Bio 20 Excretion notes
advertisement

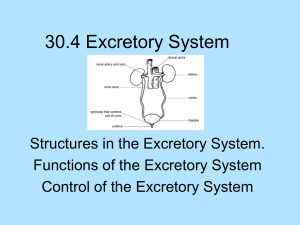
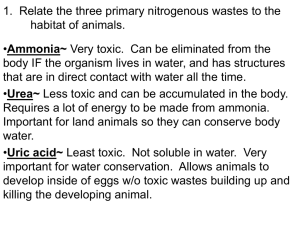
Excretory System Excretion is the process by which the body rids itself of metabolic wastes. The lungs eliminate carbon dioxide The large intestine eliminates toxic digestive waste The liver changes toxin and products of protein metabolism into soluble compounds that the kidney can collect and eliminate. The role of the liver: Excess protein is converted to carbohydrates by a process called deamination. This involves the removal of an amino group from amino acids to produce a carbohydrate and ammonia (a toxic gas). Two molecules of toxic ammonia react with carbon dioxide to produce urea. Urea is about 100,000 x less toxic than ammonia and can be safely transported through the bloodstream. Nucleic acids are also broken down into uric acid. Excess uric acid can cause kidney stones or gout. All of the waste products made by the liver travel through the blood and are then filtered by the kidney. The role of the kidneys: 1. Main role: Removal of poisonous nitrogenous wastes 2. Maintenance of blood pH 3. Maintenance of water balance 4. Maintain blood pressure Urinary System Blood is carried to the paired kidneys from renal arteries that branch off the aorta. The kidney’s can hold as much as 25% of the entire blood supply at any given time. Wastes are then filtered by the kidneys and taken to the urinary bladder via the ureters. 0000template2 Urinary System Anatomy A sphincter muscle at the base of the urinary bladder acts as a valve and released stored urine through the urethra when the muscles relax. The signal to urinate is relayed to the brain when the bladder is about 200 mL full of urine. The liquid in the bladder cause the walls to stretch, stimulating receptors. At 400 mL volume, the signal will be of increasing strength and urgency, and at a 600 mL volume, the sphincter muscles relax, voluntary bladder control is lost and urination occurs. Howstuffworks "Urination" Remember, that when you drink fluids, the fluid goes to your stomach first, and is then absorbed by the body. The loss of bladder control only occurs when much more than 600 mL is processed, absorbed, filtered and finally collected in the bladder. The bottom line: You won’t lose bladder control from drinking a Big Gulp or Slurpee. Input doesn’t equal output when it comes to excretion. Your body retains much of the fluid it consumes for normal processes. The Kidneys Cortex A cross section of the kidney reveals the anatomy of three major structures: 1. The cortex 2. The medulla 3. The renal pelvis Renal Pelvis Medulla Detailed Kidney Structure A cross-section of the kidney reveals the anatomy of three major structures: cortex, medulla, and renal pelvis ureters – tubes that conduct urine from the kidneys to the bladder renal artery - delivers blood to the kidney renal vein – sends blood back to the body renal calyces – outer extensions of the renal pelvis that filter blood cortex – outer layer of connective tissue medulla – inner layer beneath the cortex, hold the major part of the nephron renal pelvis – hollow chamber that joins the kidney with the ureter The Nephron Blood Pathway: The nephron is the functional unit of the kidney. There are about 1 million of these slender tubules in the kidney. These tubules are supplied with blood from the afferent arterioles which branch from the renal artery. They lead into a high pressure capillary bed called the glomerulus. This is where filtration occurs. Blood leaves the glomerulus via the efferent arterioles and is carried to a capillary network, called the peritubular capillaries, that wraps around the kidney tubule. Blood is then transferred to a renal vein. Then back to the venous blood system http://www.wisconline.com/objects/AP2504/AP2504.swf Filtrate Pathway: The glomerulus is surrounded by a cup-like portion of the nephron called Bowman’s capsule. The cortex contains Bowman’s capsule, afferent and efferent arterioles. Fluids to be processed into urine enter Bowman’s capsule from the glomerulus. Next, fluids move through the proximal/distal tubules and then into the collecting ducts which collect urine from many different nephrons and merge into the renal pelvis. kidney patient guide - healthy kidney Urine Formation- Removal of Wastes Formation of urine depends on filtration, re-absorption and secretion. Filtration – is accomplished by the movement of fluid into Bowman’s capsule. Blood moves through the afferent arteriole to the glomerulus and small dissolved solutes (glucose, aa, urea, uric acid, ammonia, and salts) and water pass into Bowman’s capsule (much lower pressure). The pressure gradient allows only some substances to be filtered. Red blood cells, plasma proteins, white blood cells, platelets are too large to pass through. Nephron Information Center Re-absorption – involves the transfer of essential solutes (glucose, aa, vitamins, salts, K+,and H+) and water from the nephron, back into the blood. This is very important in maintaining the body’s water balance. About 85% of filtrate is re-absorbed. (Remember the Big Gulp: If you drink a 1L Big Gulp, about 850 mL of the fluid is reabsorbed, and only 150 mL is collected in the bladder. You don’t even feel like you have to “go” yet.) -Re-absorption mostly occurs in the proximal tubule, with some minor solutes being reabsorbed in the distal tubule -Most water re-absorption occurs in the descending limb of the Loop of Henle Steps involved in re-absorption: 1. Na+ is actively transported out of the nephron. 2. Cl- and HCO3- follow Na+ by charge attraction. 3. The resulting osmotic gradient draws water from the nephron into the blood. (Remember, water follows salt) 4. An additional osmotic gradient is created by plasma proteins that stay in the blood. (They were too big to pass through Bowman’s capsule) 5. Urea and uric acid may diffuse out as well, but will be reabsorbed later Re-absorption occurs until a threshold level of substance is reached. Excess amounts of glucose and salts in the blood will not be re-absorbed and will be excreted in the urine. This is why urine tests can tell us about our blood chemistry. Tubular Secretion – involves the movement of materials from the blood back into the nephron. Nitrogen containing wastes (urea, uric acid), histamines, excess H+ (that regulate pH), minerals, drugs, penicillin, etc. are all removed from the body by the cells in the distal tubule, which actively transports these substances back to the nephron. The distal tubule contains loads of mitochondria to keep up with this energy demand. http://cpharm.vetmed.vt.edu/VM8314/Nephr onMovie.swf Regulating Water Balance Antidiuretic Hormone (ADH) helps regulate the osmotic pressure of body fluids by causing the kidneys to increase water reabsorption, producing more concentrated urine. ADH makes the distal tubules more permeable to the last 15% of water can be reabsorbed into the blood. Special nerve receptors called osmoreceptors located in the hypothalamus in the brain detect changes in the osmotic pressure of the blood and stimulate or inhibit the secretion of ADH. These receptors also elicit the thirst response, inspiring you to increase fluid consumption. Substances such as alcohol and caffeine decrease the release of ADH, resulting in increased urine output and dehydration. Blood Pressure The kidneys regulate blood pressure by regulating the amount of fluid in the blood. More fluid means higher pressure. The hormone aldosterone, acts on the nephrons to increase sodium (salt) re-absorption from the distal tubule, back into the blood. Chloride ions and water will follow, causing the blood volume to increase. Aldosterone is secreted by the adrenal cortex, just above the kidney. A drop in blood pressure is detected by the juxtaglomerular apparatus, located near the glomerulus. This causes the release of liver proteins, angiotensinogen and rennin, which stimulate the release of aldosterone from the adrenal gland. http://www.wisconline.com/objects/AP2204/AP2204.swf pH Balance Despite the variety of foods and fluids with different pH levels we consume, our bodies maintain a relatively constant pH between about 7.3 and 7.5. A relatively stable pH is maintained by a buffer system that absorbs excess H+ ions or basic ions. Bicarbonate ions (HCO3-) are key components of this system: HCO3- + H+ === H2CO3 === H2O + CO2 Bicarbonate ions in the blood remove excess H+ ions, but the buffer must be restored for this system to continue working indefinitely. The kidneys reverse this reaction. Carbon dioxide is actively transported from the peritubular capillary and combines with water to produce HCO3- and H+ ions. The bicarbonate ion diffuses back into the blood and the H+ ions combine with phosphate or ammonia and are excreted in the filtrate. The pH balance is mostly controlled by the distal tubule of the nephron Acid-Base Balance Kidney Dysfunction Diabetes Mellitis – is caused by the inadequate secretion of insulin from the pancreas. Without insulin, blood glucose levels are extremely high, and excess glucose remains in the nephron. The high osmotic gradient prevents water reabsorption and increases urine production. Diabetes Insipidus – is caused by inadequate production of Anti-Diuretic Hormone (ADH). Without ADH, urine input increases dramatically, as much as 20 L per day and the patient will be extremely thirsty. Nephritis – ‘Bright’s Diseases’ is inflammation of the nephrons which can have a variety of causes. Protein in the urine is a common symptom of nephritis. The osmotic gradient also causes an increase in urine production. Nephritis can lead to irreversible kidney damage and eventual kidney failure. Kidney Stones – are caused by the precipitation of mineral solutes form the blood. The stones lodge in the renal pelvis or the ureter, causing major pain and bleeding. Stones can be removed by surgery or by using ultrasonic waves that blast the stones into smaller fragments. Dialysis – is used for patients whose kidneys no longer function properly. Hemodialysis – a machine is connected to the patient’s circulatory system by a vein. Blood is pumped through a series of tubes submerged in solutes that removed waste from the blood. kidney patient guide - Haemodialysis animation Peritoneal Dialysis – is done through the lining of the abdominal cavity. A catheter tube is inserted and solution is fed into the abdominal cavity for two to six hours. This fluid collects wastes from the body and is drained from the catheter when the process is complete. kidney patient guide - How Peritoneal Dialysis works animation Kidney Transplant kidney patient guide - Kidney Transplant animation