PowerPoint slides - Johns Hopkins Medicine
advertisement

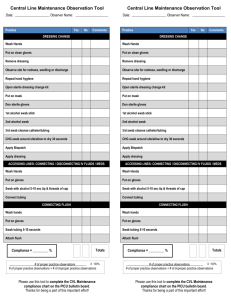
On the CUSP: STOP BSI Central Line Dressing Change © 2009 Terminology for Lines Included • Percutaneously placed central lines • Tunneled lines • Peripherally inserted central catheter • Vascular Access devices * May not include hemodialysis catheters. 2 © 2009 Who Completes • Nursing Personnel who have demonstrated competency for central line dressing changes, including PICC teams and Nurse practitioners. • Medical personnel who have demonstrated competency including physicians and physician assistants. 3 © 2009 Frequency • Once weekly if a transparent dressing is used • Every day if a gauze dressing is used while bleeding • Any time a dressing is no longer occlusive, damp or visibly soiled. 4 © 2009 Equipment Needed • Chlorhexidine Gluconate 2% w/ Isopropyl Alcohol 70% (1 Swab)* • Transparent dressing or gauze – * do not use if patient is sensitive Tincture of iodine or 70% isopropyl alcohol may be used. – *do not use chlorhexidine in patients <2 years old. • Sterile Gloves • Mask for person applying dressing • Cone mask for patient • Skin prep (appropriate size) • Tape if gauze dressing is used • Clean Gloves (appropriate size) 5 © 2009 Additional Supplies that May Be Needed • Sterile cotton tipped applicator (needed to cleanse insertion site) • Sterile cup to hold sterile saline • Sterile normal saline • Adhesive removal pads or alcohol wipes • Sterile 2x2 gauze 6 © 2009 Procedure: Preparation 1. Explain procedure to patient/family. 2. Wash your hands. 3. Don clean gloves and remove old dressing using alcohol swab or adhesive remover pads as needed. 4. Inspect insertion site of catheter for signs of infection. Culture if needed. Assess security of sutures. 5. Remove your gloves. 6. Open sterile gloves and create a sterile field using sterile glove package. Continued… © 2009 7 Procedure: Sterilization 7. Open Chlorhexidine Gluconate 2% with Isopropyl Alcohol 70% swab and drop onto sterile field. 8. Open transparent dressing and drop onto sterile field. 9. Open skin prep and place on outer edge of sterile field. 10. Don sterile gloves. Continued… 8 © 2009 Procedure: Cleansing the Site 11. Clean skin with Chlorhexidine Gluconate 2% with Isopropyl Alcohol 70% swab. 12. Using friction or scrubbing motion to apply. Begin directly at the insertion site as you move swab outward in a circular motion to cover all areas without retracing the area already cleansed. 13. Allow Chlorhexidine Gluconate 2% with Isopropyl Alcohol 70% swab to air dry completely.* *If using povidone iodine, allow to remain on the skin for at least 2 minutes, or longer until dry. 9 © 2009 Preparing to Place Dressing 14. Designate one hand to be the unsterile hand and pick up the skin prep packet. 15. Remove skin prep pad with sterile hand. 16. Apply skin prep on outer perimeter of skin where dressing edge will touch patient. *Do not put skin prep over the catheter insertion site or the immediate surrounding area. Allow to completely dry. *Do not apply organic solvents (e.g., acetone or ether) to the skin before insertion of catheters or during dressing changes. 10 © 2009 Placing the Dressing 17. Using your sterile hand, apply transparent dressing per manufacturer recommendations. 18. Label the dressing with date, time and initials to identify when changed. 19. Document the dressing change on the flow sheet per protocol if indicated. 11 © 2009 Other Options • Please see other infection prevention options under the infectious disease series for information on Chlorhexidine impregnated patches, antibiotic coated catheters etc. 12 © 2009 References • Johns Hopkins Hospital, Vascular Access Device Policy (Adult) http://safercare.s3.amazonaws.com/support_medi a/docs/clabsi/Appendix_H_Adult_VAD_Policy.pdf • MMWR Guidelines for the Prevention of Intravascular Catheter-Related Infections http://www.cdc.gov/mmwr/PDF/rr/rr5110.pdf 13 © 2009 On the CUSP: STOP BSI Central Line Maintenance 14 © 2009 Learning Objectives • Review the evidence and recommendations for central line maintenance 15 © 2009 Source of Recommendations • Centers for Disease Control • Society for Healthcare Epidemiology of America • Infectious Diseases Society of America 16 © 2009 Overview of Recommendations Central line maintenance recommendations address the following topics: • • • • • • • Central line insertion Central line dressing changes Replacement of IV administration sets Hang time for parenteral fluids Catheter hub cleansing Removal of unnecessary lines Education 17 © 2009 Central Line Insertion • Ensure use of checklist • Empower nurses to stop the procedure if the steps in the checklist are not followed • Leadership must create a culture that supports nurses 18 © 2009 Central Line Dressing Change Dressing change responsibility includes only those who have demonstrated competency: • Nursing personnel including PICC teams and nurse practitioners • Medical personnel including physicians and physician assistants 19 © 2009 Central Line Dressing Change Frequency: • Transparent dressing – Every 7 days – PRN if damp, loosened, or soiled • Gauze dressing – Every 48 hours for routine use 20 © 2009 Replacement of IV Administration Sets • Lipids and blood products (enhance bacterial growth) – Change every 24 hours • All other IV administration sets – No more frequently than every 72 hours – Not more than every 96 hours 21 © 2009 Hang Time for Parenteral Fluids • Lipid-containing parenteral nutrition – Change every 24 hours • All other IV fluids including nonlipid-containing parenteral nutrition – No formal recommendations – JHH changes nonlipid-containing IV fluids every 24 hours 22 © 2009 Catheter Hub Cleansing • Clean hub before accessing with Chlorhexidine or 70% alcohol • No formal recommendations regarding how long to cleanse hub 23 © 2009 Remove Unnecessary Lines • Assess need for continued central line access during daily multidisciplinary rounds – Add question to a Daily Goals worksheet – Complete every day during rounds 24 © 2009 Education Educate all necessary staff: • Guidelines to prevent catheter-related bloodstream infections • Use of central line checklist • Proper insertion and maintenance of central lines Ensure competency through yearly education and examination 25 © 2009 References • Marschall J, Mermel LA, Classen D, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals. Infection Control and Hospital Epidemiology. 2008; 29 (supp. 1):S22S30. • O’Grady NP, Alexander M, Dellinger P, et al. Guidelines for the prevention of intravascular catheter-related infections. Infection Control and Hospital Epidemiology. 2002; 23(12):759-769. 26 © 2009