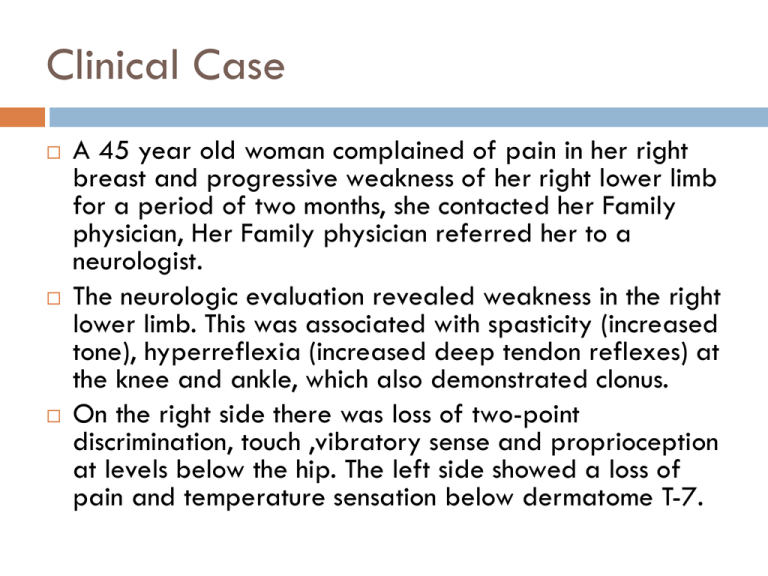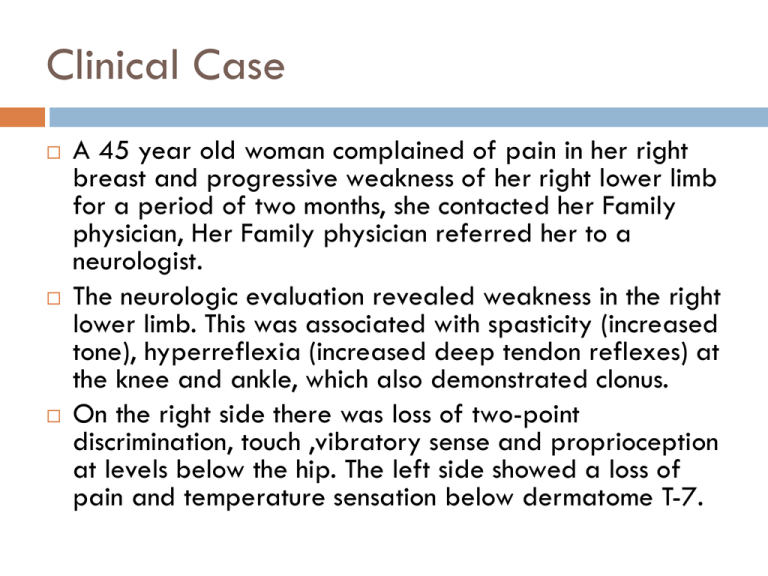
Clinical Case
A 45 year old woman complained of pain in her right
breast and progressive weakness of her right lower limb
for a period of two months, she contacted her Family
physician, Her Family physician referred her to a
neurologist.
The neurologic evaluation revealed weakness in the right
lower limb. This was associated with spasticity (increased
tone), hyperreflexia (increased deep tendon reflexes) at
the knee and ankle, which also demonstrated clonus.
On the right side there was loss of two-point
discrimination, touch ,vibratory sense and proprioception
at levels below the hip. The left side showed a loss of
pain and temperature sensation below dermatome T-7.
Clinical Case Of Spinal Cord cont..
MRI of a patient indicated to have an
extramedullary tumor expanding from the dorsal
roots at spinal cord levels T-5,6.
Based on the symptoms and clinical findings what is
your diagnosis ?
1.
This patient noticed ulcers on
the fingers of both of his
hands. They were associated
with no pain and appeared to
be the residua of burns. The
probable site of damage
responsible for this defect is
the
a. Posterior column
b. Anterior horn
c. Clarke’s column
d. Spinothalamic tract
e. Spinocerebellar tract
A 45 year old man noticed a weakness of his right
hand which was progressing and causing him problems.
He decided to see his doctor.
On examination he demonstrated bilateral weakness,
atrophy, and fasciculations of the intrinsic muscles of his
hands and shoulders. Upper motor neuron syndrome
signs, i.e., weakness, hypertonia, hyperreflexia,
positive Babinski, were evident in both lower
extremities. Dermatomes C-2 through T-6
demonstrated bilateral loss of pain and temperature
sensation. There was bilateral impairment of position
and vibratory sense below the hips.
MRI investigation showed a central cavitation at C-2
through T-7 which expanded symmetrically in all
directions. It involved the anterior white commissure
(spinothalamic fibers) and included portions of the
posterior white columns, lateral white funiculus, and
anterior gray horns.
Somatosensory Pathway(Dorsal Colum)
Somatosensory Pathway
Posterior column pathway
carries sensation of highly
localized touch, pressure,
vibration.
Posterior column pathway
includes:
Fasciculus cuneatus tract
Fasciculus gracilus tract Carries fine touch,
pressure, vibration,
sterognosis and
conscious Proprioceptive
sensations.
Dorsal Colum tracts
dorsal
cloumn
pathway
dorsal column
pathway
Left
spinal cord injury
Loss of sense of:
•touch
•proprioception
•vibration
in left leg
Dorsal Colum Lesions
Sensory ataxia
Patient staggers; cannot
perceive position or
movement of legs
Visual clues help
movement
Rombergism
An 85-year-old man is being evaluated for gait
difficulties. On examination it is found that joint
proprioception is absent in his toes. People with
impaired position sense will usually fall if they stand
with their feet together and do which of the
following?
Flex the neck
Extend their arms in front of them
Flex the knees
Turn the head
Close their eyes
Case cont….
The ability to recognize an unseen familiar object placed in
the hand depends on the integrity of which pathway
Ventral spinocerebellar tract
Dorsal column
Dorsal spinocerebellar tract
Vestibulospinal tract
Spinothalamic tract
Clinical Case Spinal cord
A patient displays a symmetrical loss of pain
and temperature on the shoulder area on both
Sides of the body with no loss of tactile
sensation. Pain and temperature and tactile
sensation Are normal over the rest of the body.
This condition would be due mostly likely to
lesion of :
Clinical Case Spinal cord cont…
A.
B.
C.
D.
anterior white commissure from C2 to C4
anterior white commissure from T1 to T5
Anterolateral system on right at C2
paracentral lobule on the left
Clinical Case Spinal cord cont..
A 54 year old male presents with complaints of loss
of pain and temperature sensation in his arms and
chest only. What is the lesion causing these
symptoms
Complete cord transection at C5
Central cavitation of the cervical spinal cord
Demyelination of the dorsal columns
Disc herniation
Clinical case
A 45 yr old man is brought to ER complaining of
inability to move his left leg
HPI- He was stabbed in the back Hr ago while
defending his girlfriend from a mugger
PE-Moderate bleeding; Stab wound at the posterior
cervical spinous prominence (c7)on the left side;
Weakness on finger flexion; extension of left finger;
inability to sense of vibration of tuning fork along left
lower limb; loss of pain and temperature sense in
contralateral limb.
Imaging: MRI: Haematoma at the level of C-T1 in the
left of the spinal cord.
1. Which of the following in not characteristic of the BrownSequard syndrome.
A.
Contralateral paralysis below the lesion level.
B.
Contralateral loss of temperature sensation 2-3 segments
below the lesion.
C.
Ipsilateral loss of position and vibratory sense below the
lesion level.
D.
An ipsilateral segmental area of atrophy and reflex loss at
the segmental lesion region.
E.
Contralateral loss of pain sensation 2-3 segments below the
lesion.
Brown-Sequard Syndrome
Ipsilateral paresis accompanied by ipsilateral
impairment of touch and vibration sense, and
contralateral loss of pain and temperature sense.
Case
An old 52 African-American man presented to the ER with a one
week history of "unable to stand". This was progressively
worsening over the week and more marked on the left lower
extremity. The patient also stated that he was unable to feel
anything (numbness) in his legs. He also complained of inability
to feel when he urinated as well as mild urinary incontinence. The
patient had a spinal tumor (meningioma) removed from the
upper thoracic spine 7 months prior to this presentation. At that
time he presented with a Brown Sequard type syndrome (left
lower extremity weakness) and a T4 sensory level. After the
tumor resection, the patient's symptoms improved significantly to
the extent that he was ambulating with a cane. However, on
presentation he was now wheelchair-bound.
Anterolateral system
The Anterolateral Pathway
Provides sensations of
“crude” touch, pressure,
pain, and temperature
Ascend within the anterior
or lateral spinothalamic
tracts:
Anterolateral System (Pain &Temp)
spinothalamic pathway
Left
spinal cord injury
Loss of sense of:
•Touch
•Pain
•Warmth/cold
in right leg
Spinothalamic Tracts
Located lateral and ventral to
the ventral horn
Carry impulses concerned
with pain and thermal
sensations (lateral tract) and
also non- discriminative
touch and pressure (medial
tract)
Fibers of the two tracts are
intermingled to some extent
In brain stem, constitute the
spinal lemniscus
Fibers are highly somatotopically arranged, with those
for the lower limb lying most
superficially and those for the
upper limb lying deeply
Lateral Spinothalamic Tract
Carries impulses concerned
with pain and thermal
sensations.
Axons of 1st order neurons
terminate in the dorsal horn
Axons of 2nd order neuron
(mostly in the nucleus
proprius), decussate within
one segment of their origin, by
passing through the ventral
white commissure & terminate
on 3rd order neurons in ventral
posterior nucleus of the
thalamus
Thalamic neurons project to
the somatosensory cortex
Anterior Spinothalamic Tract
Carries impulses concerned
with non- discriminative touch
and pressure
Axons of 1st order neurons
enter cord terminate in the
dorsal horn
Axons of 2nd order neuron
(mostly in the nucleus proprius)
may ascend several segments
before crossing to opposite
side by passing through the
ventral white commissure &
terminate on 3rd order neurons
in ventral posterior nucleus of
the thalamus
Thalamic neurons project to
the somatosensory cortex
Spino-reticulo-thalamic System
The system represents an additional route by
which dull, aching pain is transmitted to a
conscious level
Some 2nd order neurons terminate in the
reticular formation of the brain stem, mainly
within the medulla
Reticulothalamic fibers ascend to intralaminar
nuclei of thalamus, which in turn activate the
cerebral cortex
Spinocerebellar Tracts
The spinocerebellar system
consists of a sequence of
only two neurons
Two tracts: Posterior &
Anterior
Located near the
dorsolateral and
ventrolateral surfaces of the
cord
Contain axons of the second
order neurons
Carry information derived
from muscle spindles, Golgi
tendon organs and tectile
receptors to the cerebellum
for the control of posture and
coordination of movements
Posterior Spinocerebellar Tracts
Present only above level
L3
The cell bodies of 2nd
order neuron lie in Clark’s
column
Axons of 2nd order
neuron terminate
ipsilaterally (uncrossed)
in the cerebellar cortex
by entering through the
inferior cerebellar
peduncle
Ventral Spinocerebellar Tracts
The cell bodies of 2nd order neuron
lie in base of the dorsal horn of the
lumbosacral segments
Axons of 2nd order neuron cross to
opposite side, ascend as far as
the midbrain, and then make a
sharp turn caudally and enter the
superior cerebellar peduncle
The fibers cross the midline for a
second time within the cerebellum
before terminating in the
cerebellar cortex
Both spinocerebellar tracts convey
sensory information to the same
side of the cerebellum
Spinotectal Tract
Ascends in the anterolateral
part in close association with
spinothalamic system
Primary afferents reach dorsal
horn through dorsal roots and
terminate on 2nd order neurons
The cell bodies of 2nd order
neuron lie in base of the dorsal
horn
Axons of 2nd order neuron
cross to opposite side, and
project to the periaquiductal
gray matter and superior
colliculus in the midbrain
Spino - olivary Tract
Indirect spinocerebellar pathway (spinoolivo-cerebellar)
Impulses from the spinal cord are relayed to
the cerebellum via inferior olivary nucleus
Conveys sensory information to the
cerebellum
Fibers arise at all level of the spinal cord
Spinoreticular Tract
Originates in laminae IVVIII
Contains uncrossed
fibers that end in
medullary reticular
formation & crossed &
uncrossed fibers that
terminate in pontine
reticular formation
Form part of the
ascending reticular
activating system
Spino-Olivary Tracts
Project to accessory olivary nuclei and cerebellum.
Contribute to movement coordination associated
primarily with balance.
Spinotectal Tracts
Project to superior colliculi of midbrain.
Involved in reflexive turning of the head and eyes
toward a point of cutaneous stimulation.
Spinoreticular Tracts
Involved in arousing consciousness in the reticular
activating system through cutaneous stimulation.
Following an automobile accident, an eighteen year
old male was hospitalized for several weeks. A
neurological exam at that time revealed the
following:
1. Complete loss of conscious proprioception in the
right lower limb.
2. Babinski sign on the right.
3. Inability to detect pain and temperature sensation
on the medial side of the antecubital fossa
(medialepicondyle) on both upper limbs.
4. Inability to detect pain and temperature at the
apex of the left axilla, in all the intercostal spaces
on the left, and in the left lower limb.
5. The patient could feel a gentle squeezing of both
thumbs, right and left middle fingers, and the left
little finger.
6. No sensation to squeezing could be detected in the
right little finger.
Based on this exam, a single lesion may be
found at which of the following levels?
Caudal
medulla in the midline
Right side of the spinal cord at C8
Left side of the spinal cord at T1
Right side of the spinal cord at C4 - C5
Left side of the spinal cord at C4 - C5
Motor Loss
Ipsilateral paralysis below the lesion. Paralysis is the "Upper
Motor Neuron" or spastic type; there is spasticity, slow (disuse)
muscle atrophy, hypertonia, ankle clonus and a positive Babinski
sign. Superficial reflexes, e.g., the abdominal and cremasteric are
lost.
Spastic paralysis is attributed to interruption of the lateral
corticospinal tract and the accompanying lateral reticulospinal tract.
Loss of these upper motor neurons deprives the anterior horn cells,
i.e., lower motor neurons, of the impulses which generate contraction
of skeletal muscle, hence, weakness (paresis) or paralysis.
Hypertonia and hyperreflexia appear to result from loss of the
inhibitory effects of these two descending motor pathways on the
stretch reflexes, leaving them hyperexcitable to segmental muscle
afferents
It may be possible to also demonstrate a "Lower Motor
Neuron Syndrome" or flaccid paralysis ipsilaterally at
the level of the lesion. If the anterior horn cells
supplying the skeletal muscles are injured at the level of
the lesion then these muscles are denervated. This
paralysis is of the flaccid type; muscles undergo rapid
atrophy due to loss of the trophic influence of the
nerves as well as disuse. Tone and tendon reflexes are
diminished since they are reflex responses and the
injured lower motor neurons are the "final common
pathway" to the muscle in the stretch reflex, hence,
there is no reflex.
Loss of conscious proprioception, two-point discrimination and
vibratory sense ipsilaterally is due to interruption of the posterior
white columns (fasciculus gracilis/cuneatus). This is frequently
accompanied by a Romberg sign. A normal individual, standing
erect with heels together and eyes closed, sways only slightly. Stable
posture is achieve by 1) a sense of position from the vestibular
system, 2) awareness of the position and status of muscles and joints
by conscious proprioception and 3) visual input regarding our
position. Closing the eyes has only slight effect on the normal
individual's stance since the vestibular and conscious proprioception
systems are sufficient. In a patient with an impaired posterior column
conscious proprioception is diminished; when the eyes are closed loss
of both systems renders the patient unstable and they are likely to
sway or fall to the side.
Pain and temperature sensation is lost below the lesion, on
the opposite side beginning about one dermatomal segment
below the level of the lesion. These sensations are carried
by the lateral spinothalamic tract whose fibers originated on
the side opposite the lesion but which crossed in the anterior
white commissure. Dorsal root afferents carrying pain and
temperature synapse in the dorsal gray; the second order
neuron crosses in the anterior white commissure along an
ascending path for a distance of about one spinal segment.
Because of the oblique ascent of the crossing fibers in the
anterior white commissure, injury of the spinothalamic tract is
not likely to be carrying sensation from that level.
A careful sensory evaluation may reveal that at the
dermatomal level of the lesion there is a bilateral loss
of pain and temperature sensation. Since the second
order neurons from both sides cross in the midline below
the central canal, a hemisection of the cord may
interrupt the crossing fibers from both sides and
produce this limited bilateral deficit.
The pain in the left breast was the result of the
pressure of the tumor on the dorsal root.
Hemisection of Spinalcord
At the level of
lesion
side
Sensory
disturbance
Motor
disturbance
Reflexes
On the same side
Below
On the Opposite
side
Loss of all sensation
Loss of the dorsal
Loss of
1-superfecial sensations column due to
1-pain & temp.
2-deep sensations
damage of gracil &
due to damage of
cunite leading to loss lateral
of
spinothalamic tract.
1. fine touch
2-crude touch due
2. kinesthetic
to damage of
3. vibration
ventral
4. sterognosis
spinothalamic tract.
1-LMNL
UMNL due to
2-paralysis of muscles damage of pyramidal
which its supply arising tract
from damage
Loss of all reflexes
which its centers in
damage segments
On the same side
1-loss of flexor
withdrawal reflex
2-increase crossed
extensor reflex
Above
On the same side
Hyperanasthesia
(Hypersensitivity)
increase sensitivity to
1. pain
2. touch
3. Temp.
Anterior cord syndrome
Loss of motor function and pain-temperature sensation
below the level of the lesion
Typically seen following hyperflexion injuries with
impingement of bone or herniated disc tissue directly
on the anterior spinal cord
Due to mechanical compression of the anterior spinal
artery and secondary infarction of the anterior spinal
cord
Rarely due to aortic dissection interrupting the blood
supply to the anterior spinal arteries
posterior column function is not affected (position
sense and vibration sense)
Posterior cord syndrome
proprioceptive sensory loss.
Usually due to posterior spinal artery occlusion,
chronic atherosclerosis and impaired collateral
circulation, tumors or discs compressing the posterior
spinal cord, or vitamin B12 deficiency.
Pain and temperature sensory function + motor
function not affected.
Brown-Sequard syndrome
lateral cord syndrome due to a lesion involving half
of the spinal cord
Ipsilateral loss of motor function and proprioceptive
sensory function + contralateral loss of paintemperature sensation.
Most commonly due to traumatic hemisection of the
spinal cord (eg. stabbing knife thrust)
Syringomyelia
the result of central cord cavitation affecting a few segments, and usually involving
the cervical spinal cord
frequently found in Arnold-Chiari malformations affecting the upper cervical cord and
medulla
mainly affects the crossing fibres of the spinothalamic tract as they decussate in the
ventral white commissure => bilateral pain-temperature sensory loss over a few
segments eg. only affecting the neck and upper shoulders in a cape-like distribution
(or only affecting the upper limbs) with normal sensation above and below the
affected dermatomes
does not affect the spinothalamic tracts in the early stages => no initial lower trunk or
lower limb pain-temperature sensory loss
does not usually affect the dorsal columns => normal position sense ("dissociative"
sensory loss)
may rarely affect the lower motor neurons to the upper limbs early in the disease
course, and may eventually affect the corticospinal tracts
may affect the spinal extension of the trigeminal nucleus => face hypoesthesia in a
characteristic balaclava helmut distribut
Case Cont…
A patient of yours who is now in her late 40's walks with a
distinct limp. As you take her history she tells you that when she
was four years old and on an outing at the zoo with her family,
she got sick with an "upset stomach" and that she "couldn't
walk anymore" because of pain in her legs. When she returned
home her mother found that she had a fever of 103° F. The
following morning the child could not move her legs, and she
was taken to the hospital. Examination revealed that muscle
tone was greatly reduced in the lower limbs, and the patellar
and Achilles's tendon reflexes could not be elicited. Upper
limbs were not affected.
Clinical Case of Spinal cord cont..
•
•
•
A 23 yr old women complained of pain in her right
breast and progressive weakness of her right lower
limb for a period of many months.
The neurologic examination revealed weakness in the
right lower limb. This was associated with spasticity
(increased tone), hyperreflexia (increased deep tendon
reflexes) at the knee and ankle, which also
demonstrated clonus.
On the right side there was loss of two-point touch,
vibratory sense and proprioception at levels below the
hip. The left side showed a loss of pain and
temperature sensation below dermatome T-7.
–Conclusion of the diagnosis that the patient was determined to have an
extramedullary tumor expanding from the dorsal roots at spinal cord levels T5,6.
Pure hemisection of the cord rarely occurs but it is among the best cases for
illustrating the features of spinal cord injury.
•spastic paralysis
•lateral corticospinal tract
•loss of position sense, discriminative touch and vibratory sense on the
side of the lesion –
-involvement of the and the posterior white column on the side of the
lesion.
On the side opposite the lesion there is a loss of pain and temperature due
to involvement of the lateral spinothalamic tract.
•At times, it is possible to also demonstrate a bilateral sensory deficit
and flaccid paralysis at the level of the lesion.
Syringomyelia
•
•
A 55 year old man noticed a weakness of his left hand
and loss of pain in his both arms which was progressing
and causing him mental apathy and he felt he should
visit neurologist .
On examination he demonstrated bilateral weakness,
atrophy, and fasciculations of the intrinsic muscles of his
hands and shoulders. Upper motor neuron syndrome
signs, i.e., weakness, hypertonia, hyperreflexia, positive
Babinski, were evident in both lower extremities.
Dermatomes C-2 through T-6 demonstrated bilateral
loss of pain and temperature sensation. There was
bilateral impairment of position and vibratory sense
below the hips.
MRI investigation showed a central cavitation at C-2
through T-7 which expanded symmetrically in all
directions.
It involved the anterior white commissure
(spinothalamic fibers) and included portions of the
posterior white columns, lateral white funiculus, and
anterior gray horns.
Syringomyelia
Syringomyelia
the result of central cord cavitation affecting a few segments, and usually involving
the cervical spinal cord
frequently found in Arnold-Chiari malformations affecting the upper cervical cord and
medulla
mainly affects the crossing fibres of the spinothalamic tract as they decussate in the
ventral white commissure => bilateral pain-temperature sensory loss over a few
segments eg. only affecting the neck and upper shoulders in a cape-like distribution
(or only affecting the upper limbs) with normal sensation above and below the
affected dermatomes
does not affect the spinothalamic tracts in the early stages => no initial lower trunk or
lower limb pain-temperature sensory loss
does not usually affect the dorsal columns => normal position sense ("dissociative"
sensory loss)
may rarely affect the lower motor neurons to the upper limbs early in the disease
course, and may eventually affect the corticospinal tracts
Cauda equina syndrome
Slow progressive loss; often asymmetric or unilateral
Often due to chronic disc herniation
May be due to spinal tumors
Less severe back pain, may produce severe radicular symptoms
Sensory loss affects all sensory modalities - lumbar > sacral
Sensory loss may affect penis/clitoris and pubic area, and be asymmetrical
Sensory loss may follow a specific dermatomal pattern
Muscle weakness - lumbar > sacral
Muscle weakness mainly affects glutei, hamstrings, gastrocnemius and soleus
muscles
Muscle atrophy and fasiculations common
Tendon reflex loss - knee > ankle
Late bladder involvement (flaccid bladder)
Inferior cord syndrome
(conus medullaris) syndrome
Involvement of the terminal spinal cord
Usually of rapid onset
More severe back pain, less severe radicular symptoms
Symmetrical defects
Saddle distribution sensory loss +/- sensory dissociation
Tendon reflex loss - ankle > knee
Early consistent impotence +/- bladder involvement
Subacute lesions may produce UMN signs - hyperreflexia of ankle
jerks, increased anal tone and spastic bladder
Case
A 55-year-old man injured his thoracic spine in a
motor vehicle accident 2 years ago. Initially he had
a bilateral spastic paraparesis and urinary urgency,
but this has improved. He still has pain and thermal
sensation loss on part of his left body and
proprioception loss in his right foot. There is still a
paralysis of the right lower extremity as well.
Questions
In this patient, where would you expect the pain and
temperature abnormalities to begin?
a. Exactly at the level of the lesion
b. Four or five segments above the lesion
c. Four or five segments below the lesion
d. One or two segments above the lesion
e. One or two segments below the lesion