Vaksin dan sera
advertisement
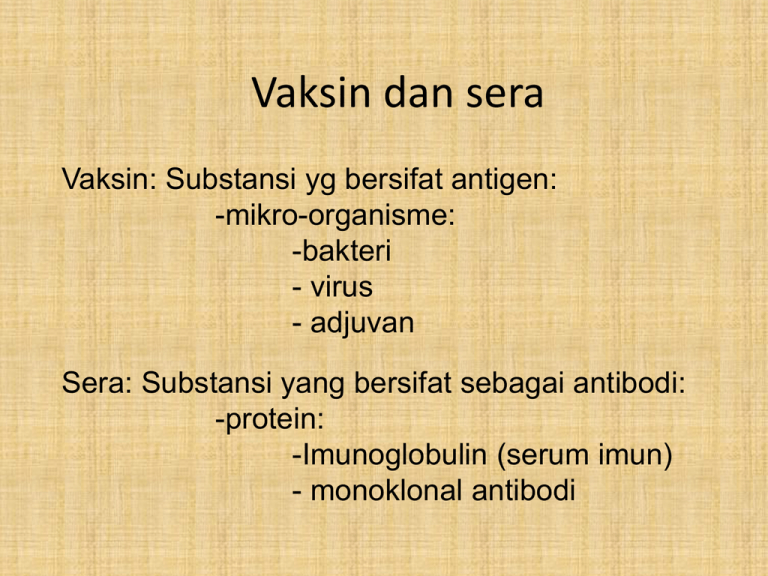
Vaksin dan sera Vaksin: Substansi yg bersifat antigen: -mikro-organisme: -bakteri - virus - adjuvan Sera: Substansi yang bersifat sebagai antibodi: -protein: -Imunoglobulin (serum imun) - monoklonal antibodi Vaksin -Vaksin dalah substansi biologik yg dapat meningkatkan sistem imun untk penyakit tertentu -Vaksin mengandung sejumlah kecil agen yg menyerupai mikroorganisme tertentu - Agen akan menstimulir sistem imun tubuh untk mengenal agen asing tersebut , membunuhnya , dan mengingatnya, - Sehingga bila ada agen yg sama tersebut masuk kedalam tubuh dengan mudah akan dibunuhnya Fungsi vaksin • Sebagai profilaktik • Mencegah serangan infeksi mikroba patogen • Sebagai therapeutik • Untuk pengobatan penyakit kanker Syarat vaksin yang baik 1. Mampu meningkatkan respon imun terhadap penyakit tertentu (TB-CMI; bakteriIg) 2. Mempunyai daya proteksi yg lama – Idealnya masa hidupnya lama 3. Aman – Tdk menimbulkan penyakit 4. Stabil – Tdk berubah dlm penyimpanan seblm diberikan 5. Relative murah Mekanisme A. Vaccines contain antigens (weakened or dead viruses, bacteria, and fungi that cause disease and infection) B. B cells to produce antibodies, with assistance from T-cells D. macrophages engulf them, process the information contained in the antigens, C. and send it to the T-cells so that an immune system response can be mobilized Jenis vaksin yg telah diproduksi • • • • • • • • • • Hepatitis B virus Hepatitis A virus Influenza Measles Mumps Polio Rubella Rabies Yellow Fever Varicella Zoster Develop vaccines against infectious diseases such as tuberculosis, malaria, AIDS and rotavirus. Jenis vaksin Vaksin Vaksin hidup/live vaccine Live attenuated organisms Heterologous vaccines Live recombinant vaccines Vaksin mati/killed vaccine Subcellular fractions Recombinant proteins Vaksin hidup • Attenuated organisms – Organisme dilemahkan (kurang virulen) dengan cara invitro mis.dg. perlakuan pemanasan (mutans), dengan bahan kimia – Org. Selektif mutans dlm tubuh bereplikasi lambat dan tidak virulen, tdk menimbulkan gejala klinis – Menimbulkan respons imun Vaksin hidup • Heterologous vaccines – Organisme yang mirip dengan target vaksin tetapi kurang virulen, yg dpt berbagi antigen dengan organisme virulen – Strain vaksin tersebut bereplikasi dalam tubuh penerima dan menstumir terbentuknya respon Ab, bereaksi silang dengan organisme virulen (target) – Misalnya: virus cowpox dan vaccinia- mirip virus variola Agen penyakit smallpox Vaksin rekombinan -Menggunakan rekayasa genetika: -Gen yg telah terkode sebg imunogenik protein dari suatu organisme disisipkan kedalam genome organisme lain (mis virus vaccinia) -Organime tersebut mengekspresikan gen yg baru gen baru tersebut dinamakan rekombinan - Bila diinjeksikan pada individu akan bereplikasi dan mengekspresikan sejumlah protein asing yg cukup utk menginduse respon imun spesifik dr protein tersebut Vaksin rekombinan Vaksin mati/killed vaccine Organisme patogen di inaktivkan dengan cara: - Pemanasan - bahan kimia: beta-propiolactone or formaldehyde These vaccines are not infectious and are therefore relatively safe. Subcellular fractions: - Protektive imun biasanya terjadi langsung dari satu atau dua jenis protein dari organisme patogen -Memungkinkan utk menggunakan protein murni dari org yg dimurnikan utk digunakan sebagai vaksin prosedur: MO dibiakkan dan kemudian di inaktivkan Protein yg diinginkan dimurnikan dan dikonsetratkan dr suspensi kultur. Prosedur (vaksin virus polio) Step 3 Step 2 Step 1 Use the tissue culture to grow new viruses. Done The polio vaccine is complete. Use formaldehyde to kill the viruses. Use the purifier to isolate the polio viruses. Step 4 Fill the syringe with the killed Prosedur (vaksin tetanus toxin) Step 1 Use the growth medium to grow new copies of the Clostridium tetani bacteria Done The tetanus vaccine is complete. Step 2 Isolate the toxins with the purifier. Step 3 Add aluminum salts to the purified toxins. Step 4 Fill the syringe with the treated toxins. Vaksin protein rekombinan (killed vaksin) -Immunogenic proteins of virulent organisms may be synthesized artificially by introducing the gene coding for the protein into an expression vector, such as Ecoli or yeasts. The protein of interest can be extracted from lysates of the expression vector, then concentrated and purified for use as a vaccine. The only example of such a vaccine, in current use, is the hepatitis B vaccine. Prosedure protein rekombinan (vaksin HiB) Step 2 Add the segment of DNA to the DNA of a yeast cell (which is in the yeast culture Step 1 Use the tweezers to pull out a segment of DNA from the hepatitis B virus. Done The hepatitis B vaccine is complete. Step 3 Use the purifier to isolate the hepatitis B antigen produced by the yeast cells. Step 4 Fill the syringe with the purified hepatitis B antigen. Attributes - Killed vaccines 1.Immune response •poor; only antibody - no cell immediated immune response. •response is short-lived and multiple doses are needed. •may be enhanced by the incorporation of adjuvants into the vaccine preparation 2. Safety •Inactivated, therefore cannot replicate in the host and cause disease. •Local reactions at the site of injection may occur. 3. Stability •Efficacy of the vaccine does not rely on the viability of the organisms. •These vaccines tend to be able to withstand more adverse storage conditions. 4. Expense •Expensive to prepare. Adjuvants Certain substances, when administered simultaneously with a specific antigen, will enhance the immune response to that antigen. Such compounds are routinely included in inactivated or purified antigen vaccines. Adjuvants in common use: 1. Aluminium salts -First safe and effective compound to be used in human vaccines. -It promotes a good antibody response, but poor cell mediated immunity. 2. Liposomes and Immunostimulating complexes (ISCOMS) 3. Complete Freunds adjuvant is an emulsion of Mycobacteria, oil and water ; -Too toxic for man -Induces a good cell mediated immune response. 4. Incomplete Freund's adjuvant as above, but without Mycobacteria. 5. Muramyl di-peptide Derived from Mycobacterial cell wall. 6. Cytokines IL-2, IL-12 and Interferon-gamma. DNA Vaccines DNA vaccines are at present experimental, but hold promise for future therapy since they will evoke both humoral and cellmediated immunity, without the dangers associated with live virus vaccines. The gene for an antigenic determinant of a pathogenic organism is inserted into a plasmid. This genetically engineered plasmid comprises the DNA vaccine which is then injected into the host. Within the host cells, the foreign gene can be expressed (transcribed and translated) from the plasmid DNA, and if sufficient amounts of the foreign protein are produced, they will elicit an immune response. Sera (antibody) The advantages of antibody-based therapies include versatility, low toxicity, pathogen specificity, enhancement of immune function, and favorable pharmacokinetics; The disadvantages include high cost, limited usefulness against mixed infections, and the need for early and precise microbiologic diagnosis. The potential of antibodies as anti-infective agents has not been fully tapped. Antibody-based therapies constitute a potentially useful option against newly emergent pathogens. Serum therapy, human MAbs, and antimicrobial chemotherapy Antibody therapy Chemotherapy Immune serum Human MAb Specificity Narrow Narrow Broad Source Animals Humans Tissue culture Bioreactor Fermentation Fermentation Chemical synthesis Toxicity High Low Low Cost High High Low Administration Difficult Easy Easy Pharmacokinetics Variable Consistent Consistent Antimicrobial Immune enhancement Toxin neutralization Antimicrobial Immune enhancement Toxin neutralization Mechanism of action Antimicrobial