the lecture by Dr Ezeanochie
advertisement

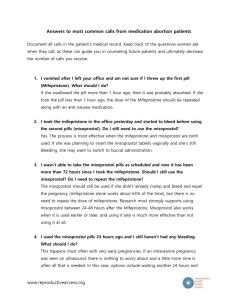
Safe abortion- medical methods of termination, post abortion care and referral, pre and post abortion counseling 27/06/2014 Learning Objectives Definition of Abortion Comprehensive abortion care Concept of unsafe/safe abortion Protocols for medical termination Components and principles of Post abortion care Introduction The termination of a human pregnancy before the age of viability Unsafe abortion is defined by the World Health Organization (WHO) as a procedure for terminating an unintended pregnancy, carried out either by persons lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both. Comprehensive abortion care Provide safe, high-quality services, including abortion, postabortion care and family planning; Decentralize services so they are closer to women; Be affordable and acceptable to women; Understand each woman’s particular social circumstances and individual needs and tailor her care accordingly; Address the needs of young women; Reduce the number of unintended pregnancies and abortions; Identify and serve women with other sexual or reproductive health needs; Be affordable and sustainable to health systems. Pre-abortion encounter Information, counselling and decision-making Medical history Physical examination Laboratory and other investigations (if necessary and available) Discussing contraceptive options Objectives of Pre-abortion encounter Provide information and offer counselling in a way that a woman can understand to allow her to make her own informed decisions Confirm pregnancy status and determine location and duration. Evaluate for any medical conditions that require management or may influence the choice of abortion procedure. Provide an opportunity to discuss future use of contraception. Medical Termination Use of pharmacological drugs to terminate pregnancy. Sometimes the terms “non-surgical abortion” or “medication abortion” are also used. Medical abortion is a multistep process involving two medications (mifepristone and misoprostol) and/or multiple doses of one medication (misoprostol alone). Peculiarities Avoids surgery Mimics the process of miscarriage Controlled by the woman and may take place at home Takes time (hours to days) to complete abortion, and the timing may not be predictable Women experience bleeding and cramping, and potentially some other side-effects (nausea and vomiting) May require more clinic visits than MVA Protocols for Medical Termination Up to 9weeks (63 days), preferred option Mifepristone 200mg oral stat, then Misoprostol 800ug stat (oral, vaginal or sublingual) 24-48 hours after mifepristone If less than 7weeks, may use 400ug misoprostol stat Alternative option (up to 63 days ie 9weeks) when mifepristone isn't available Misoprostol 800 μg Vaginal or sublingual Every 3-12 hours up to 3 doses Stop when patient stats bleeding 9–12 weeks (63–84 days, preferred option) Mifepristone 200mg stat orally, then Misoprostol 800 μg, then 400 μg subsequently (Vaginal, then vaginal or sublingual) Every 3 hours up to 5 doses Start 36–48 hours after taking mifepristone Alternative option (9-12weeks), when mifepristone is not available Misoprostol 800 μg Vaginal or sublingual Every 3-12 hours up to 3 doses Stop when patient stats bleeding 12 – 16 weeks Misoprostol 800 μg, then 400 μg Vaginal, then vaginal or sublingual OR Misoprostol 400 μg, then 400 μg Oral, then vaginal or sublingual Every 3 hours up to 5 doses Start use 36–48 hours after taking mifepristone Alternative Misoprostol 400 μg Vaginal or sublingual Every 3 hours up to 5 doses Buccal misoprostol Sublingual Follow-up Usually seen 1 – 2 weeks after intake of drugs Confirm complete abortion by clinical examination, negative PT or ultrasound if indicated Suspect ectopic pregnancy if no response or features of rupture Pain management Respectful, non-judgmental communication Verbal support and reassurance Thorough explanation of what to expect The presence of a support person who can remain with her during the process (if the woman desires it) Hot water bottle or heating pad Pain mgt contd Analgesia (NSAIDs, e.g. ibuprofen 400–800 mg and opiod analgesia e.g tramadol) Anxiolytics / sedatives (e.g. diazepam 5– 10 mg) Adjuvant medications may also be provided, if indicated, for side-effects of misoprostol (e.g. loperamide for diarrhoea) Pain mgt contd >12 weeks’ gestation In addition to NSAIDs, offer at least one or more of the following: oral opioids; intramuscular (IM) or intravenous (IV) opioids; Paracetamol is usually ineffective for pain management during an abortion and is not recommended Give oral analgesics 30-45 minutes before drugs to ensure maximal pain relief Caution It is essential that the woman knows to seek medical attention for: prolonged or heavy bleeding (soaking more than two large pads per hour for two consecutive hours) fever lasting more than 24 hours Malodourous vaginal discharge or feeling generally unwell more than 24 hours after misoprostol administration Post abortion care Post abortion care is a strategy to address this problem by treating women with complications, providing family planning services to prevent future abortions, counseling and referring women for other needed services, and engaging communities. PAC Postabortion care is an approach for reducing deaths and injuries from incomplete and unsafe abortions and their related complications. Postabortion care is an integral component of comprehensive abortion care Post abortion encounter Follows principles of PAC Counselling on family planning and linkage to other reproductive health services Counselling should be non-judgemental and woman centred Components Treatment of incomplete and unsafe abortion and complications Counselling to identify and respond to women’s emotional and physical health needs Contraceptive and family-planning services to help women prevent future unwanted pregnancies and abortions Components of PAC Reproductive and other health services that are preferably provided on-site or via referrals to other accessible facilities Community and service-provider partnerships to prevent unwanted pregnancies and unsafe abortions, to mobilize resources to ensure timely care for abortion complications, and to make sure health services meet community expectations and needs. Conclusion Unsafe abortion remains a serious public health problem and a leading cause of maternal morbidity and mortality Delivery of safe abortion services especially medical abortion can help reduce complications associated with unsafe abortion Family planning services and linkage to other reproductive health services are essential components of comprehensive Post abortion care