November 3 Part 2
advertisement

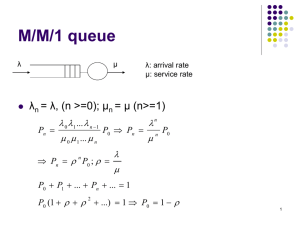
Capacity Setting and Queuing Theory BAMS 580B Capacity and Resources A key lever for improving patient flow. How do we measure capacity? What is the capacity of a 20 seat restaurant? A 16 bed ward? Capacity is a RATE Patients/day Customers/hour We can view a 16 bed ward as a queuing system with 16 servers What is the capacity of a bed? Does this analogy apply to the restaurant? A system is composed of resources with capacities. Often we use the expressions “resource” and “capacity” interchangeably (hopefully without confusion) How Much Capacity is Needed? or How Many Resources are Needed? Ward Occupancy 30 Midnight census Surge capacity 25 Base capacity 20 15 0 100 200 Day 300 400 Capacity tradeoffs when demand is variable Too much capacity or too many resources = idleness Not enough capacity – waits Should we set capacity equal to demand? What does this mean? This is called a balanced system It works perfectly when there is no variation in the system It works terribly when there is variation! Why? • Once behind, you never can catch up. Queuing theory quantifies these tradeoffs in terms of performance measures. Queuing Models (Mathematical) queuing models help us set capacity (or determine the number of resources needed) to meet: Service level targets Average wait time targets Average queue length targets Queuing models provide an alternative to simulation They provide insights into how to plan, operate and manage a system Where are there queues in the health care system? A single server queuing system Buffer Server • A queue forms in a buffer • Servers may be people or physical space • The buffer may have a finite or unlimited capacity • The most basic models assume “customers” are of one type and have common arrival and service rates A multiple server queuing system Server Buffer Server Server Several parallel singer server queues Buffer Buffer Buffer Server Server Server Parallel Queues vs. Multiple server Queues Provide examples of multiple server queues (MSQs) Provided examples of parallel queues (PQs) In what situations would each of these queuing systems be most appropriate? Why? Networks of queues Most health care systems are interconnected networks of queues and servers with multiple waiting points and heterogeneous customers. What examples have we seen in the course? Often we model these complex systems with simulation. • But in some cases we can use formulae to get results Queuing Theory background Developed to analyze telephone systems in the 1930’s by Erlang. How many lines are needed to ensure a caller tries to dial and obtains a “line”. Applied to analyze internet traffic, telecommunications systems, call centers, airport security lines, banks and restaurants, rail networks, etc. Queues and Variability There are two components of a queuing system subject to variability The inter-arrival times of “jobs” The service times or LOS Why are these variable? We describe the variability by Mean Standard deviation Probability distribution • Usually the normal distribution doesn’t fit well • Often an exponential distribution fits well – If we know its rate or mean we know everything about it. The exponential distribution P(T ≤ t) = 1 – e-λt The quantity λ is the rate. The mean and standard deviation of the exponential distribution is 1/rate (1/λ). Example; Patients arrive at rate 4 per hour. The mean interarrival time is 15 minutes. What is the probability the time between two arrivals is less than 10 minutes (1/6 of an hour) • P( T ≤ 1/6) = 1 – e-4∙(1/6) = 1- e-2/3 = 1 - .487 = .513. The exponential distribution underlies queuing theory. A queue with exponential service times and exponential inter-arrival times and one (FCFS) server is called an M/M/1 queue. Exponential distributions don’t allow negative times and have a small probability of long service times. Capacity management and queuing systems Capacity management involves determining the number of servers to use and the size of the waiting rooms. Examples How many long term care beds are needed? How many porters are needed? How many nurses are needed? How many cubicles are needed in an ED? Some healthcare systems have no buffers; all the waiting is done outside of the system or upstream. ALC cases waiting for LTC beds Analyzing a queuing system Outputs Inputs Arrival Rate Service Rate Number of Servers Buffer Size Queue Analyzer QUEUMMCK_EMBA.xls Capacity Utilization Wait Time in Queue Queue Length Blocking Probability Service Levels Single server queues – some definitions Ri – average inflow rate (customers/time) () 1/Ri – average time between customer arrivals Tp – average processing time by one server 1/Tp – average processing rate of a single server () c – number of servers Rp = c/Tp – system service rate (often c=1) K – buffer capacity (often K=) A single server queuing system is stable whenever Rp > Ri A single server queuing system is balanced whenever Rp = Ri Examples A Finite Capacity Loss System Model for an (old-fashion) phone system • c servers • K=0 • When all servers are busy, system is blocked and customers are lost Performance measure – fraction of lost jobs – this is legislated! Walk-in Clinic with 6 seats and 1 doctor c=1 K=6 Characteristics and Performance Measures System characteristics Traffic Intensity (or utilization) = = arrival rate/service rate Safety Capacity = Rs = Service rate – arrival rate Performance Measures Average waiting time (in queue) – Ti Average time spent at the server - Tp Average flow time (in process) – T = Ti + Tp Average queue length – Ii Average number of customers being served - Ip Average number of customers in the system – I =Ii + Ip Performance measure formulas (M/M/1 queue – no limit on queue size) System Utilization = P(Server is occupied) = If traffic intensity increases, the likelihood the server is occupied increases This occurs if the arrival rate increases or the service rate decreases P(System is empty) = 1- P(k in system) = k(1- ) Average Time in System = 1/ Safety capacity Average Time in Queue = Average time in system – average service time If safety capacity decreases; time in queue increases! Average Number of jobs in the system (including being served) = /(1- ) Average Queue Length = 2/(1- ) If we know safety capacity, service time and traffic intensity, we can compute all system properties Little’s Law holds too number in queue = arrival rate x waiting time in queue An Example - M/M/1 Queue Customers arrive at rate 4 per hour, mean service time is 10 minutes. Service rate is 6 per hour System utilization = Probability the server is occupied = = 2/3. Safety capacity = service rate – arrival rate = 2 P(System is empty) = 1- = 1/3. P(k in the system) = k(1- ) = (1/3)(2/3)k Average Time in system= 1/safety capacity = ½ hour Average Time in queue = Average time in system – average service time = ½ - 1/6 = 1/3 hour Average Queue Length = 2/(1- ) = 4/3 Suppose arrival rate increases to 5.9 customers per hour. Then =5.9/6 = .9833 So P(System is empty) = .0167; Average time in system = 10 hours and Average number of customers in the system = 58.9! About QUEUMMCK.xls An M/M/c queue is the same as an M/M/1 queue except that there may be more than one server. In this model, there is a single buffer and c servers in the resource pool. Customers are processed on a FIFO basis. When there are more than c customers in the system, the buffer is occupied and waiting for service occurs. An M/M/c/K queue is an M/M/c queue with a finite buffer of size K. There are at most K + c customers in the system. When the buffer is filled, the system is blocked and customers are lost. QUEUMMCK.xls, which is now called performance.xls, computes performance measures including blocking probabilities for the M/M/c/K queue. Problem 1 Patients arrive at rate 5/hr. They require on average 1 hour of treatment. How many service providers do we need to ensure that the average wait time is 30 minutes? Assume a large waiting room. Running QUEUEMMCK.xls we find that with 6 service providers - average wait is 1 hour and average number waiting is 2.94 7 service providers - average wait is ½ hour and average number waiting is .80 Note that with 7 service providers all 7 are occupied less than 1% of the time. Thus we tradeoff throughput with capacity utilization Problem 2 – A LTC Facility Bed requests arrive at the rate of 3 per month Patients remain in beds for about 15 months. How many beds are required so that the average wait for beds is 1 month. Trial and error with queummck shows that 59 beds are required. Also we can see that there is only a 3% chance of waiting and average occupancy is 45 beds. We can also do sensitivity analysis with arrival rates and length of stays Problem 3 A walk in clinic has 3 doctors; Average time spent with a patient is 15 minutes Patients arrive at rate of 12 per hour How many chairs should we have in the waiting room so only 5% of patients are turned away? Queummck suggests 17. Implications of queuing formulas As the safety capacity vanishes, or equivalently, the traffic intensity increases to 1: waiting time increases without bound! queue lengths become arbitrarily long! In the presence of variability in inter-arrival times and service times, a balanced system will be highly unstable. These formulas enable the manager to derive performance measures on the basis of a few basic descriptors of the queuing system The arrival rate The service rate The number of servers When the system has a finite buffer, the percentage of jobs that are blocked can also be computed Don’t Match Capacity with Demand If service rate is close to arrival rate then there will be long wait times. Recall average queue length = 2/(1- ) • If traffic intensity near 1, queue length will be very small. Queue Length vs. Traffic Intensity 120 100 80 60 40 20 0 0.5 0.6 0.7 0.8 0.9 1 Idle Capacity And Wait Time Targets Relationship between Wait Times and Idle Capacity Proportion of Patients Exceeding Wait Time Target 100 75 To ensure only 5% of patients exceed wait time target, there will be idle capacity 23% of the time. 50 25 0 0 20 Percentage of time there is idle capacity 40 Summary When the manager knows the arrival rate and service rate, he/she can compute: The average number of jobs in the queue. The average time spent in the queue. The probability an arriving patient has to wait. The system utilization. This can be done without simulation! This information can be used to set capacity or explore the sensitivity of recommendations to assumptions or changes. Thus queuing theory provides a powerful tool to manage capacity.