Birth Related Stressors
advertisement

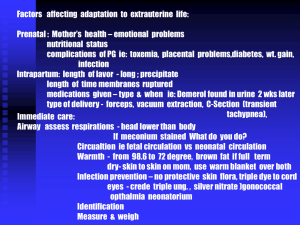
The Newborn at Risk: Birth Related Stressors Chapter 29 1) Newborn at Risk for Asphyxia 2) Care of the Newborn with Respiratory Distress 3) Transient Tachypnea of the Newborn (TTN) 4) Meconium Stained Amniotic Fluid 5) Newborn at Risk Cold Stress 6) Hypoglycemia 7a) Hyperbilirubinemia 7b) Hemolytic Disease of the Newborn 8) Newborn at Risk for Anemia 9) Newborn at Risk Polycythemia 10) Antibiotic Therapy 1 All InfantsNursing Care -A, B, C’s -NTE -Early detection/treatment of hypoglycemia -Support the family 2 • Nursing care • Should always include these • How do you maintain a NTE? • - cap on head • - radiant heat source • - keep infant dry • - warm objects prior to contact with infant • - positioning of the infant (flexed posture) • Early detection/treatment of hypoglycemia 3 1) Newborn at Risk for Asphyxia • Asphyxia is severe, prolonged hypoxia • Can occur during antepartum, intrapartum, or postpartum • Causes respiratory, circulatory, and biochemical changes 4 Risk Factors for Asphyxia • Before and during labor – Biophysical profile – Fetal heart rate – nonreassuring • Due to complications causing low O2 – – – – Low fetal scalp pH Meconium stained fluid Prematurity Multiple gestation 5 • Biophysical profile • - fetal breathing movement • - fetal movement of body/limbs • - fetal tone • - amniotic fluid volume • - reactive FHR with activity • FHR • - decreased variability • - normal FHR 110-160 baseline • - decelerations • Scalp pH • - 7.25 or > considered normal 6 Risk Factors for Asphyxia • At birth – – – – – – – Diffcult birth Low cord pH - acidosis APGAR Male SGA Sepsis Congenital heart/lung defects 7 03:05 Asphyxia • Newborn may be unable to make the transition to extrauterine circulation • Reverts to fetal circulatory patterns • pulmonary hypertension • increasing hypoxia • acidemia • Requires intensive supportive care to reverse 8 Newborn at Risk Asphyxia(R<60, start chest compressions) Nursing care • • • • Oxygen IV fluids May need newborn resuscitation (NRP) Relate appropriate information to parents 9 5:35 2) Care of the Newborn with Respiratory Distress • Respiratory Distress Syndrome – Prematurity – Surfactant deficiency disease – Transient Tachypnea of the Newborn • Meconium Aspiration Syndrome 10 6:05 11 • How would we know that the infant has high CO2, or is acidotic? • ABG or Capillary Blood Gas (CBG) • Normal PH = 7.30-7.40 after birth…. • Co2 arterial= 35-45 & capillary= 35-50 • Po2 on room air arterial = 50-80& capillary= 35-45 • Bicarbonate 19-22 arterial or capillary l • Sao2 per pulse ox probe >90 – What would be normal for a cord pH……? • Look it up! 12 Newborn at Risk Respiratory Distress • Respiratory distress syndrome (RDS) aka. Hyaline membrane disease (HMD) – ↓ surfactant – Hypoxia – Respiratory acidosis which can develop • Into Metabolic acidosis • RDS- indicates a failure to synthesize surfactant • So who is at risk? • more frequent in caucasian • more frequent in males than females • prematurity 13 14 Newborn at Risk Respiratory Distress Nursing assessment, you’re going to see – Respiratory – tachypnea, apnea (Normal is 30-60) – Chest – retractions, grunting, nasal flaring – Skin color – pallor, mottling, cyanosis 15 • Nursing Care Plan, page 744, Care of the Newborn with Respiratory Distress • Turn to • Table 28-1, page 742 Clinical Assessment Associated with Respiratory Distress • Respiratory • - tachypnea (RR > 60) is the most frequent • and easily detected sign of respiratory distress • - apnea (bad sign) • sign of • -metabolic alterations • - CNS disease • -IVH • -sepsis • -prematurity • Chest • work of breathing • -retractions -grunting -nasal flaring 16 17 10:10 Newborn at Risk Respiratory Distress • Nursing Care – Surfactant replacement – Oxygen – ventilation (ex: oxy hood/tent) – ABG’s monitored – IV fluids/TPN (ex: Central lines) – Cluster care – Supportive care 18 12:18 3) Transient Tachypnea of the Newborn (TTN) • Failure to clear airways of lung fluid (in utero fluid is produced, if this fluid isn’t cleared from the pressures on chest from birth, then TTN. C-Section don’t get this squeeze.) – Mild intrauterine asphyxia • Maternal over sedation, bleeding, IDM – Difficult birth • Breech birth, prolapsed cord • C/Section birthInfant may have tachypnea with shallow rapid respirations or grunting respirations. Retractions and increased effort with breathing nasal flaring. • REVIEW: • Normal Respiratory Rate 30-60 per minute 19 TTN Nursing Assessment • Little or no difficulty breathing at birth • Shortly after… – Grunting – Flaring – Mild cyanosis – Tachypnea- usually by 6 hours of age •RR as high as 100-140/min. 20 TTN Nursing Care – Supplemental O2 – IV Fluids 21 15:05 WTF 16:35 4) Meconium Stained Amniotic Fluid As the baby stays in the fluid, this fluid will stain the baby • MAS • - 13% of births have meconium stained fluid • - of those 4-11% develop MAS Represents a fetal asphyxial insult • before/during labor Risk factors • Term SGA’s • Postterm • Long labors 22 Meconium Aspiration Syndrome (MAS) Meconium fluid has aspirated into the baby’s lungs • Air trapping, if not released can rupture/pneumothorax • Alveoli overdistention • Possible pneumothorax • Chemical pneumonitis 23 19:40 Nursing Care of the Newborn with Meconium Aspiration Syndrome • Prevention of aspiration (Prevent!!) – – – – – – Detect meconium stained amniotic fluid Suction ASAP Mechanical ventilation Surfactant Antibiotics Supportive care 24 20:35 5) Newborn at Risk Cold Stress • Cold stress- excessive heat loss resulting in the use of compensatory mechanisms (increased respirations, nonshivering thermogenesis) • Infant heat production is by nonshivering thermogenesis • Burning of brown fat • Requires energy – utilizes O2 and glucose – Leading to Hypoxemia ( < 40mg/dL ) • Which Produces acids • Decreases surfactant production 25 Cold Stress Chain of Events 26 Ladewig et al, P. 697 • Figure 26–8 Cold stress chain of events. The hypothermic, or cold-stressed, newborn attempts to compensate by conserving heat and increasing heat production. These physiologic compensatory mechanisms initiate a series of metabolic events that result in hypoxemia and altered surfactant production, metabolic acidosis, hypoglycemia, and hyperbilirubinemia. • Cold stress is excessive heat loss resulting in the use of compensatory mechanisms to maintain core body temperature • Heat loss occurs in the newborn through evaporation, convection, conduction, and radiation. 27 21:55 Methods of Heat Loss • Evaporation– loss of heat incurred when water is converted to a vapor. Drying the newborn and etc. • Convection-the loss of hear from the warm body surface to the cooler air currents (ie. air conditioned rooms, air currents, O2 by mask, & removal from incubator into cooler air) • Conduction-the loss of heat to a coolder surface by direct skin contact (cold hands, cool scales, cold stethoscope etc) • Radiation– heat transfers from heated body surface to cooler surfaces and objects NOT in direct contact with the body (wall of a room or incubator, objects near the infant 28 Newborn at Risk Cold Stress • Signs/Symptoms – ↑ movement – ↑ respirations – ↓ skin temperature – ↓ peripheral perfusion (cyanotic looking) – Hypoglycemia- producing heat uses up stores – Metabolic acidosis 29 Newborn at Risk Cold Stress • Nursing care – Don’t let it happen!! – Assess skin temperature q 15-30 minutes – Warm slowly – rapid temperature elevation may produce apnea – Remove plastic wrap, caps, or heat shields while re-warming – Warm intravenous fluids prior to infusion – Block heat loss by evaporation, radiation, convection, and conduction – Asses for hypoglycemia 30 • Don’t let it happen!! • - the amount of heat loss of an infant • depends a great deal on the nurses actions • What are some ways we can decrease heat loss? • - NTE • - prewarm surfaces • - avoid drafts • - ….. • Warm slowly • - rapid temperature elevation may cause • HYPOTENSION • APNEA 31 25:20 6) Hypoglycemia • Why treat? – To prevent CNS damage or death 32 Hypoglycemic Neonate • At Risk – – – – – – – Sick and stressed neonates Infants of diabetic mothers SGA infants Smaller twin will have less stores Male infant Preterm AGA Mother with preeclampsia 33 Signs of hypoglycemia • • • • • • • Lethargy or jitteriness/tremor Poor feeding Vomiting Pallor, cyanosis Apnea, Irregular Respirations, Respiratory Distress Tremors, jerkiness, seizure activity High pitched cry (meaning neurological origin) 34 Glucose level • • Hypoglycemic newborn’s plasma glucose concentration is 40 mg/dl or lower. Signs of hypoglycemia may occur before 40 mg/dl and require intervention 35 27:55 Capillary blood specimen site • To check blood glucose, capillary blood is usually drawn from newborn’s heel. Avoid the shaded areas to prevent injury to arteries or nerves in the foot. 36 Care of the Hypoglycemic Neonate • Early formula feeding or breastfeeding • If too ill, gavage feeding or IV infusion of D5W • Continue to monitor adequacy of treatment • Conserve energy stores • Maintain a neutral thermal environment 37 30:40 7a) Hyperbilirubinemia • Bilirubin (Normal bilirubin level is ~10-14) – potential toxin collects in fatty tissue and brain kernicterus – Jaundice – skin yellow due to deposit of bilirubin in tissues • Up to 60% of term newborns will have clinical jaundice; ↑ for premature infants • Unconjugated bilirubin is a breakdown product derived from hemoglobin released from destroyed RBC’s=indirect bilirubin • To be eliminated from the body, conjugation of bilirubin occurs. Conjugation is the conversion of yellow lipid soluble pigment into water-soluble pigment=direct bilirubin 38 31:55 Newborn at Risk Hyperbilirubinemia • Risk factors – – – – – – – Fetal-maternal ABO/Rh incompatibilities Prematurity Cephalohematomas- from birth trauma Bruising Birth trauma Polycythemia Delayed meconium passage, which are normally excreted thru stool 39 Newborn at Risk Hyperbilirubinemia • Classification – Physiologic jaundice – Breastfeeding / Breast milk jaundice – Pathologic jaundice 40 • Physiologic jaundice in the term newborn • - typically peaks at 3-4 days then declines over the first week of life • usually the total bili will be < 12 mg/dLbili can go as high as 17 with multiple risk factors 41 • Breastfeeding jaundice (early onset) - compared to formula fed infants--breast fed infants are 3-6X more likely to develop moderate to severe jaundice (moderate = bili> 12, severe= bili >15 mg/dL) - due to mild dehydration (decreased volume of breast milk) - dehydration may cause a delay in meconium passage 42 • Breastmilk jaundice (late onset) • - occurs later—bili usually peaks at day 614 can develop in up to 1/3 of healthy breast fed infants bili can vary from 12-20, at this age it would not be considered pathologic- bili level usually continually falls after 2 wks of age, however, it may remain elevated for 1-3 months. if the cause of the jaundice is in question, the mom may be asked to stop breastfeeding, but continue to express breastmilk, with formula substitution, if the bili drops rapidly over 48 hours, this confirms breastmilk jaundice and breastfeeding may be resumed. 43 32:52 Hyperbilirubinemia - Physiologic • RBCs shorter life span • Immature liver • Lack of intestinal bacteria to conjugate bilirubin • Poor hydration hinders urine & bowel elimination 44 Newborn at Risk Hyperbilirubinemia • Nursing Care – – – – – I&O Hydration Observe for jaundice Phototherapy Transfusions – Nursing care plan, page 779-780 45 • • • • • • • • • • • • • • • • • • I&O - monitor for first stool WHY? Hydration - early frequent feeds - more severe IVF Jaundice - note when it occurs - monitor progression - transcutaneous bili check before discharge Phototherapy - use of visible light to convert bilirubin into water soluble isomers that can be eliminated without being conjugated in the liver Transfusions - for severe anemia - exchange transfusions to replace the baby’s damaged blood ↑ RBC count and ↓ bili level 46 35:30 Hyperbilirubinemia Pathologic Jaundice • Hemolytic disease of the newborn (HDN) due to a – Rh incompatibility – ABO incompatibility • Jaundice at birth or in the first 24 hours of life – Physiologic jaundice occurs after 24hrs • Hydrops fetalis- massive edema in the fetus or newborn, usually in association with RBC destruction. (blood incompatibility) Rhogam to prevent. • Kernicterus- toxic accumulation of bilirubin in tissues caused by hyperbilirubinemia. 47 • Rh incompatibility • - Rh negative Mom/Rh positive Dad • have an Rh positive baby • - baby’s blood cells cross over to the Rh negative Mom • - Mom develops antibodies (Rh sensitization) • - subsequent pregnancies are at risk for HDN • - How do we avoid this? RhoGAM • Signs/Symptoms • During pregnancy • - placenta helps rid some bili, but not all = • mild anemia/hyperbilirubinemia/jaundice • - liver/spleen and bone marrow can’t keep • up with RBC destruction= • severe anemia & liver/spleen enlargement • - baby’s organs can’t handle the severe anemia • leading to heart failure with fluid buildup in tissues • and organs= hydrops fetalis • • • • After birth - baby’s liver can’t conjugate the large amount of bili severe hyperbilirubinemia and jaundice - leading to the most severe form of hyperbilirubinemia kernicterus 48 7b) Hemolytic Disease of the Newborn • Rh incompatibility – Rh neg mother with Rh positive newborn – Jaundice, anemia, hemolysis of RBC’s, increased immature RBCs – Most severe form of hemolytic disease of newborn – Hydrops Fetalis – Multi-organ system failure due to severe anemia – Rhogam for the block 49 • Hemolytic disease of the newborn secondary to Rh incompatibility – Isoimmune – Rh neg mother with Rh positive newborn passes maternal antibodies to fetal circulation that destroy the fetal RBC • Jaundice, anemia, increased immature RBCs (erythroblasts) r/t hemolysis of RBC’s, • Most severe form is hydrops fetalis – occurs when maternal antibodies attach to the Rh site on the fetal RBC, making them susceptible to destruction by phagocytes; multi-organ system failure; frequently fatal 50 38:20 Hemolytic Disease of the Newborn Same thing, but not as severe • ABO incompatibility • Mother blood type O & infant A or B can result in jaundice but rarely hemolytic disease – Jaundice, hyperbilirubinemia, hepatosplenomegaly r/t hemolysis of RBC’s – Rh is not a factor 51 Care of Newborn at Risk for Hyperbilirubinemia • Identifying the Cause of Hemolytic Disease – Blood type – Coombs’ test • Indirect- amount of Rh + antibodies in mother’s blood • Direct- presence of antibody coated Rh+ RBC’s in newborn – Serum bilirubin – CBC – Reticulocyte count 52 39:35 Care of Newborn at Risk for Hyperbilirubinemia • Alleviate anemia • Exchange transfusion – Withdraw & replace all newborn’s blood with donor blood • Increase serum albumin levels • Reduce serum bilirubin – Phototherapy – Drug therapy- Phenobarbital (Bilirubin binds to Phenobarbital, so when it goes… the bilirubin does too) 53 8) Newborn at Risk for Anemia • Normal Hgb – Term 15-20 g/dL, less 14 = anemia – Preterm 14-18 g/dL, less 13 = anemia • Hemoglobin levels < 14g/dl in term infant or 13 g/dl in preterm 54 Common Causes of Anemia • Blood Losses – Placental bleeding – Intrapartal blood loss – Umbilical cord bleeding – Birth trauma – Cerebral bleeding • Hemolysis • Impaired red blood cell production 55 42:10 Physiologic anemia • Decreased hgb first 6-12 weeks • Production of RBC’s stopped in response to elevated O2 • Hgb levels decrease, bone marrow production resumes 56 Care of the Newborn with Anemia • Early Detection and correction of pathological anemia – Pale infant, poor weight gain, tachycardia, tachypnea, apneic episodes • Ensure newborn well-being. Follow checklist: airway, breathing, circulation, neutral thermal environment, early detection and intervention of hypoglycemia, promote comfort & bonding • Monitor: total blood out 57 Anemia • Signs & Symptoms – ↓ Hgb – Pallor – ↓ BP – Tachycardia – Tachypnea – Apneic episodes 58 Nursing Care - Anemia • Mild anemia – Iron supplement • More severe – Hydration – Blood Transfusion 59 9) Newborn at Risk Polycythemia • • • • ↑ blood volume ↑Hct > 65%-70% Hgb > 22 g/dl More common in: – – – – – – IDM SGA Postmature Term infants with delayed cord clamping Maternal-fetal transfusion Twin-to-twin transfusion 60 Newborn at Risk Polycythemia Often asymptomatic – S/S •CHF - Tachycardic, Respiratory distress (30-60 is normal) •↑ bili •↓ peripheral pulses 61 Nursing Care • Exchange transfusion with FFP or albumin • Monitor VS during transfusion • +/- phototherapy • Treatment goal – Reduce hematocrit to a range of 55%-60%, this is a success 62 48:38 Newborn at Risk Infection • Sepsis Neonatorum – Newborns up to 1 month of age are particularly susceptible – Prematurity increases risk • Caused by organisms that do not cause infection in older children 63 Predisposing Factors • Maternal antepartal infections – TORCH - Toxoplasmosis, Rubella, Cytomegalic Inclusion Disease, Herpes (all deadly to newborns) • Intrapartal – Amnionitis, passage through the birth canal, Group B hemolytic Strep, Herpes, Gonococci, Listeria • Nosocomial – Pseudomonas, Staphylococcus aureas and epi 64 50:43 Diagnosis • Usual Lab work – CBC, Blood Cultures (best) and Sensitivity with Gram Stain, Urine for antibody screen, C-Reactive Protein level, other cultures as recommended or ordered • Chest x-ray • If viral infection is suspected TORCH (toxoplasmosis, other, rubella, cytomegalovirus, herpes virus) titers are drawn. Skull and bone x-rays to check for any damage. 65 51:42 • • • • Nursing care Infants with sepsis can rapidly deteriorate! Supportive care Administer medications as ordered Recognition of the signs of sepsis- hypotonia, color changes – pallor, dusky, cyanosis, grey, temperature instability, feeding intolerance, hyperbilirubinemia, tachycardia, apnea, behavioral changes, RDS-type symptoms – Respiratory Distress symptoms: • Incr respirations, nasal flaring, retractions, grunting, peripheral edema • A sub normal temperature, is a cardinal sign of sepsis. 66 53:42 10) Antibiotic Therapy Review proper dose/kg Therapeutic peak/trough values Method of administration (thru IV, Central line is better) Incompatibilities Side effects 67 54:23 Duration of Antibiotic Therapy • Therapy initiated before test results are final • Treatment of infection with 2 broad spectrum antibiotics per intravenous route • When the pathogen and its sensitivities are determined appropriate specific antibiotic therapy is implemented for 7-14 days. 68