Slide 1 - ECDC - Europa - European Centre for Disease Prevention
advertisement

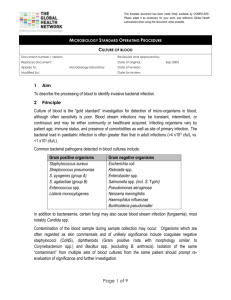
Public health microbiology Disciplines and laboratory methods Ones upon the time there was a microbiologist Epidemiologist????? Which one????? And she found a way; PH microbiologist Objectives of the lecture Define public health microbiology (PHM) Explain role of PHM Give example of PHM disciplines Understand basic methods of characterization of the microorganisms What is Public Health Microbiology (PHM)? “Microbiology is the study of microorganisms, including viruses, fungi, parasites and bacteria including immunity to these microorganisms. Public health microbiology refers to a cross-cutting area that spans the fields of human, animal, food, water, and environmental microbiology, with a focus on human health and disease. Public health microbiology laboratories play a central role in detection, monitoring, outbreak response, and providing scientific evidence to prevent and control infectious diseases. Public health microbiology requires laboratory scientists with ability to work effectively across disciplines, particularly with epidemiologists and clinicians.” Consensus definition for PHM laid out by the group of microbiologists representing the member states of the EU within the ECDC National Microbiology Focal Point Network Why focus on this? Public health is multidisciplinary •Epidemiologists •Laboratory specialists •Clinicians •Veterinarians •Environmental specialists Activities must be •Nurses coordinated to reach •And more… common goals! The Lab – Epi challenge Epidemiologists and lab specialists are infectious disease experts with different: • Perspective and approach • Skills and knowledge • Working habits “The two sides of the same medal” Communication and understanding between Lab and Epi is crucial to the quality of public health investigations! Epi and lab – room for synergy? Infecious disease epidemiology – Hypothesis -> risk factors -> methods to make conlusions from incomplete data Veterinary data Clinical microbiology – Evidence of the presence of pathogen, but not everyone can be sampled and the problems don’t stop there... Environmental data Different laboratories... ...with different roles •Primary health care laboratories •Hospital laboratories •Independent diagnostic laboratories (state, regional or private) •Academic research laboratories •Veterinary Laboratories •Environmental Laboratories •Reference laboratories •Public health laboratories Some important PH Laboratory tasks 1. Confirm diagnosis for targeted interventions (detection, monitoring, outbreak response, and providing scientific evidence) 2. Identify (new) types of pathogens • Population-dynamics • Virulence, persistence, resistance • Implications for control measures 3. Microbiological safety of food and water 4. Quality assurance of diagnostic results 5. Information management, communication and coordination 6. Biosafety 7. Develop new tests/ Optimize existing tests 8. Basic/applied research for new insights and innovative solutions to health problems (vaccine and antibiotic development) Where to find a public health microbiology laboratory regime •Only integrated into the national PH institute, depending on size and development of country (eg. Netherlands) •In a separate institution collaborating with the national PH institute (eg. France, Institute Pasteur) •At the national PH institute and in regional laboratories, depending on infrastructure and size of country (eg. Germany, UK, Sweden) Keep in mind Essential functions of a PHL are not exclusive Many public health laboratories conduct both public health and clinical diagnostic services Many public health laboratories conduct both public health and research Some public health laboratories produce and sell vaccines or biologicals (ex: Cantacuzino Institute, Roumania: diagnostic antisera; Pasteur Institute, Senegal: yellow fever vaccine) Do you know your country's laboratory system? Who is in charge of which disease? Who do you contact in which case? • Local labs • Regional labs • Hospital labs • Reference labs • International lab networks FIND OUT! http://ecdc.europa.eu/en/activities/microbiology/pages/ microbiologicalcooperation_nationalmicrobiologicalfocalpoints.aspx What disciplines do you need at a PH laboratory Bacteriologists / Virologists / Parasitologist Medical Microbiologists Molecular Biologists Immunologists Post doctoral researchers / PhD students Technicians / technical assistance / Analyst Phylogenetic / molecular epidemiology specialists Environmental specialists Zoonosis specialists FIND Epidemiologists/ Statisticians Public Health Microbiologists OUT! …..what is the difference and who is the best contact for what… Conclusions part1: Conditions for successful collaboration between Lab and Epi ( Satu and Sabine share experience with you) Identify common goals Understand that one is not only supporting the other, you work together for the same goals Establish and keep up lines of communication from the beginning to the end Communicate expectations Agree on authorship issues before the start of the project Share data and information efficiently and openly; do not hide data and information Understand that there are different perspectives Recognize different skills Respect different working cultures Part 2: From story to reality Step by step Species versus strains Discriminating features Classification Strain: one single isolate or line Species: related strains Type: sub-set of species Genus: related species Family: related genera Steps in isolation and identification • Step 1: Streaking culture plates – colonies on incubation (e.g 24 hr) – size, texture, color, hemolysis – oxygen requirement Sheep blood agar plate culture Bacillus cereus. Bacillus anthracis CDC/Dr. James Feeley 21 Mixed colonies Isolation and identification Step 2: Colonies Gram stained • cells observed microscopically Gram negative Gram positive Heat/Dry Crystal violet stain Iodine Fix Alcohol de-stain Safranin stain 25 26 Gram stain morphology Gram positive or negative Shape • cocci (round) • bacilli (rods) • spiral or curved (e.g. spirochetes) Single or multiple cells • clusters (e.g. staphylococci) • chains (e.g. streptococci) Step 3: Isolated bacteria are speciated Generally using biophysiological tests Example Salmonella and E-coli Step 4: Antibiotic susceptibility testing Susceptible Not susceptible Bacterial lawn No growth Growth Antibiotic disk DNA structure DNA is usually a double-helix and has two strands running in opposite directions. (There are some examples of viral DNA which are single-stranded). Each chain is a polymer of subunits called nucleotides (hence the name polynucleotide). Molecular differentiation Genomics • Gene characterization – Sequencing – PCR (Polymerase chain reaction ) • • Specific part of a gene 16SrRNA – Restriction digests • Hybridization Genotypic typing methods Fingerprint-based methods – Plasmid profile, RFLP(restriction fragment length polymorphism), PFGE, AFLP Character-based methods – MLVA (Multiple Loci VNTR Analysis), ribotyping (restriction fragments that contain all or part of the genes coding for the 16S and 23S rRNA ), microarray’s Sequence-based methods – MLST – SNP=single nucleotide polymorphism typing Minimum spanning tree of 240 strains Salmonella Enteritidis by MLVA MRSA typed with PFGE & MLST PFGE McDougal LK et al, 2003, J Clin Microbiol 41:5113-20 Noroviruses Norwalk virus Hawaii virus Snow Mountain virus Mexico virus Desert Shield virus Southampton virus Lordsdale virus GI GI.1, GI.2 GII GIII Protein profiling: defining a species by characteristic proteins Proteomics: defining all proteins expressed by a species under specific growth conditions Rapid diagnosis without culture • WHEN AND WHY? • grow poorly • can not be cultured • Need speedy results Bacterial DNA sequences amplified directly from human body fluids • Polymerase chain reaction (PCR) • Great success in rapid diagnosis of tuberculosis. Serologic identification • antibody response to the infecting agent • several weeks after an infection has occurred Diagnostic methods time line time of diagnosis sensitivity - virus isolation 1 – 7 days high* high** - hybridisation 3 – 4 hours high1 good - PCR 3 – 4 hours high2 good 30 min low3 high 3 – 5 hours good4 high - ELISA 3 – 4 hours high low - Immunofluorescence (IFA) - Immunoblot 2 – 4 hours good good 2 – 4 hours good good - Neutralisation/ compliment fixation - HIA 4 – 7 days good high 2 – 4 hours low good Virus detection - Electronmicroscopy - capture ELISA specificity Serology 1 3 ca. 104 particle/ml, 106 particle/ml, 2 4 ca. 200 genome equivalent/ml, ca. 0.01 µg antigen/ml * depending on cultivation system ** depending on detection System Prof. Matthias Niedrig, RKI Conclusion part2: Choice of typing method Pathogen Reproducibility Discriminatory power Exchangeability of data! Study question • Local/global and short/long term epidemiology Availability and resources ? Acknowledgment