TCP Supervision
advertisement

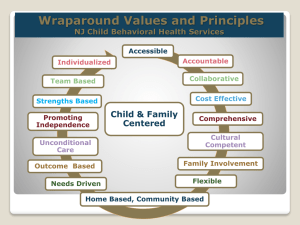
USING PERSON-CENTERED PLANNING AS A ROADMAP FOR CARE COORDINATION AND BETTER OUTCOMES IN AN INTEGRATED TREATMENT SETTING Diane Grieder, M.Ed AliPar, Inc. NYAPRS Conference September 2011 Learning Objectives Understanding how Person-Centered planning can be a bridge to providing coordinated/integrated care • Understanding what is meant by shared-decision making and how it can improve outcomes for people • Learn about the Mental Health Care Model (Wagner’s Chronic Care Model revisited) • So, what are we really talking about today? • Health Care Reform • Accountability (Accountable Care Organizations) • NYS Health Homes (for people with chronic conditions) • Patient/Person Centered Medical Home • Coordinated Care • Integrated Care • Better Outcomes for people • Better collaboration between providers Traveling the Transformation Highway Integration and Care Coordination SAMHSA Rationale for Integrated Care: •Behavioral Health is part of Health •Prevention Works •Treatment is Effective •People Recover • Pam Hyde, Director of SAMHSA What does a recovery oriented system of care look like? From: To: Illness Focused Recovery Focused “Compliance” valued “Choice” valued Deficit Focused Being known by what’s wrong Strength Focused Being known as an individual Shared decision making Professional “in charge” Active Participation Learned Helplessness “Silo of care” focused Institutional resources Planning is done for the person Broad bio-psychosocial focused Community resources/integration Planning is collaborative, recurring, and involves an ongoing commitment to the person © 2009 Coordinated Care Services, Inc. CMHS/SAMHSA 10 x 10 Plan: Pledge for Wellness (2007) We envision in which people with mental illnesses pursue optimal health, happiness, recovery and a full and satisfying life in the community via access to a range of effective services, supports and resources. We pledge to promote wellness for people with mental illnesses by taking action to prevent and reduce early mortality by 10 years over the next 10 year time period. Major Health Risks for MH Population Cardiovascular disease is primary culprit • Risk factors include: • Smoking • Physical inactivity • Medication side effects • Toxic effects of abused substances • Diet • Poor access to care: underuse of evidence-based medical services • Higher exposure to medical errors Druss, 2007 Causes of Health Disparities • Medications, especially the atypical antipsychotic drugs, effect on: • Weight gain • Dyslipidemia (unhealthy cholesterol profiles) • Glucose (sugar) metabolism • High rates of smoking • Lack of weight management/poor nutrition • Physical inactivity Causes of Health Disparities • Lack of access to & utilization of preventive community healthcare, including health promotion services/resources • Poverty • Social isolation • Separation of health & mental health systems at the federal, state, local level • Lack of coordinated infrastructure, policy, planning, quality improvement strategies, regulation or reimbursement Chronic Care Model Community Health System Health Care Organization Resources and Policies SelfManagement Support Informed, Activated Patient Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team Outcomes Improved Outcomes Mental Health Care Model Community Resources and Policies Social Inclusion and Opportunity Empowered, Hopeful Consumer Mental Health System Health Care Organization SelfManagement Support Productive Interactions Delivery Decision System Support Design Receptive, Capable Team Recovery / Wellness Outcomes Clinical Information Systems The Chronic Care Model • Model depends on individual having continuous, planned care • Part of the model includes care management: • To educate and support the individual in becoming a partner in healthcare decision making • To adopt self-management strategies for health promotion & living well with chronic disease • To access community resources AHRQ Definition of Patient Centered Medical Homes (PCMH) 5 functions and components: • Patient-Centered • Comprehensive Care • Coordinated Care • Superb Access to Care • A systems based approach to quality and safety Integrated MH/SA Services Goal: To improve the proficiency of both systems of care to identify and engage persons with co-occurring disorders •Screening/Assessment •Professional Development/Training •Program Models/Guidelines •System Coordination Care Coordination • One of the core functions of the PCMH – defined as: “The deliberate organization of patient care activities between 2 or more particiapnts involved in a patient’s care to facilitate the appropriate delivery of health care services” • Reducing Care Fragmentation…A Toolkit for Coordinating Care. California Healthcare Foundation Care Coordination vs. Case Management? •Care coordination is the facilitation of access to and coordination of medical and behavioral/social support services for persons across different providers and 0rganizations. •Case Management typically focuses on a medical model with an emphasis on the person’s mental health needs only. Key Recommendations for Integrated Healthcare: Consumer Recommendations • Assure there is no wrong door for receiving care • Establish Team Based Coordinated Care • Honor Consumer Choices • Incorporate services to facilitate receipt of physical healthcare • Educate providers and consumers • Create environment of respect and acceptance • Multnomah County MHASD Healthcare Integration Report 6/22/10 Bridging the two worlds Care Manager Functions • Develop and maintain rapport with individual and provider • Educate the individual and family • Monitor symptoms & communicate findings to provider • Develop and maintain a self-care action plan • Maximize adherence (interest) to the care plan (can be communiyt wide)through negotiation of solutions to treatment-emergent problems Cole & Davis (2004) A Solution… Hypothesis • Person-centered treatment plans are a key lever of personal and systems transformative change in creating health homes/providing care coordination Defining Person-Centered Practice • Person-Centered Practice is defined as working with consumers in an individualized and empowering way to assist them in their personal recovery journey. 23 Being Person-Centered in Practice • • • • The consumer as a whole person Sharing power and responsibility Having a therapeutic alliance The clinician as person 24 What is PCP? Taking a Closer Look • Person-centered planning is a collaborative process resulting in a recovery oriented treatment plan is directed by consumers and produced in partnership with care providers and natural supporters for treatment and recovery supports consumer preferences and a recovery orientation • Adams/Grieder The Recovery Plan • It is the “work/social contract”, created by the person and provider. Service Plan Functions • Identifies responsibilities of team members--including person served and family • Increases coordination and collaboration • Decreases fragmentation and duplication • Coordinates multidisciplinary/multi-agency interventions • Prompts analysis of available time and resources • Provides assurance / documentation of medical necessity • Anticipates frequency, intensity, duration of services • Promotes culturally competent services 27 CARF Behavioral Health Standards 2011 on Integrated Care • An individualized integrated plan regarding medical and behavioral health needs is developed with collaboration of: • The person served • All staff necessary to carry out the plan Guidance to meet this standard includes: The individualized plan is developed with the active involvement of the person served as well as the various disciplines needed to successfully implement the plan. The plan addresses and integrates, in a holistic manner, the medical and behavioral health needs of the person served Why Shared Decision Making in Health Care? The Problem • High rates of failure to engage, disengagement, and non-adherence • Less than 5% of people with severe mental illnesses receive most evidence-based services • Important reasons include lack of information, inattention to the person’s goals, failure to empower the person, and failure to provide effective services Finding Common Ground… • Research indicates that physicians still fail to find common ground with patients • Without agreement about what is wrong, it is difficult for a patient and doctor to agree on a treatment plan that is acceptable to both • Not essential that patient/doctor share the same perspective • doctor's explanation and recommended treatment must at least be consistent with the patient’s point of view and make sense in the patient’s world Shared Decision Making is at the Core of Ethical, Patient Centered Care Patient Centered Medical Home Accountable Care Organizations Meaningful Use of Health Information Technology (HIT) Supporting Principles Autonomy “The general trend has been to expand autonomy in health care decision making. [It] assumes the better informed an individual is, the better equipped he or she is to make health care decisions.” • Surgeon General’s Report on Mental Illness • 1999 – Chapter 7 Supporting Principles Transparency – Choice based on value “consumers deserve to know the quality and cost of their health care. Health care transparency provides consumers with the information necessary, and the incentive, to choose health care providers based on value. Providing reliable cost and quality information empowers consumer choice.” US Dept of Health & Human Services www.hhs.gov/transparency/ Supporting Principles Person-Centered Planning •Treatment planning (and documentation) beyond reimbursement and administrative goals •A roadmap for reaching individual goals Pushing the Agenda Shared Decision Making •As consensus building (not coercion) •As a motivator for both experts to change •As a systems change protocol Decision Support Systems Address these Problems through • A structured approach to : • defining one’s goals, • obtaining information on effective service options, • choosing services, • participating in developing treatment plans, • on-going assessment of one’s progress, and • reviewing treatment decisions Shared Decision Making Clinician and patient work together They share information About options and outcomes About preferences They work toward a consensus about the preferred test or treatment They reach an agreement on the test or treatment to implement (Charles C, Soc Sci Med 1997; 44:681) Decision-Making • Process of making a choice (decision) from among two or more discrete options (Wills & Holmes- Rovner, 2006) • Provider role as a consultant to support SDM (Adams & Drake, 2006) • Majority of mental health treatment decisions are preference-driven (personal values do/should significantly guide the decisionmaking) We Believe Patients Should Be Supported & encouraged to participate in their health care decisions Fully informed with accurate, unbiased & understandable information Respected by having their goals & concerns honored Benefits of SDM • Reduced decisional conflict • Greater knowledge • Improved satisfaction with the decision-making process • Improved ability to make choices (fewer people left undecided) • Improved concordance of decisions with personal values • More active involvement of consumers in decision-making • Improved communication between consumers and providers • Limited study of how preferences and decision-making processes impact choices made by consumers, including service engagement and intervention outcomes Outcomes of Shared Decision Making for Persons with Severe Mental Illnesses • Have been demonstrated in randomized trials to: • Increase knowledge and participation in planning • Enhance patient satisfaction with care • Reduce unmet needs • Improve adherence and quality of life • Decrease symptoms of depression and alcohol abuse • Practitioners • Increased insight into patient preferences • Improved efficiency of care • Some age and discipline related reluctance to participate Discussion • How do these functions relate to what you consider your role responsibilities (either as a provider or as a recipient of services) at this point in time? • What implications does this information have for clinicians/case managers/care coordinators/consumers in the future? • Diane Grieder, AliPar, Inc., www.alipar.org, 757-647-8716