and carbapenemase‐producing Enterobacteriaceae during
advertisement
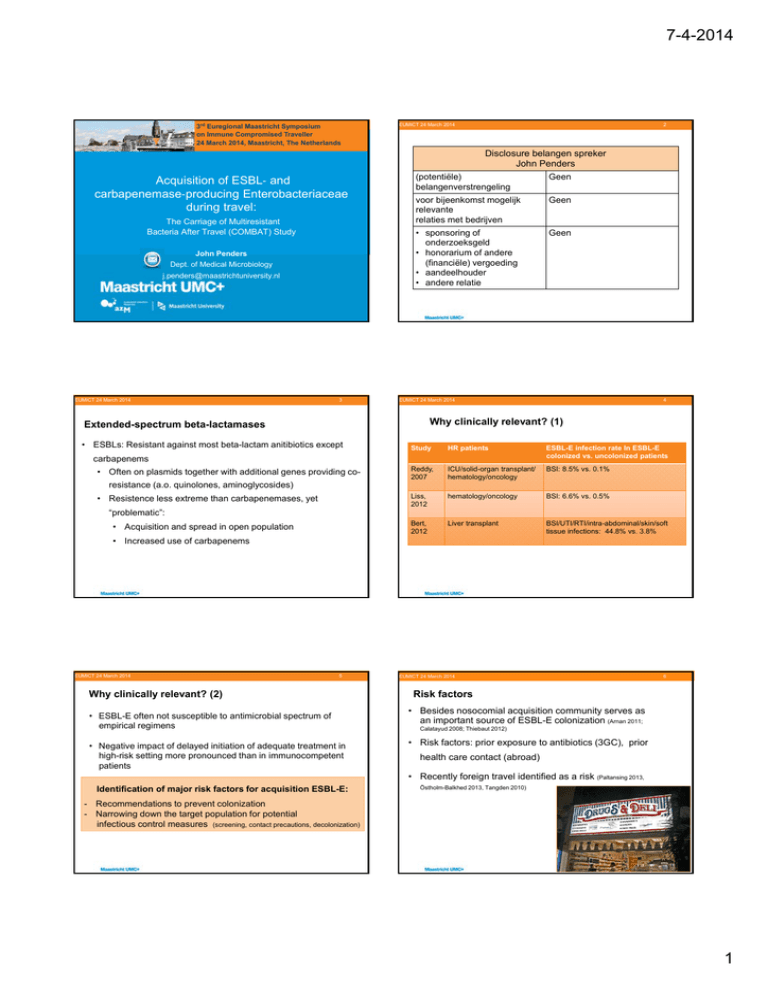
7-4-2014 3rd Euregional Maastricht Symposium on Immune Compromised Traveller 24 March 2014, Maastricht, The Netherlands Acquisition of ESBL‐ and carbapenemase‐producing Enterobacteriaceae during travel: The Carriage of Multiresistant Bacteria After Travel (COMBAT) Study John Penders Dept. of Medical Microbiology j.penders@maastrichtuniversity.nl EUMICT 24 March 2014 3 EUMICT 24 March 2014 2 Disclosure belangen spreker John Penders (potentiële) Geen belangenverstrengeling voor bijeenkomst mogelijk Geen relevante relaties met bedrijven • sponsoring of Geen onderzoeksgeld • honorarium of andere (financiële) vergoeding • aandeelhouder • andere relatie EUMICT 24 March 2014 4 Why clinically relevant? (1) Extended-spectrum beta-lactamases • ESBLs: Resistant against most beta-lactam anitibiotics except Study • carbapenems • Often on plasmids together with additional genes providing co- Reddy, 2007 HR patients ESBL-E infection rate Inthan ESBL-E Higher colonization rates in high-risk patients in colonized vs. uncolonized patients healthy individuals (Kader 2007, Ko 2013) ICU/solid-organ transplant/ hematology/oncology BSI: 8.5% vs. 0.1% resistance (a.o. quinolones, aminoglycosides) Liss,• 2012 • Resistence less extreme than carbapenemases, yet “problematic”: Bert, 2012 • Acquisition and spread in open population hematology/oncology BSI:shown 6.6% vs.to0.5% ESBL-E colonization has been increase the risk of a subsequent ESBL-E infection in high-risk patients - Impaired mucosal barrier in HR patients Liver transplant BSI/UTI/RTI/intra-abdominal/skin/soft tissue infections: 44.8% vs. 3.8% • Increased use of carbapenems EUMICT 24 March 2014 5 Why clinically relevant? (2) • ESBL-E often not susceptible to antimicrobial spectrum of empirical regimens • Negative impact of delayed initiation of adequate treatment in high-risk setting more pronounced than in immunocompetent patients EUMICT 24 March 2014 6 Risk factors • Besides nosocomial acquisition community serves as an important source of ESBL-E colonization (Arnan 2011; Calatayud 2008; Thiebaut 2012) • Risk factors: prior exposure to antibiotics (3GC), prior health care contact (abroad) • Recently foreign travel identified as a risk (Paltansing 2013, Identification of major risk factors for acquisition ESBL-E: Östholm-Balkhed 2013, Tangden 2010) - Recommendations to prevent colonization - Narrowing down the target population for potential infectious control measures (screening, contact precautions, decolonization) 1 7-4-2014 EUMICT 24 March 2014 7 COMBAT Study Carriage Of Multiresistant Bacteria After Travel Tropenpoli AMC Havenziekenhuis EASE Travel Clinic EUMICT 24 March 2014 8 Baseline data • Inclusion Nov. 2012-Nov. 2013 • 2001 travelers, 215 household members • Response rate: T1 97.8%, T2 96.6% 2,000 Travelers & 400 household members Pre-travel Objectives: • Incidence of colonization ESBL- and • Age: 50.4 (18.1-81.7), M/F: 45.9/54.1 Pre-travel colonization Q + swab Travel carbapenemase-producing Post-travel • 124 (6.2%) Travellers Q + swab Enterobacteriaceae 1 month Q + swab • 14 (6.4%) HH members 3 months Q + (swab) • 1884 Travellers “at risk” 6 months Q + (swab) 12 months Q + (swab) • Persistence of colonization • Transmission to household members • (Travel-associated) risic factors • Examining the resistome EUMICT 24 March 2014 9 EUMICT 24 March 2014 10 Main organisms and co-resistance ESBL-E acquisition according to UN subregions Escherichia coli Klebsiella pneumoniae Enterobacter cloacae Proteus vulgaris Citrobacter freundii Citrobacter braakii Proportion of resistant strains Proteus mirabilis EUMICT 24 March 2014 11 Carbapenemase-producing Enterobacteriaceae • 4/2000 “at risk” travelers acquired CP-E – Incidence rate 0.2% (95%CI 0.075-0.5%) Pretravel Posttravel 1 OXA-48 E. coli 2/Turkey & Greece EUMICT 24 March 2014 E. coli Klebsiella 12 Conclusions and discussion • 1 Traveler CP-E positive pre-travel (OXA-48 E. coli) 1 month 3 months 6 months OXA-48 E. coli OXA-48 E. coli NEG ……. ……. NEG OXA-48 Klebsiella NEG NEG ……. …….. 3/Indonesia NEG OXA-48 E. coli OXA-48 E. coli OXA-48 E. coli OXA-48 E. coli …….. 4/Indonesia NEG NEG NEG OXA-48 E. coli NEG …….. 5/Myanmar NEG NDM-1 E. coli NDM-1 E. coli NEG …… …… 6/SE Asia NEG NDM-1 E. coli NEG NEG …… ……. Subject/destinatio n 1 0,9 0,8 0,7 0,6 0,5 0,4 0,3 0,2 0,1 0 1 year • Very high ESBL-E acquisition rates in travelers to Asia & Northern Africa • Within subregions large variations between countries • Acquisition (and transmission?) of CP-E in travelers without health care contact • Travel- and traveler-associated risk factor analysis will provide further insight into (modifiable) risk factors • Infection control measures: prevention, screening, contact precautions? 2 7-4-2014 EUMICT 24 March 2014 13 EUMICT 24 March 2014 Thank you! Erasmus MC - Rotterdam Dr. Damian Melles Prof. dr. Henri Verbrugh Drs. Maris Arcilla ESBL-E colonization over time MUMC – Maastricht Dr. J. Penders Dr. Ellen Stobberingh 0,4 0,35 Colonization rate (%) COMBAT-study Team AMC - Amsterdam Prof. dr. Menno de Jong Dr. Constance Schultsz Dr. Bram Goorhuis Drs. Jarne van Hattem 14 UMC Utrecht Dr. Martin Bootsma Havenziekenhuis Rotterdam Dr. Perry van Genderen 0,3 0,25 Travelers 0,2 Household members 0,15 0,1 0,05 0 Pre-travel Post-travel 1 month post-travel ..and all employees of the Travel Clinics (Havenziekenhuis, Tropenpoli AMC, EASE Travel & Health Support)! EUMICT 24 March 2014 15 Chronic diseases Disease/condition Prevalence (%) Diabetes 2.7% Respiratory 4.3% CVD 4.4% GI 2.7% Hepatic/renal 0.4% Malignancy 0.9% Autoimmune disease 1.5% Immunosuppressive drug use 1.2% 3