactions to foreign proteins and to antigen-antibody reactions. PATHOLOGIC VARIATIONS. An increase in the number of eosinophilic leucocytes above 400/µl is referred to as eosinophilia and below 40/μl is termed as eosinopenia. Eosinophilia. The causes are: 1. Allergic disorders e.g. bronchial. asthma, urticaria, angioneurotic oedema, hay fever, drug hypersensitivity. 2. Parasitic infestations, e.g. trichinosis, echino-coccosis, intestinal parasitism. 3. Skin diseases e.g. pemphigus, dermatitis her-petiformis, erythema multiforme. 4. Loffler's syndrome. 5. Pulmonary infiltration with eosinophilia (PIE syndrome). 6. Tropical eosinophilia. 7. Malignant diseases with metastases. 8. Irradiation. 9. Miscellaneous disorders e.g. polyarteritis nodosa, rheumatoid arthritis, sarcoidosis. 10. Eosinopenia. Adrenal steroids and ACTH induce eosinopenia in man. Basophils. MORPHOLOGY. Basophils resemble the other mature granulocytes but are distinguished by coarse, intensely basophilic granules which usually fill the cytoplasm and often overlie and obscure the nucleus. The granules of basophils contain heparin, histamine and 5-HT. In the tissues these cells become mast cells. Mast cells or basophils on degranulation are associated with histamine release. PATHOLOGIC VARIATIONS. Basophil leucocytosis or basophilia refers to an increase in the number of basophilic leucocytes above 100/µl. Basophilia is unusual and is found in the following conditions: 1. Myelosclerosis 2. Myxoedema 3. Ulcerative colitis 4. Following splenectomy 5. Hodgkin's disease 6. Urticaria pigmentosa. LEUKEMOID REACTION Leukemoid reaction resembles the picture of leukemia in the peripheral blood. This change consists of increase in the young, or emergence of the immature cells, sometimes blast forms. As in leukemia, leukemoid reaction is usually accompanied by increase in the total cell number. But occasionally cell counts are normal, or even decreased. Leukemoid reaction occurs in massive infection, allergic diseases, in response to extensive tissue damage, hemolysis, or as a result of tumor destruction. The pathophysiology of leukemoid reaction includes focal reactive proliferation of the bone marrow with increased production of precursors, belonging to various hematopoeitic lineages. The concomitant increase in permeability of the blood-marrow barrier leads to leakage of the immature forms into the peripheral blood. Based on the cell type, leukemoid reactions are classified as myelocytic, monocytic, lymphocytic, or mixed, lymphomonocytic, or myelomonocytic. Depending on the total cell counts leukemoid reactions can be leukopenic, leukocytic (from 10,000 to 80,000 leukocytes/μL), or normocytic. Leukemoid reaction appears to be adaptive since it is accompanied by accumulation of functionally active mature leukocytes in the peripheral blood.