VISUAL_SYSTEM_2
advertisement
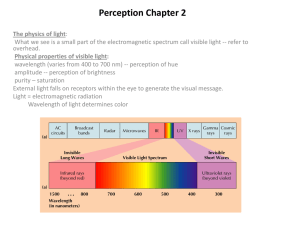
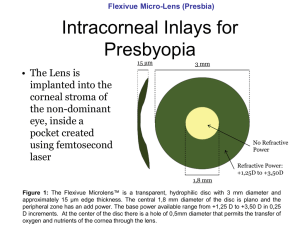
Visual System Lecture Outline • Structures of the Eye • Refraction and Image Formation • Visual Acuity • Autonomic Control of Pupil Diameter • Clinical Correlations • Dr W Kolbinger, Visual System (2009) 1 Anatomic Considerations The Ocular Fundus Fovea Optic disc Macula The optic disc region itself only contains axons of retinal ganglion cells, the output elements of the retina, but it lacks photoreceptors. As a consequence, the optic disc is responsible for the blind spot, a region inside the boundaries of the visual field, where we don’t receive visual information. 3 Optics of the Eye Convex Lens Focuses Light Rays Concave Lens Diverges Light Rays Measurement of the Refractive Power of a Lens—“Diopter” The refractive power in diopters of a convex lens is equal to 1 meter divided by its focal length. Optics of the Eye Cornea refractive power: 42 D Flat lens refractive power: 13 D Rounded lens refractive power: 26 D Plasticity: 13 D 5 Accommodation • Far Vision Ciliary muscle relaxed Suspensory ligaments tightened Flat lens refractive power: 13 D Focus on the Retina Accommodation Adjusts the Refractive Power of the Eye 6 Accommodation • Near Vision Ciliary muscle constricted Suspensory ligaments floppy Rounded lens refractive power: 26 D Focus on the Retina 7 Presbyopia • Near Vision Flat lens The variability of the refractive power of the lens between far vision (13 D) and near vision (26 D) is called refractive plasticity. Unfortunately, the lens looses its elasticity during aging, thereby reducing the ability to focus on near objects, a condition called presbyopia. Blurred picture on the Retina 8 Emmetropia (Normal Vision). Cataracts “Cataracts” are an especially common eye abnormality that occurs mainly in older people. A cataract is a cloudy or opaque area or areas in the lens What is Visual Acuity? Visual acuity is the ability to distinguish between two nearby points. Visual acuity is high when the two-point discrimination threshold is low (high spatial resolution). • Two point discrimination of the visual system • Normal: an angle of 5 minutes of a degree • highly dependent on the densities of retinal photoreceptors visual acuity also depends on a proper function of the optical apparatus of the eye, including accommodation. When the optical apparatus fails to produce a focused (sharp) picture on the retina, the objects in the visual field appear “blurry”. 5‘ Far vision Near vision 10 Neurological Examination of Visual Acuity • Eye charts and near cards Patient 20 800 Normal Distance equivalents 20 20 11 RETINAReceptor and Neural Function of the Retina • • • • Dr W Kolbinger, The Retina (2009) Photoreceptors and Phototransduction Color Vision Processing of Visual Information Clinical Correlations 13 Layers of the Retina Photoreceptor layer Photoreceptors rhodopsin Disks Outer segment -Visual pigment Nucleus Synaptic ending Rods are highly sensitive to light and enable us to see under low intensity light conditions (at night). Inner segment Synapses with bipolar and horizontal cells Rod Cones(3) are less sensitive to light. enable us to see colors. glutamate Cone 15 •Convergence is high in the rod system. It is low in the cone system. As a consequence, spatial resolution (visual acuity) is better in bright light, when the cone system is active. •Rods and cones are not evenly distributed over the whole retina and the fovea only contains cones, but no rods. As a consequence, there is no central vision under dim light conditions • Night Blindness The Visual Pigment Rhodopsin is the visual pigment of rods. It consists of two components: · Opsin, a protein which is synthesized in the photoreceptor (cones have different types of opsins). · Retinal, a chromophore, is the light absorbing compound or the visual pigment. It is derived from Vitamin A and is the chromophore of the visual pigment in rods and cones. Vitamin A is synthesized from beta-carotene contained in our food. Photoreception -The Dark Current GDP cGMP Na+ , G protein (Transducin) Visual pigment-Rhodopsin Dr W Kolbinger, The Retina (2009) cGMP-gated channel cGMP phosphodiesterase 18 Phototransduction GTP cGMP Na+ 5’GMP cGMP phosphodiesterase Dr W Kolbinger, The Retina (2009) 19 Color Vision Is Based on Comparison of Activity of Three Cone Types Visible Light Is Part of the Electromagnetic Spectrum The visible part of the spectrum is characterized by wavelengths ranging from 400 to 700 nm (nanometers). 20 Monochromatic Light: Colors of a Rainbow Dr W Kolbinger, The Retina (2009) 21 Three Types of Cones Have Different Spectral Sensitivities The human retina contains three types of cones: · S (short wavelength sensitive) cones, also called “blue” cones, with a maximum sensitivity at 430 nm · M (medium wavelength sensitive) cones, also called “green” cones, with a maximum sensitivity of 530 nm · L (long wavelength sensitive) cones, also called “red” cones, with a maximum sensitivity of 560 nm. Log relative sensitivity Stimulation of Cones by Monochromatic Light 450 nm monochromatic light 400 500 600 700 Wavelength (nm) 23 Stimulation of Cones by Monochromatic Light Log relative sensitivity 600 nm monochromatic light 400 500 600 700 Wavelength (nm) 24 Red-Green Color Blindness Protanopia Normal Individuals affected by red-green color blindness can no longer distinguish certain red colors from certain green colors. Deuteranopia 25 pseudo-isochromatic color plates like the one on the right are presented to the patient. The numbers embedded in the pattern of colored dots can be distinguished by individuals with a fully intact color vision. Dichromats, who are weak in red-green discrimination, have difficulties in identifying the numbers on all plates Visual Pathways Lecture Outline • • • • • The Visual Field Passage of Light Neuronal Pathways The Primary Visual Cortex Parallel Pathways for Depth, Motion, Form and Color • Clinical Correlations 27 The Visual Field Total amount of space we can see with this eye, when the eye is fixed straight ahead, pointing towards the center of the visual field (point of fixation). The extension of the visual field is measured in degrees of maximum deviation from this straight line in all directions. For right eye- left visual hemifield/nasal - right visual hemifield/temporal The vertical axis together with the horizontal axis divide the visual field into Four quadrants:superior left, superior right, inferior left and inferior right quadrant of the visual field. Projections of the Visual Field on the Retina The four quadrants of the visual field are projected onto the retina. The superior half of the visual field is projected to the inferior half of the retina, and vice versa. The left half of the visual field is projected on the right half of the retina, and vice versa. The nasal visual hemifield of the right eye temporal hemiretina of the right eye. temporal visual hemifield of the right eye nasal hemiretina of the right eye visual field defects e.g “bitemporal hemianopia`` 29 Chief Complaint: Headache and Nausea History: A 76 year old retired college dean presents with recurrent headaches over the past four years. Her headaches have significantly increased in duration and intensity over the past few months. She also reports episodes of nausea and vomiting. Her husband adds that she has recently developed difficulties with comprehending spoken language. The patient experiences uncoordinated movements of the right hand. She stopped drinking and smoking cigarettes during her first pregnancy, when she was 27. General Examination: 76 year old female in no acute distress. No significant cardiac, respiratory, or abdominal abnormalities. Vital signs unremarkable. Neurological Examination: The patient can speak fluently, but the content is frequently incomprehensible to the listener. Her ability to read and write is markedly reduced (dyslexia and dysgraphia respectively.) The patient can not identify a hairbrush, but was able to demonstrate its use. Numbness was detected in the right lower face and right hand. In addition, the examination of the right hand revealed impaired 2-pt discrimination, joint position, and fine touch. Motor examination and reflex testing of the lower extremities were unremarkable. Marked weakness of right arm flexion and extension was present, as well as elevated right biceps and brachioradialis reflexes. Brodmann’s Areas - Left Hemisphere. Neuronal Pathways, From the Retina Onwards relay station between the retina and the primary visual cortex. circadian clock afferent limb of the pupillary light reflex contribute to eye movements The Primary Visual Cortex V1 Occipital pole Area 17 34 The Primary Visual Cortex V1 Parieto-occipital sulcus Calcarine sulcus Area 17 35 Neuronal Pathways, From the Retina Onwards • Fibers originating in nasal hemiretina cross over at the optic chiasm, fibers originating in the temporal hemiretina don’t. • LGN fibers carrying sensory information of the superior half of the visual field follow the temporal radiation pathway, fibers originating in the inferior half of the visual field follow the parietal radiation pathway. Example1- the axons originating in the right LGN which are carrying sensory information from the superior left quadrant of the visual field, use the temporal radiation and synapse in the inferior portion (below the calcarine sulcus) of the primary visual cortex (V1). Example 2 - ? Retinotopic Organization of V1 Visual field left eye Visual field right eye Left hemisphere Right hemisphere 37 Neurological Examination of the Visual Fields The visual pathways are commonly tested in neurological examinations and they have high localizing value. Loss of vision is clinically tested in each quadrant of the visual field in a “confrontation visual field test”. In this test, each eye is tested separately by having the patient look straight at the examiners eye, while standing in double arms length distance. While the examiner occludes his left eye with one hand, the patient occludes his right eye (and vice versa). Then the examiner moves his other hand, with one (or more) of his fingers stretched out, gradually from the periphery to the center of the visual field, to determine where it is first seen. Assuming the examiner has normal vision, the patient should see the appearance of the hand at the same time as the examiner. He should also be able to tell the number of fingers stretched. Sparing of the Macula When the macula is not included, Macular sparing is often associated with vascular lesions involving the posterior cerebral artery or its branches,blood supply of the occipital pole of the cerebbral cortex (the area representing macular vision) may stay intact, due to sufficient blood flow from the middle cerebral artery. Eye Movements Lecture Outline • Types of Eye Movements • Extraocular Muscles, their Innervation and Control • Saccadic Eye Movements • Clinical Correlations 40 Types of Eye Movements • Conjugate Eye Movements • Saccadic eye movements (and gaze) • Vestibulo-ocular reflex • Optokinetic reflex (and smooth pursuit) • Non-Conjugate Eye Movements • Vergence (convergence and divergence) 41 Isolating Extraocular Muscle Function 42 Neurological Examination of Eye Movements Extraocular movements are examined using the “H-test”. Cranial Nerve Nuclei and Control Units in the Brainstem Midbrain CN III CN IV nucleus of MLF-control of vertical eye movements III III IV IV Cerebellum CN VI Pons VI VI pontine paramedian reticular formation (PPRF)/ horizontal gaze center. vestibulo-cerebellum (flocculo-nodular lobe)-optokinetic eye movements Medulla 44 Cortical Control Units Frontal eye field (Area 8) planning and initiation of eye movementssaccadic eye movements Parieto-occipital eye field dorsal (parietal) pathway for motion (and depth) led up exactly into this area.-optokinetic movements and smooth pursuit 45 Saccadic Eye Movements to the Right Frontal eye field Right Left PPRF Left MLF 46 Diplopia Visual field of the left eye Visual field of the right eye Fovea Fovea 47 Internuclear Ophthalmoplegia Internuclear ophthalmoplegia is based on a lesion of the medial longitudinal fasciculus (MLF), which prevents adduction of the eye on the side of the lesion during attempted lateral gaze. In the example on the right shows a patient with a lesion of the left MLF (adduction of the left eye is impaired). Convergence does not involve the MLF and is not affected by the lesion. EXAMPLE- Multiple Sclerosis. Internuclear Ophthalmoplegia Prevents adduction of the right eye X MLF lesion on the right Right Left 49 Chief Complaint: Nausea and Vomiting History: An 8 year old boy visited his pediatrician, and his mother reported that he was in good health until about two weeks ago. He describes that his initial symptoms include a mild bifrontal headache, which has become progressively worse. During the last few days, he developed nausea and bouts of occasional projectile vomiting accompanying the headaches. Furthermore, he recently noticed that he has tremendous difficulty when walking down the stairs from his bedroom to the kitchen and reported difficulties in sleeping. No family history of abnormal development or mental retardation exists. He has two perfectly healthy younger brothers. General Examination: This 8 year boy presents with pronounced pubic hair growth, a low pitched voice, enlarged genitalia, and acne on his forehead. Cardiac and respiratory examinations were unremarkable. Neurological Examination: Patient is alert and oriented x 3. No receptive or expressive aphasias were noted. Pupillary light reflex was intact bilaterally. Both the left and right optic discs appeared more pale than normal. Downward gaze (while the eyes were adducted) was impaired bilaterally. MLF lesion + PPRF lesion = 1 ½ Syndrome Prevents adduction of the right eye X X PPRF lesion on the right Right Prevents conjugate gaze of both eyes to the right X MLF lesion on the right Left 51 The Basics of Hair Cell Morphology Endolymph: High in Potassium Apex of Hair Cell with Cilia Base of Hair Cell with Synapse on Afferent Fiber 52 Cells of the Retina Photoreceptor Horizontal cell Bipolar cell Amacrine cell Ganglion cell 53 Some Bipolar Cells are Activated by Light, Others by Darkness There are two basic types of retinal bipolar cells. Some bipolar cells are activated (depolarized) when the light is ON. They are therefore called ON bipolar cells. Other bipolar cells are activated (depolarized) during darkness, when the light is OFF. They are therefore called OFF bipolar cells. Light Depolarizes ON Center Bipolar Cells Signconverting synapse: metabotropic glutamate receptor Photoreceptor hyperpolarizes during light ON On Center Bipolar Cell depolarizes during light ON 54 Parallel Pathways Specialized for Visual Information of Depth, Motion, Form and Color Dorsal (parietal) pathway Depth Motion LGN Where? Magno Parvo Ventral (inferior temporal) pathway What? Form Color 55 Light Hyperpolarizes OFF Center Bipolar Cells Signconserving synapse: ionotropic glutamate receptor Photoreceptor hyperpolarizes during light ON OFF Center Bipolar Cell hyperpolarizes during light ON 56