1. An introduction to drugs, their action and discovery
advertisement

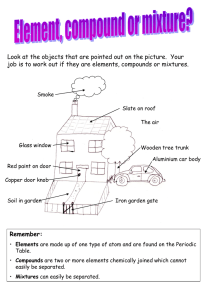
1. An Introduction to Drugs, Their Action and Discovery The basic concepts in Medicinal Chemistry 1.1 Introduction • Primary objective- design and discovery of new compounds that are suitable for use as drugs • A team of workers- chemistry, biology, biochemistry, pharmacology, mathematics, medicine and computing, amongst others • Requires of drug discovery or design- synthesis of the drug, a method of administration, the development of tests and procedures to establish how it operates in the body, and a safety assessment • Drug discovery may also require fundamental research into the biological and chemical nature of the diseased state. • Medicinal chemists need to have an outline knowledge of the above mentioned aspects. 1.2 What are drugs and why do we need new ones? • Definition of drug -chemical substances that are used to prevent or cure diseases in humans, animals and plants • Activity - pharmaceutical/pharmacological effect on the subject, e.g. analgesic or βblocker • Potency - the quantitative nature of the effect • The word “Drug” usually defined as agent used for the psychotic effect by the media or general public. • Even the drugs abused have their activity. • Drugs act by interfering with biological processes, so no drug is completely safe. • That is, suitable quantity to cure or excess to be poisonous! E.g. aspirin, paracetamol can be toxic if excesses. • Side effect – unwanted effect usually; however, they are not always non-beneficial • For example, the drowsiness side effect of anti-histamine may help sleep. • Drug resistance or tolerance (tachyphylaxis) occurs when a drug is no longer effective in controlling a medical condition. • Reasons – induced oxidases in the liver that are able to metabolize the drug; a special enzyme induced to metabolize the drug; down regulated drug receptors Therapeutic index • Chemotherapeutic index = Minimum curative dose /Maximum tolerated dose • By Ehrlich in search of a safer antiprotozoal agent in 19th century -- more effective drugs showed a greater selectivity for the target microorganism than its host • Therapeutic index = LD50/ED50 1.3 Drug discovery and design: a historical outline • Origin of drugs – natural products from plants, animals, and/or minerals since ancient time • Drugs ↔ Poison = pharmakon in Greece, and the criteria can be ‘quantity’ usually • Information about usages and toxicity of drugs were limited by communication until the invention of printing press in 15th century→ Herbals and Pharmacopeia↑ → drug misuse or abuse ↑ →→ the ineffective and/or more toxic preparations removed by the practitioners Evolution and revolution • Early 19th – plant extracts and pure isolates from medicinal plants appearedSome of these drugs were very toxic • Late 19th, to find less toxic medicines than those based on natural sources → synthetic substances as drugs • Early 20th synthetics dominated the main origin of therapeutic drug origins • Leads – the known pharmacologically active chemicals used in drug design and development • Analogues – the-lead related compounds Therapeutic index • Paul Ehrlich and Sacachiro Hata who produced arsphenamine in 1910 – in the search of more effective anti-microbiotic agents: Atoxyl, Arsphenamine (Salvarsan) Therapeutic index Therapeutic index Minimum curative dose Maximum tolerated dose ED50 LD50 • The term structure–activity relationship (SAR) is now used to describe Ehrlich’s approach to drug discovery, which consisted of synthesizing and testing a series of structurally related compounds (see Chapter 3). ONa As O OH H2N Atoxyl H2N NH2 HClx2 HO As As Arsphenamine (Salvarsan) OH QSAR – quantitative structure–activity relationship • 1960s that Hansch and Fujita devised a method that successfully incorporated quantitative measurements into structure–activity relationship determinations • The most successful uses of QSAR has been in the development in the 1970s of the antiulcer agents cimetidine and ranitidine. • Both SAR and QSAR are important parts of the foundations of medicinal chemistry. Concept of Drug Receptor • In 1905 John Langley proposed that so-called receptive substances in the body could accept either a stimulating compound, which would cause a biological response, or a non-stimulating compound, which would prevent a biological response. • Receptor sites (Chap. 8) usually take the form of pockets, grooves or other cavities in the surface of certain proteins and glycoproteins in the living organism. • Ligand – The binding of a chemical agent, referred to as a ligand, to a receptor sets in motion a series of biochemical events that result in a biological or physiological effect. • Stereoelectronic structure: Both as regards molecular shape and electron distribution, is complementary with the stereoelectronic structure of the receptor responsible for the desired biological action. • The drug conformation adopted when binds to the receptor is known as active conformation. • The section of the structure of a ligand that binds to a receptor is known as its pharmacophore. • E.g., the “quaternary nitrogens” that are believed to form the pharmacophore of the neuromuscular blocking agent tubocrarine are separated in the molecule by a distance of 115.3 nm. H3CO + CH3 HO O H2C H H3C + N (S) H N H CH3 CH2 (R) O OH OCH3 (+)-Tubocurarine chloride 2Cl- • Esters and N-substituted amides, for example, have structures with similar shapes and electron distributions but N-substituted amides hydrolyze more slowly than esters. • However, changing a group or introducing a group may change the nature of the activity of O O the compound. R' R' O N R H Amide R Ester O N O N O N H NH2 Procaine (anaesthetic) NH2 Procainamide (antiarrhythmic) Membranes • Drugs normally have to cross non-polar lipid membrane barriers (see sections 7.2 and 7.3) in order to reach their site of action. As the polar nature of the drug increases it usually becomes more difficult for the compound to cross these barriers. HN N O O N O N Physostigmine O Neostigmine N+ Modern Techniques • Computerized molecular modeling (1970s) – allows the researcher to predict the threedimensional shapes of molecules and target, calculate the binding energy, and reduced the need to synthesize every analogue of a lead compound • Combinatorial chemistry (1990s) – originated in the field of peptide chemistry but has now been expanded to cover other areas. • simultaneous production of large numbers of compounds, known as libraries, for biological testing. • Used for structure–activity studies and to discover new lead compounds. • The procedures may be automated. 1.4 Leads and analogues: some desirable properties • Bioavailability – Lipinski’s rules to predict a molecule to be likely orally bioavailable 1. a molecular mass less than 500; 2. a calculated value of log P* less than 5; 3. less than ten hydrogen bond acceptor groups (e.g. -O- and -N-, etc.); 4. less than five hydrogen bond donor groups (e.g. NH and OH, etc.). ⃰ P = partition coefficient of octanol/water Solubility • Any compounds that are potential drug candidates have to be soluble to some extent in both lipid and water. • Ideal leads and/or analogues have a balance between their water solubility and their lipophilicity. Structure • The nature of the structures of leads and analogues will determine their ability to bind to receptors and other target sites. • Binding forces between a drug and a receptor – electrostatic bonds, such as hydrogen bonds and van der Waals’ forces, ion pair, and Cl covalent bond N HOOC NH2 Cl Melphalan DNA Alkylating agent • A major consideration in the selection of leads and analogues is their stereochemistry. • It is necessary to pharmacologically evaluate individual enantiomers as well as any racemates. Cl OH N (Z) (E) H N chloroquine R=S form N HO HO 7 (potency) 100 (potency) diethylstilbestrol OH Stablility • Stability after administration and shelf-life • Three strategies are commonly used for improving a drug’s in situ stability: 1. modifying its structure; prepare a more stable analogue with the same pharmacological activity 2. administering the drug as a more stable prodrug 3. using a suitable dosage form Create a more stable analogue OH Hydrolysis N N O O Pilocarpine (active) N pH=7.4 OH N N N O Pilocarpic acid (inactive) N O O Carbamate analogue Forming a complex • Cyclodextrins are bottomless flower-potshaped cylindrical oligosaccharides consisting of about 6–8 glucose units. The exterior of the ‘flower-pot’ is hydrophilic in character whilst the interior has a hydrophobic nature. • water solubility, bioavailability and pharmacological action ↑ • ↓ side effects Prodrug formation H N O P O N Cl Cl Cyclophosphamide H HN O P HO N Cl Cl Phosphoramidate mustard Shelf-life • Shelf-life is the time taken for a drug’s pharmacological activity to decline to an unacceptable level. • 10 % decomposition is often taken as an acceptable limit provided that the decomposition products are not toxic. • deterioration – microbial degradation and adverse chemical interactions and reactions • Adverse chemical interactions between the components of a dosage form can also be avoided by the use of suitable excipients. • Decomposition by chemical reaction – heat, light, atmospheric oxidation, hydrolysis by atmospheric moisture and racemization


![Shark Electrosense: physiology and circuit model []](http://s2.studylib.net/store/data/005306781_1-34d5e86294a52e9275a69716495e2e51-300x300.png)