HMP SHUNT & URONIC ACID PATHWAY
advertisement

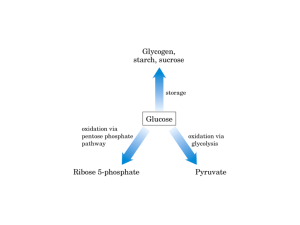
HMP SHUNT [Hexose Monophosphate Pathway] / PPP [Pentose Phosphate Pathway] • Principle pathway for oxidation of Glucose-Glycolysis & TCA • HMP-alternative pathway for oxidation of Glucose-not for Energy • Occours in cytosol • Provides: NADPH [reductive synthesis] & Pentoses [for NA synth] • Most common at the site of synthesis: Liver [phospholipid, FA synth, Cholesterol], adipose tissue [FA synth], lactating mammary gland [FA synth], adrenal cortex [Cholesterol, steroid hormone synth], testes & other endocrine glands concerned with steroid synthesis and RBC • NADPH produced: required for – Reductive biosynthesis of FA, TG, cholesterol, steroids [NADH – reduction in Catabolic pathways (NADH enters ETC→ ATP); NADPH – reduction in Synthetic pathways] 1 HMP Anabolic pathway that utilizes the 6 carbons of glucose to generate 5 carbon sugars and reducing equivalents 2 Oxidative reactions 1. • • • • Dehydrogenation of G-6-P by G6PD: Irreversible oxidation to 6-PGL- sp. coenzyme NADP+ 1st NADPH is produced HMP-primarily regulated at G6PD NADPH-comp inhibitor of G6PD 2. Hydrolysis of 6-PGL to 6-P-Gluconate by 6-PGL hydrolase or lactonase - irreversible 3. Oxidative decarboxylation of 6-P-Gluconate by 6-PGluconate dehydrogenase Irreversible 2nd NADPH is produced • • 3 Non-oxidative reactions • Interconversion of 3-, 4-, 5- and 7-Carbon Sugars • Ribulose 5-P to be converted to ribose 5-P [for Nucleic acid synthesis] • Or to intermediates of Glycolysis : F-6-P and Glycerladehyde-3-P • Non-oxidative part - controlled by availability of intermediates • Only coenzyme required: TPP for Transketolase reaction 4 Products of HMP Shunt G6P NADPH Biosynthesis (fatty acids, steroid hormones) Ribose 5-P Nucleic acid synthesis (DNA, RNA) 6G-6-P→ 5G-6-P regenerated, 6 CO2 eliminated,12 NADPH generated, 1 Glucose is completely oxidized 5 Uses of NADPH 1. Reductive biosynthesis: NADPH is a high energy molecule and electron donor. It is required as a source of electrons for biosynthesis of FA, cholesterol, sterols, hormones, and bile salts. 2. Reduction of H2O2: ROS- damage DNA, proteins, unsaturated lipids– reperfusion injuries, cancer, inflammatory diseases, aging. Several protective mechanisms: Enzymes that catalyze Antioxidant reactions: Glutathione peroxidase or GOD [ using reduced Glutathione or GSH which is active as antioxidant, present in most cells which can detoxify H2O2 ] Glutathione reductase or GR [regenerates GSH from oxidized glutathione formed in above reaction] using NADPH as a source of electrons Antioxidant chemicals: Vit E, A, C, uric acid, bilirubin, ceruloplasmin etc a. b. 6 3. CYP 450 or Cyt P-450: major pathway for hydroxylation of xenobiotics Supply of NADPH is critical for liver microsomal cyt P-450 4. Phagocytosis of microorganisms esp bacteria, foreign particles etc by Neutrophils & Macrophages: imp defense mechanism Oxygen dependent system- MPO [myeloperoxidase system]most potent, NADPH OXIDASE [needs NADPH] in WBC cell memb, converts O2 into Superoxide FR [Respiratory burst]→Superoxide is converted by SOD [superoxid dismutase] into H2O2 →lysosomal MPO converts it to hypochlorous acid HOCl·→ kills bacteria a. NADPH OXIDASE deficiency- Chronic granulomatosis b. Oxygen independent system- pH changes in phagolysosomes and lysosomal enzymes- destroy pathogens 7 G6PD and NADPH in the RBC Glucose Oxidant Stress Certain Drugs Infections Fava Beans Glucose Erythrocyte G6P 2 ADP G6P Glucose 6-phosphate dehydrogenase Glycolytic pathway 6-Phospho2 ATP 2 Lactate gluconate HMP NADPH + H+ H2 O2 2 GSH NADP Glutathione reductase Glutathione peroxidase GS-SG G6PD deficiency prevents the production of NADPH in the erythrocyte. Lack of NADPH results in hemolysis. 2 H2 O 8 G-6-PD deficiency • Inherited disease-most common disease producing enzyme abnormality in humans- X-linked • Hemolytic anemia due to inability to detoxify oxidizing agent • 400 different types of mutations [point mutations] • Shortened life span due to complications • Increased resistance to falciparum malaria in female carriers of mutation • ↓activity of G6-PD→↓NADPH [HMP] →↓detoxification of FR & peroxides • RBC- most vulnerable as HMP is only means for NADPH production. (other tissues NADP-dependent malate dehydrogenase also] • Precipitating factors- Oxidant drugs[ A-antibiotics (sulfamethoxazole), A-antimalarial (primaquin),A-antipyritics (acetanilid), ingest Fava beans [favism], severe infection-free radical generation in macrophages diffuse to RBC-hemolysis 9 Regulatory Mechanisms Enzymes G6PD and 6PGD catalyze irreversible steps of the HMP shunt. [NADPH] inhibits these enzymes via feedback inhibition [ATP]: a putative inhibitor of these steps [G-6P] increases flux through the HMP shunt (G-6P is a substrate) 10 TPP is coenzyme for Transketolase Transketolase reaction is measured in RBC as index of Thiamine status. Wernicke-Korsakoff syndrome: seen in alcoholics and persons with Thiamine deficiency is due to genetic defect in the enzyme Transketolase 11 Uronic acid Pathway of Glucose Importance in humans: • Provides UDP-glucuronic acid for conjugation [conjugation of bilirubin, steroids etc] and synthesis of glycosaminoglycans. • In lower animals (not in primates- deficiency of enzyme Lgulonolactone oxidase), this pathway leads to synthesis of Vit C. • Essential Pentosuria: one of Garrod’s tetrad [alkaptonuria, albinism, pentosuria, cystinuria- inborn error of metabolism]: *1 in 2500 births due to deficiency of xylitol dehydrogenase → L-xylulose excreted in urine gives + benedict’s test-not harmful. *Diffentiated from DM by + Bials test [orcinol in HCL-Bial’s reagent] by pentose sugars. 12 URONIC ACID PATHWAY G-6-P Phosphoglucomutase G-1-P + UTP [UDPG Phosphorylase] UDP- Glucose enters Uronic acid pathway 13 Aldose reductase- Glucose to Sorbitol [glucitol]: Lens, retina, Schwann cell of peripheral nerves, kidney, placenta, RBC, cells of ovaries and seminal vesicles. Sorbitol dehydrogenase- Sorbitol to Fructose Glucoe to Sorbitol to Fructose: in seminal vesicles for sperm cell [fructose is preferred carbohydrate energy source] Hyperglycemia: Uncontrolled DM-large amt Glucose enters Lens, Retina,Nerve, Kidney – with action of aldose reductase →↑Sorbitol, cannot pass through cell memb, so trapped inside cell. Sorbitol dehydrogenase is absent in Lens, retina, kidney and nerve cell →↑sorbitol accumulates →Osmotic effects →cell swelling and water retention: cause of cataract formation, peripheral neuropathy, vascular problems leading to nephropathy and retinopathy 14