Androgen Insensitivity Syndrome
(AIS)
Alice Mann
Maureen O’Brien
Elizabeth Rueckert
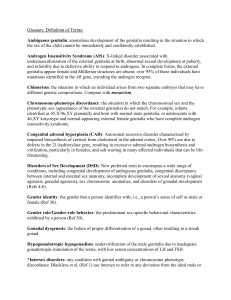
What is AIS?
A genetic condition where affected people have male chromosomes
and male gonads with complete or partial feminization of the external
genitals
An inherited X-linked recessive disease with a mutation in the
Androgen Receptor (AR) gene resulting in:
– Functioning Y sex chromosome
– Abnormality on X sex chromosome
Types
– CAIS (completely insensitive to AR gene)
• External female genitalia
• Lacking female internal organs
– PAIS (partially sensitive-varying degrees)
• External genitalia appearance on a spectrum (male to female)
– MAIS (mildly sensitive, rare)
• Impaired sperm development and/or impaired masculinization
Also called Testicular Feminization
Androgen Insensitivity Visuals
QuickTime™ and a
TIFF (LZW) decompressor
are needed to see this picture.
No. 2
No. 1
Image 1: A woman with an XY
chromosome pattern but insensitivity
to androgens
Image 2:A newborn genetic male
(46XY) with complete androgen
insensitivity syndrome and female
external genitalia
Classification of AIS Forms
Exists along continuum depending on degree of mutation in AR
gene (Quigley and French)
– Grade 1: PAIS
• Male genitals, infertile
– Grade 2: PAIS
• Male genitals but mildly ‘under-masculinized’
– Grade 3: PAIS
• Male genitals more severely ‘under-masculinized’
– Grade 4: PAIS
• Ambiguous genitals
– Grade 5: PAIS
• Essentially female genitalia, with enlarged clitoris
– Grade 6: PAIS
• Female genitalia with pubic/underarm hair
– Grade 7: CAIS
• Female genitalia with little to no pubic/underarm hair
History
Possibly first mentioned in the Talmud (400 BC)
Speculation of whether Joan of Arc (1412) and Queen Elizabeth I
(1533-1603) had AIS
First reported 1817
– Steglehner described apparently normal woman with
undescended testes
Dieffeneach (American geneticist) 1906
– Hereditary Pattern
Petterson and Bonnier 1937
– Concluded that affected persons are genetically male
Wilkins, 1957
– Found tissue unresponsiveness to androgens
Androgen receptor gene cloned and sequenced in 1988
Statistics
Affects 1 in 20,400 people
– 2/3 of cases inherited from mother
– 1/3 of cases come from a spontaneous mutation in the
egg
No effect on life expectancy
For a carrier woman, there is a 1 in 4 chance in each
pregnancy that the child will have AIS and a 1 in 2 chance if
the fetus is male
No racial differences
Normal Sexual Development
Sex Chromosome = XY
MALE
Gonads = Testes
External Genitalia = Male
FEMALE
Sex Chromosome = XX
Gonads = Ovaries
External Genitalia = Female
Normally chromosome sex determines gonad sex which determines
phenotypic sex
WHAT HAPPENS IN AIS?
Androgen Receptor Gene
AIS results from mutations in the androgen receptor gene, located
on the long arm of the X chromosome (Xq11-q12).
The AR gene provides instructions to make the protein called
androgen receptor, which allows cells to respond to androgens,
such as testosterone, and directs male sexual development.
Androgens also regulate hair growth and sex drive
Mutations include complete or partial gene deletions, point
mutations and small insertions or deletions.
QuickTime™ and a
TIFF (LZW) decompressor
are needed to see this picture.
The Process of Sexual Development
In AIS the chromosome sex and gonad sex do not agree with the
phenotypic sex
Phenotypic sex results from secretions of hormones from the
testicles
The two main hormones secreted from the testicles are
testosterone and mullerian duct inhibitor
– Testosterone is converted into dyhydrotestosterone
– Mullerian duct inhibitor suppresses the mullerian ducts and
prevents the development of internal female sex organs in
males
Wolffian ducts help develop the rest of the internal male
reproductive system and suppress the Mullerian ducts
– Defective androgen receptors cause the wolffian ducts and
genitals to be unable to respond to the androgens
testosterone and dihydrotestosterone.
AIS Fetus Development
•
Each fetus has non-specific genitalia for the first 8 weeks after
conception
• When a Y-bearing sperm fertilizes an egg an XY embryo is
produced and the male reproductive system begins to develop
• Normally the testes will develop first and the Mullerian ducts
will be suppressed and testosterone will be produced
• Due to the inefficient AR gene cells do not respond to
testosterone and female genitalia begin to form
The amount of external feminization depends on the severity of
the androgen receptor defect
• CAIS: complete female external genitalia
• PAIS: partial female external genitalia
• MAIS: Mild female external genitalia, essentially male
Testing for AIS
Tests
– During Pregnancy
• Chorionic Villus Sampling (9-12 weeks)
• Ultrasound and Amniocentesis (after 16 weeks)
– After Birth
• Presence of XY Chromosomes
– Buccal Mouth Smear
– Blood Test
• Pelvic Ultrasound
• Histological Examination of Testes
Biochemical Testing for Carriers
Tests
– 1960-70s: Skin biopsies-evaluate androgen binding
capacity
• Carries: 50% androgen binding
• Problem: some cases skipped because mutation did
not always take place in the binding region of the
gene
– 1990s: DNA Testing
• blood or mouth cavity smears
– Now:
• Measure length of base pair repeat region in first
exon of gene and compare it to a female relative’s
repeat region to determine if they are a carrier
Non-Biochemical Testing
Maternal relatives affected by AIS
In an XX female
– Delayed puberty
– Reduced pubic-auxiliary hair
– Asymmetric pubic-auxiliary hair
– Reduced bone density
Treatments
Surgery
– Orchidectomy or gonadectomy
• Removal of the testes
– Vaginal lengthening
– Genital plastic surgery
• Reconstructive surgery on the female genitalia if
masculinization occurs
• Phalloplasty
• Vaginoplasty
– Pressure dilation
• Clitorectomy
Debate
– What age?
– Who decides?
Treatments
Hormone Replacement Therapy (HRT)
– Types
• Female: Estrogen
– Progesterone (sometimes take to reduce risk of breast
or uterine cancer)
– postorchidectomy
• Male: Testosterone and DHT
– Form
• Oral, transdermal, implant, injection, vaginally
– Prevents osteoporosis (age 10 or 11)
• Body responds as if it is post-menopausal, thus
body density decreases and osteoporosis occurs
Psychological Issues
Medical Care Services (geneticist and a pediatric
endocrinologist)
– Criticisms
• Lack of emotional and psychological support
Family
– When to tell their children about their disorder
– Knowledge of if they are a carrier and if so guidance on
whether they should have children or not
Patients
– Therapy
• Isolation
• Registration desk of a doctor’s office
• Group examination
– Androgen Insensitivity Syndrome Support Group (AISSG)
Case Study
Discovery at age
– 12 years old
– 18 years old
Fears
Support
Bibliography
http://www.geneclinics.org
http://www.medhelp.org
http://web.nexis.com
http://www.androgendb.mcgill.ca/intro.htm