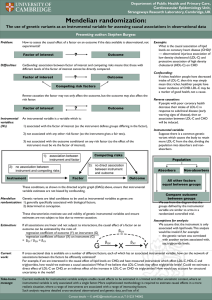
New Concepts in the Evaluation
and
Treatment of Dyslipidemia
Nathan D. Wong, PhD, FACC
Professor and Director
Heart Disease Prevention Program
Division of Cardiology
University of California, Irvine
President, American Society for
Preventive Cardiology
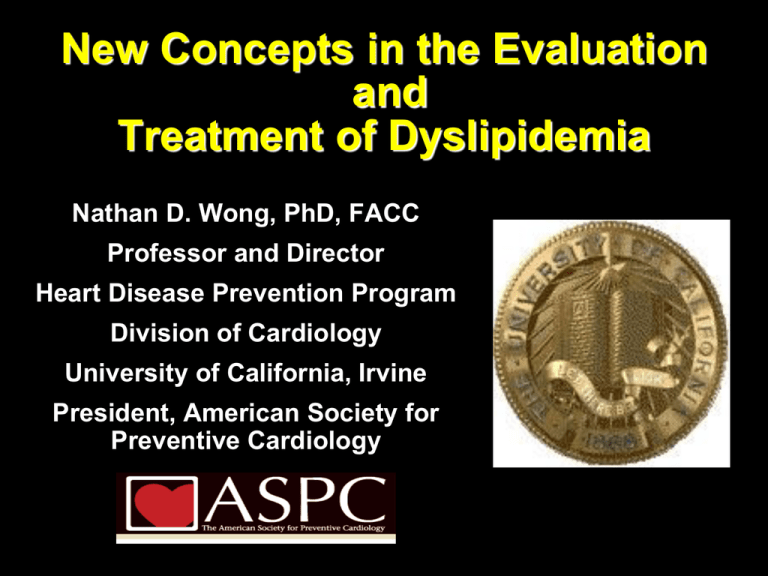
Lipoprotein Particles
VLDL
Density (g/ml)
0.95
Chylomicron
VLDL
Remnants
1.006
IDL
Chylomicron
Remnants
1.019
LDL-R
1.050
1.063
HDL2
Lp(a)
1.100
HDL3DL3
Only these lipoprotein particles
found in plaque at biopsy.
1.20
5
10
20
40
60
Particle Size (nm)
80
1000
Lipid Atherogenesis
HDL
Endothelial
injury
High plasma
LDL
LDL
+
VLDL
Adherence
of platelets
LDL infiltration
into intima
Release
of PDGF
Oxidative
modification
of LDL
Liver
Cholesterol
excreted
LCAT
APO-A1
Advanced
fibrocalcific
lesion
Other
growth
factors
+
Macrophages
Foam cells
Fatty streak
Unstable
lesion
lipid core
adventitia
Anti-atherosclerotic therapy
Stable
lesion
lipid core
adventitia
From Davies et al (1998
Proportion of U.S. Adults at Recommended
Lipid Levels in NHANES 2003-2004
80
70
60
50
Men
Women
CVD
DM
Percent of
40
Adults
30
20
10
0
LDL-C
HDL-C
TG
Ghandehari and Wong et al, Am Heart J 2008
All
Genetic Causes of Dyslipidemia
Type I – Familial Hyperchylomicronemia
Fasting triglycerides > 1000 mg/dl
Defect in lipoprotein lipase or apo CII
Not necessarily at increased risk of CAD
Type II - Familial Hypercholesterolemia (type II)
LDL-C > 95th percentile for age and gender
CAD in men by 3rd or 4th decade
Defect in LDL receptor
Autosomal dominant inheritance
Prevalence 1:500
Familial Defective apo B 100
Defective apo B alters LDLr handling
Previously undetecable from FH
Genetic Causes of Dyslipidemia
Type III – Hyperlipoproteinemia
Increased TC, VLDL, decreased HDL; Increased VLDL:TG
Defect in apo E results in increased concentration of remnant particles
Rare
Type IV – Familial Hypertriglyceridemia
Increased TC (due to VLDL), TG, decreased LDL, HDL
Results from hepatic overproduction of VLDL
Prevalence 1:100 – 1:50; Association with CAD not as strong as FH
Heterogeneous inheritance
Very sensitive to diet and EtOH
Type V
Increase in chylomicrons and VLDL
Rare
Genetic Causes of Dyslipidemia
Familial Combined Hyperlipidemia
Increased TC, LDL and/or triglycerides; decreased HDL
Most common genetic dyslipidemia: prevalence 1:50
Heterogenous inheritance
Accounts for 10-20% of patients with premature CAD
Defects in HDL Metabolism
Most often low HDL is secondary to other dyslipidemia
Not all associated with increased CAD risk (e.g. apo AIMilano)
Tangier’s Disease
CETP defects result in increased HDL
Total Cholesterol Distribution:
CHD vs Non-CHD Population
Framingham Heart Study—26-Year Follow-up
No CHD
35% of CHD
Occurs in
People with
TC<200 mg/dL
150
CHD
200
250
300
Total Cholesterol (mg/dL)
Castelli WP. Atherosclerosis. 1996;124(suppl):S1-S9.
1996 Reprinted with permission from Elsevier Science.
14-y incidence
rates (%) for CHD
Low HDL-C Levels Increase CHD Risk Even
When Total-C Is Normal
14
12
10
8
6
4
2
0
< 40 40–49 50–59 60
HDL-C (mg/dL)
260
230–259
200–229
< 200
Risk of CHD by HDL-C and Total-C levels; aged 48–83 y
Castelli WP et al. JAMA 1986;256:2835–2838
Why is HDL the New Frontier?
Multiple Beneficial Properties of HDL
1. Reverse cholesterol transport
2. Anti-oxidant
3. Inhibit vascular inflammation:
Adhesion molecules and monocyte infiltration
4. Anti-thrombotic / profibrinolytic:
Increase fibrinolysis; decrease platelet aggregation
5. Endothelial stabilization
Apo A-I, major protein of HDL is the major player in all
these properties. It is the vehicle for cholesterol
removal. Thus, current concepts dictate that HDL
therapy should be Apo A-I based rather than HDL
Kashyap et al 2008
Cholesterol based.
Groups
Duration of follow-up
CHD Cases
≥10 years
<10 years
CHD Risk Ratio* (95% CI)
5902
4256
Sex
N=262,525
Male
Female
7728
1994
Fasting status
Fasting
Nonfasting
7484
2674
Adjusted for HDL
Yes
No
4469
5689
1.72 (1.56–1.90)
Overall CHD Risk Ratioa
Decreased Risk
aIndividuals
1
Increased Risk
2
in top versus bottom third of usual log-triglyceride values, adjusted for
at least age, sex, smoking status, lipid concentrations, and blood pressure (most)
CHD=coronary heart disease
Sarwar N, et al. Circulation. 2007;115:450-458.
HDL=high-density lipoprotein
Triglyceride-rich lipoproteins carry cholesterol and promote
atherosclerosis*
Very–low-density lipoprotein (VLDL) is precursor to low-density
lipoprotein (LDL)
Hypertriglyceridemia (HTG) drives
Cholesterol esters enrichment of VLDL (more atherogenic)
↓ LDL size (small, dense LDL are more atherogenic)*
↓ LDL-C (small, dense LDL carry less cholesterol)*
↓ High-density lipoprotein (HDL) size (small, dense HDL are unstable)
HTG is linked to other proatherogenic states*
Insulin resistance
Proinflammatory state
Prothrombotic state
Prooxidative state
Endothelial dysfunction
*Reasons why non–HDL-C is stronger than LDL-C as predictor of cardiovascular disease
More Particles
Fewer Particles
LDL=
130 mg/dL
Apolipoprotein
B
More
apolipoprotein B
Cholesterol
ester
Correlates with:
TC
198 mg/dL
LDL-C
130 mg/dL
TG
90 mg/dL
HDL-C
50 mg/dL
Correlates with:
TC
210 mg/dL
LDL-C
130 mg/dL
TG
250 mg/dL
HDL-C
30 mg/dL
Non–HDL-C 148 mg/dL
Non–HDL-C 180 mg/dL
Otvos JD, et al. Am J Cardiol. 2002;90:22i-29i.
TC=total cholesterol, LDL-C=low-density lipoprotein cholesterol,
TG=triglycerides, HDL-C=high-density lipoprotein cholesterol
Cholesterol per particle, BUT
Subendothelial penetration
Subendothelial binding
Oxidized/modified
LDL-receptor clearance
LDL=low-density lipoprotein
Non-HDL-Cholesterol and CVD Risk
Significance of Non-HDL-C
LDL-C levels incompletely measure the total
atherogenic burden
When serum TG are >200 mg/dL, increased remnant
atherogenic lipoproteins heighten risk beyond predicted
by LDL-C
– Associated with substantially elevated VLDL-C
VLDL-C and IDL-C are not accounted for by the
calculation of LDL-C
Non-HDL-C = cholesterol concentration of all
atherogenic lipoproteins
Miller M, et al. Am J Cardiol 2009;101:1003-1008
Atherogenic Lipoproteins
Non-HDL; Apo B-100—containing
Very–low-density lipoprotein (VLDL)
VLDL
IDL
LDL
Made in the liver
Triglycerides (TG) >> cholesterol esters (CE)
Carries lipids from the liver to peripheral tissues
Intermediate-density lipoprotein (IDL)
• Formed from VLDL due to lipase removal of TG
• Also known as a VLDL remnant
Low-density lipoprotein (LDL)
• Formed from IDL due to lipase removal of TG
• CE >> TG
Lp(a)
Lipoprotein (a)
• Formed from LDL w/addition of apolipoprotein A
HDL
High-density lipoprotein (HDL)
• Removes cholesterol from peripheral tissues
• Atherogenic and prothrombotic
The Framingham Study
Within non–HDL-C levels, no
Liu J, et al. Am J Cardiol. 2006;98:1363-1368.
2.5
Relative CHD Risk
association was found
between LDL-C and the risk
for CHD
In contrast, a strong positive
and graded association
between
non–HDL-C and risk for CHD
occurred within every level of
LDL-C
Non–HDL-C is a stronger
predictor of CHD risk than
LDL-C
2
1.5
1
0.5
0
<130
130–159
LDL-C,
mg/dL
≥160
≥190
160–189
<160
Non–HDL-C,
mg/dL
CHD=coronary heart disease, HDL-C=high-density lipoprotein
cholesterol, LDL-C=low-density lipoprotein cholesterol
Lp(a) in Atherogenesis: Another Culprit?
Identical to LDL particle except for addition of apo(a)
Plasma concentration predictive of atherosclerotic
disease in many epidemiologic studies, although
not all
Accumulates in atherosclerotic plaque
Binds apo B-containing lipoproteins and proteoglycans
Taken up by foam cell precursors
May interfere with thrombolysis
Maher VMG et al. JAMA. 1995;274:1771-1774.
Stein JH, Rosenson RS. Arch Intern Med. 1997;157:1170-1176.
Lp(a): An Independent CHD Risk Factor in Men of the
Framingham Offspring Cohort
10
5
2
RR
2.7
1.9
1.8
1.8
1.2
1
0.5
3.6
Lp(a)
TC
HDL-C
HT
0.2
0.1
RR=relative risk; HT=hypertension; GI=glucose intolerance.
Bostom AG et al. JAMA. 1996;276:544-548.
GI
Smoking
Placebo - Statin outcome trials
Continuum
of risk
Placebo MI rate per 100 subjects per 5 years
53.7
End stage
CORONA
GISSI-HF Heart failure
(rosuvastatin)
22.6 Secondary
prevention
4S
(simvastatin)
HPS
(simvastatin)
12.9
CARE
(pravastatin)
LIPID
8.44
7.9
2.8
High-risk CHD patients
(high cholesterol)
Majority of
CHD patients
(broad range of
cholesterol levels)
(pravastatin)
PROSPER
(pravastatin)
Primary
prevention
WOSCOPS
(pravastatin)
AFCAPS/TexCAPS
(lovastatin)
JUPITER
(rosuvastatin)
Patients at high risk
of CHD (high
cholesterol)
Patients at low
risk of CHD
(low HDL-C)
LDL cholesterol and benefit in clinical trials
Is lower better ?
30
4S - Placebo
25
Rx - Statin therapy
PRA – pravastatin
ATV - atorvastatin
Secondary Prevention
4S - Rx
20
15
LIPID - Placebo
CARE - Placebo
LIPID - Rx
CARE - Rx
Primary Prevention
HPS - Rx
TNT – ATV10 HPS - Placebo
PROVE-IT - PRA
WOSCOPS – Placebo
TNT – ATV80
PROVE-IT – ATV
AFCAPS - Placebo
TNT
10
5
JUPITER
6
AFCAPS - Rx
WOSCOPS - Rx
ASCOT - Placebo
ASCOT - Rx
0
40
(1.0)
60
(1.6)
80
100
120
140
(2.1)
(2.6)
(3.1)
(3.6)
LDL-C achieved mg/dL (mmol/L)
Adapted from Rosensen RS. Exp Opin Emerg Drugs 2004;9(2):269-279
LaRosa JC et al. N Engl J Med 2005;352:e-version
160
(4.1)
180
(4.7)
200
(5.2)
Cholesterol Treatment Trialists’ (CCT) Collaboration:
Efficacy and safety of cholesterol-lowering treatment:
prospective meta-analysis fo data from 90,056
participants in 14 randomized trials of statins
(The Lancet 9/27/05)
Over average 5 year treatment period (per mmol/L
reduction—approx 40 mg/dl in LDL-C):
12% reduction in all-cause mortality
19% reduction in coronary mortality
23% reduction in MI or CHD death
17% reduction in stroke
21% reduction in major vascular events
No difference in cancer incidence (RR=1.00).
Statin therapy can safely reduce 5-year incidence of major
coronary events, revascularization, and stroke by about
20% per mmol/L (about 38 mg/dl) reduction in LDL-C
HPS: First Major Coronary Event
StatinPlaceboType of Major
Allocated Allocated
Vascular Event (n = 10269) (n = 10267)
Coronary events
Nonfatal MI
357 (3.5%)
574 (5.6%)
Coronary death
587 (5.7%)
707 (6.9%)
Subtotal: MCE
898 (8.7%)
1212 (11.8%)
Statin Better
0.73 (0.670.79)
P < 0.0001
Revascularizations
Coronary
513 (5.0%)
725 (7.1%)
Noncoronary
450 (4.4%)
532 (5.2%)
Subtotal: any RV
939 (9.1%)
1205 (11.7%)
Any MVE
0.76 (0.700.83)
P < 0.0001
0.76 (0.720.81)
P < 0.0001
2033 (19.8%) 2585 (25.2%)
0.4
Placebo Better
0.6
0.8
Heart Protection Study Collaborative Group. Lancet. 2002;360:722.
1.0
1.2
1.4
HPS—Simvastatin:
Vascular Events by Baseline LDL-C
Baseline
LDL-C (mg/dL)
Statin
(n = 10,269)
Placebo
(n = 10,267)
<100
282 (16.4%)
358 (21.0%)
100–129
668 (18.9%)
871 (24.7%)
1083 (21.6%)
1356 (26.9%)
130
All patients
2033 (19.8%)
2585 (25.2%)
Event Rate Ratio (95% CI)
Statin Better Statin Worse
0.76 (0.72–0.81)
P < 0.0001
0.4 0.6 0.8 1.0 1.2 1.4
www.hpsinfo.org
HMG-CoA Reductase Inhibitor:
Secondary Prevention
Pravastatin or Atorvastatin Evaluation and Infection
Therapy (PROVE-IT)—TIMI 22 Study
4,162 patients with an ACS randomized to atorvastatin (80 mg) or pravastatin (40
mg) for 24 months
Recurrent MI or
Cardiac Death
30
Atorvastatin
Pravastatin
25
16% RRR
20
15
10
5
P =0.005
0
3
6
9
12
15
18
21
24
27
30
Follow-up (months)
ACS=Acute coronary syndrome, CV=Cardiovascular, MI=Myocardial infarction, RRR=Relative risk
reduction
Cannon CP et al. NEJM 2004;350:1495-1504
TNT: Rationale
Patients With CHD Events (%)
30
25
TNT
20
15
10
5
Screening
?
Atorvastatin 10 mg
Atorvastatin 80 mg
0
60
(1.6)
80
(2.1)
100
(2.6)
120
(3.1)
140
(3.6)
160
(4.1)
LDL-C, mg/dL (mmol/L)
Adapted from LaRosa et al. N Engl J Med. 2005:352:1425-1435.
180
(4.7)
200
(5.2)
TNT: Changes in LDL-C by
Treatment Group
160
Baseline
Atorvastatin 10 mg (n=5006)
3.5
120
Mean LDL-C level = 101 mg/dL (2.6 mmol/L)
100
3.0
2.5
80
2.0
60
P<.001
Mean LDL-C level = 77 mg/dL (2.0 mmol/L)
1.5
40
1.0
20
0.5
0
0
Screen 0 3
12
24
36
48
Study Visit (Months)
LaRosa et al. N Engl J Med. 2005;352:1425-1435.
60
Final
Mean LDL-C (mmol/L)
Mean LDL-C (mg/dL)
4.0
Atorvastatin 80 mg (n=4995)
140
Proportion of Patients Experiencing
Major Cardiovascular Event
TNT: Primary Efficacy Outcome Measure: Major
Cardiovascular Events*
0.15
Atorvastatin 10 mg
Atorvastatin 80 mg
Relative
risk
reduction
22%
Mean LDL-C level = 101 mg/dL
0.10
0.05
Mean LDL-C level = 77 mg/dL
HR=0.78 (95% CI 0.69, 0.89); P<.001
0
0
1
2
3
Time (Years)
4
5
* CHD death, nonfatal non–procedure-related MI, resuscitated cardiac arrest,
fatal or nonfatal stroke.
LaRosa et al. N Engl J Med. 2005;352:1425-1430.
6
Meta analysis of moderate vs aggressive statin
therapy
Coronary death or MI
ACS
Stable CHD
Cannon et al (2006) JACC 48:438
Recent Coronary IVUS
Progression Trials
Relationship between LDL-C and Progression Rate
Median change in percent
atheroma volume (%)
1.8
CAMELOT
placebo
1.2
0.6
REVERSAL
atorvastatin
0
-0.6
REVERSAL
pravastatin
ACTIVATE
placebo
A-Plus
placebo
ASTEROID
rosuvastatin
-1.2
50
60
70
80
90
100
110
120
Mean LDL-C (mg/dL)
Nissen SE, Nicholls S et al. JAMA 2006;295:1555–1565
ASTEROID: Study Design
Patients (≥18 years)
CAD, undergoing coronary
angiography
Target coronary artery: ≤50%
reduction in lumen diameter of
≥40 mm segment
Rosuvastatin 40 mg (n=349 for IVUS analysis;
n=292 for QCA analysis)
Target segment for QCA: all
segments >25% at baseline
No cholesterol entry criteria
Visit:
Week:
2
0
1
–6
IVUS
QCA
Lipids
Eligibility
assessment
Lipids
3
13
4
26
5
39
6
52
7
65
8
78
9
91
10
104
Lipids Tolerability
Lipids
Tolerability Tolerability IVUS
QCA
Tolerability
Tolerability
Lipids
Tolerability
End Point Analysis:
Change in Key IVUS Parameters
Change from baseline (%)
Median atheroma volume in the
most diseased 10-mm
subsegment
0
-1
-2
-3
-4
-5
-6
-7
-8
-9
-10
n=319
Median normalized TAV
n=346
- 6.8%
*
- 9.1%
*
*P<0.001 for difference from baseline. Wilcoxon signed rank test
Adapted from Nissen et al. JAMA 2006;295(13):1556-65.
Example of Regression of Atherosclerosis with
Rosuvastatin in ASTEROID (measured by IVUS)
Sipahi I, Nicholls S, Tuzcu E,
Nissen S. Interpreting the
ASTEROID trial: Coronary
atherosclerosis can regress with
very intensive statin therapy.
Cleve Clin J Med, 2006; 73:937944.
Reprinted with
permission. Copyright
2006. Cleveland Clinic
Foundation. All rights reserved.
Diabetes Mellitus:
Effect of an HMG-CoA Reductase Inhibitor
Meta-analysis of 18,686 patients with DM randomized to treatment
with a HMG-CoA Reductase Inhibitor
A statin reduces adverse CV events in diabetics
Cholesterol Treatment Trialists’ (CTT) Collaborators. Lancet 2008;37:117-25
Residual Cardiovascular Risk
in Major Statin Trials
Patients Experiencing
Major Coronary Events, %
100
75%
80
75%
73%
69%
62%
62%
60
40
20
0
4S
LIPID
CARE
HPS
WOS
AFCAPS /
TexCAPS
N
4444
9014
4159
20 536
6595
6605
LDL
-35%
-25%
-28%
-29%
-26%
-25%
Secondary
High Risk
Primary
Adapted from Libby PJ, et al. J Am Coll Cardiol, 2005:46:1225-1228.
Statin Monotherapy vs Combination Rx
0%
-10%
-20%
-30%
-24% -25%
-31%
-34%
-34% -35%
-36%
-40%
-50%
-60%
-70%
-80%
-80%
-90%
-90%
-100%
-95%
Reduction in CV Events
Brown BG et al NEJM 1999; 323:1289-98
Brown BG et al. NEJM 2001;345(22):1583-92
Brown BG. Circulation Suppl 1997
WOSCOPS Prava
4S Simva
CARE Prava
HPS Simva
PostCABG Lova
AFCAPS Lova
ASCOT Atorva
FATS
HATS
FATS 10 YR F/U
HATS: Percent Change in Stenosis
4.5
4.0
Change (%)
3.5
3.0
2.5
2.0
1.5
1.0
0.5
0.0
-0.5
-1.0
Placebo
Antioxidant
Vitamins*
Simvastatin/
Niacin†
*P = 0.16 for comparison with placebo; †P < 0.001; ‡P = 0.004.
HATS = HDL-Atherosclerosis Treatment Study.
Adapted from Brown BG et al. N Engl J Med. 2001;345:1583-1592.
Simvastatin /
Niacin/
Antioxidants‡
Patients Free of Events (%)
HATS: Patients Free of Events
Simvastatin-niacin
100
97%
90
All placebos
80
76%
RR = 0.10
P = 0.03
70
0
0
1
2
Years
HATS = HDL-Atherosclerosis Treatment Study.
Adapted from Brown BG et al. N Engl J Med. 2001;345:1583-1592.
3
Change in % stenosis
per year
Change in Percent Diameter Stenosis
vs On-treatment HDL-C in QCA Trials
CCAIT
1.4
1.2
PLAC I
MARS
1
MAAS
CCAIT
0.8
PLAC I
0.6
0.4
MAAS
0.2
0
-0.2
-0.4
-0.6
-0.8
-1
40
45
LCAS
Placebo
Statin*
MARS
LCAS
ASTEROID
50
On-treatment HDL-C (mg/dL)
*ASTEROID
rosuvastatin
MARS lovastatin
MAAS simvastatin
LCAS fluvastatin
CCAIT lovastatin
PLAC I pravastatin
Ballantyne CM, Nicholls S et al. Circulation 2008; Online
Fibrate Evidence:
Primary Prevention
Fenofibrate Intervention and Event Lowering in
Diabetes (FIELD)
9,795 diabetic patients randomized to fenofibrate (200 mg) or placebo
for 5 years
11% RRR
CHD Death or
Nonfatal MI (%)
9
6
5.9
5.2
3
0
P=0.16
Placebo
Fenofibrate
A fibrate does not provide significant additional benefit* in diabetics
CHD=Coronary heart disease, MI=Myocardial
infarction, RRR=Relative risk reduction
*Unadjusted for concomitant statin use
Source: Keech A et al. Lancet 2005;366:1849-61
ACCORD Lipid Study Results
(NEJM 2010; 362: 1563-74)
5518 patients with type 2 DM treated with open
label simvastatin randomly assigned to
fenofibrate or placebo and followed for 4.7
years.
Annual rate of primary outcome of nonfatal MI,
stroke or CVD death 2.2% in fenofibrate group
vs. 1.6% in placebo group (HR=0.91, p=0.33).
Pre-specified subgroup analyses showed
possible benefit in men vs. women and those
with high triglycerides and low HDL-C.
Results support statin therapy alone to reduce
CVD risk in high risk type 2 DM patients.
Fibrate Evidence:
Primary and Secondary Prevention
Action to Control Cardiovascular Risk in Diabetes
(ACCORD) Lipid Trial
5,518 diabetic patients on statin therapy randomized to fenofibrate
(160 mg) or placebo for 4.7 years
8% RRR
CV death, nonfatal
stroke or nonfatal
MI (%/year)
3
2.4
2.2
2
1
0
P=0.32
Placebo
Fenofibrate
On a background of statin therapy, a fibrate does not reduce CV events
in diabetics
CV=Cardiovascular, MI=Myocardial infarction,
RRR=Relative risk reduction
Source: ACCORD study group. NEJM 2010;Epub ahead of print
AIM-HIGH NEJM 11/15/2011
Objective
To determine whether the residual risk associated
with low levels of HDL-C in patients with
established CHD whose LDL-C therapy was
optimized with statins ± ezetimibe would be
mitigated with extended-release niacin vs. placebo
during long-term follow-up
Entry Criteria
Patients Age ≥ 45 Years with
Coronary Heart Disease (CHD), or
Cerebrovascular Disease (CVD), or
Peripheral Arterial Disease (PAD)
And Dyslipidemia
Low Levels of Baseline HDL-C
<40 mg/dL for men; < 50 mg/dL for women;
Triglycerides 150-400 mg/dL;
LDL-C < 180 mg/dL
Study Design
Open-Label Run-In:
Up-Titrate Niacin
from 500mg to
2,000mg/day
Adjust simva to
LDL 40 – 80 mg/dL
ER Niacin + 40-80 mg/day
simvastatin
4-8 weeks
R
Placebo + 40-80 mg/day
simvastatin
-2
-1
0
1
2
3
6
Months Relative to Randomization
Follow
to end
of
study
12
Endpoints
Primary Outcome Composite (Time to
First
Occurrence):
Coronary Heart Disease Death
Non-Fatal MI
Ischemic (Non-Hemorrhagic) Stroke
Hospitalization for ACS
Symptom-Driven Revascularization
Secondary Composite Endpoints:
CHD Death, Non-Fatal MI, Ischemic Stroke, or
Hospitalization for High-Risk ACS
CHD Death, Non-Fatal MI or Ischemic Stroke
Cardiovascular Mortality
Selected Baseline Characteristics
Number randomized
Mean (SD) age
Male
Caucasian
Current smokers
History of Hypertension
History of Diabetes
Metabolic Syndrome
History of MI
History of Cerebrovascular
Disease
3,414
64±9
85%
92%
20%
71%
34%
81%
56%
21%
All baseline characteristics balanced between treatment groups
Concomitant Medications at Entry
On a Statin
Duration of Statin Therapy*
94%
≥ 1 year
≥ 5 years
Prior Niacin Use
76%
40%
20%
ASA/Antiplatelet Therapy
Βeta-Blocker
ACEI / ARB
98%
80%
74%
Use of all secondary prevention therapies was
well-balanced between treatment groups
*Duration of statin therapy not ascertained in 6%
Baseline Lipids (mg/dL)
LDL-C (mean)
HDL-C (mean)
Triglycerides
On Statin
(n=3,196)
Off Statin
(n=218)
71
35
161
1259
33
215
107
81
165
111
(median)
Non-HDL (mean)
Apo-B
(mean)
HDL-C at Baseline & Follow-up
55
Combination Therapy
Monotherapy
50
mg/dL
45
P < 0.001
*
*
*
Year 1
Year 2
Year 3
40
35
30
25
Baseline
LDL-C at Baseline & Follow-up
80
Combination Therapy
75
Monotherapy
mg/dL
70
65
*
60
P < 0.001
55
50
Baseline
Year 1
Year 2
Year 3
Primary & Secondary Endpoints
Hazard
Ratio
95% CI
1.02
0.87, 1.21
CHD Death, MI,
Ischemic Stroke,
High-Risk ACS
1.08
0.87, 1.34
CHD Death, MI,
Ischemic Stroke
1.13
0.90, 1.42
Cardiovascular
Death
1.17
0.76, 1.80
Primary Endpoint
Secondary Endpoints
Cumulative % with Primary Outcome
Primary Outcome
50
Combination Therapy
Monotherapy
40
30
20
HR 1.02, 95% CI 0.87, 1,21
Log-rank P value= 0.79
16.4%
16.2%
10
0
0
N at risk
Monotherapy 1696
Combination Therapy 1718
1
1581
1606
2
3
Time (years)
1381
1366
910
903
4
436
428
Interpretation of Study Findings
and Therapeutic Implications
Contemporary optimal medical therapy and
aggressive secondary prevention (particularly
with intensive LDL-C lowering therapy) may
make it increasingly difficult to demonstrate
incremental treatment superiority
Previous therapy in patients receiving statins
(94%) and niacin (20%) may have limited our
ability to demonstrate a favorable treatment
effect with niacin
The unexpected 9.8% increase in HDL-C in
placebo-treated patients could have minimized
between-group event rate differences
Interpretation of Study Findings
and Therapeutic Implications
? Intensive use of statin therapy for ≥1 year in ~
75% of patients may have caused “delipidation” of
lipid-rich necrotic cores, converting high-risk
vulnerable plaques → stable, quiescent plaques
Residual risk in AIM-HIGH patients during followup was appreciable (5.4% event rate/year), but
was not mitigated by niacin
Whether niacin benefit might have been discerned
during a longer follow-up remains uncertain
Conclusions
Among patients with stable, non-acute,
cardiovascular disease and LDL-C levels of <70
mg/dL, there was no incremental clinical benefit
from the addition of niacin to statin therapy during
a 36-month follow-up, despite significant
improvements in HDL-C and triglycerides
AIM-HIGH reaffirms current NCEP ATP-III
treatment guidelines for LDL-C lowering as the
principal target of lipid treatment
Additional analyses will be required to determine
if certain subsets of patients with low HDL-C in
AIM-HIGH may benefit from niacin treatment
HDL regulation through CETP inhibition
Cys 13 – dalcetrapib binding site
Lipid tunnel
Anacetrapib (MSD)
CETP crystal structure
Dalcetrapib (Roche)
Dalcetrapib
Torcetrapib
Anacetrapib
9000 nmo/l
50 nmol/l
57 nmol/l
CETP inhibition
37.2%
≥80%
90%
HDL-C increase
33.9%
91%
129%
Blood pressure increase
No
Yes
No
Increases aldosterone
production (in vitro)
No
Yes
No
IC50
Qui et al (2007) Nat Struct Mol Biol 14;106-112, Ranaletta et al (2010) J Lipid Res on line, Okamoto et al. Nature. 2000;406:203–207, Clark et al. J Lipid Res.
2006;47:537–552, Masson D. Curr Opin Invest Drugs. 2009;10:980-987, Grooth et al. Circulation. 2002;105:2159–2165, Clark et al. Arterioscler Thromb Vasc
Biol. 2004;24:490–497; Krishna et al. Lancet. 2007;370:1907-1914, Stein et al. Am J Cardiol. 2009;104:82–91, Barter et al. N Engl J Med. 2007;357:2109–2122,
Torcetrapib and Atherosclerosis
Radiance 1 and Illuminate studies
Torcetrapib raises HDLc 54%,
Lowers LDLc by 15% but:Lack of impact on carotid IMT
Increased risk of coronary event
Barter et al (2007) NEJM 356;2109-22
Kastelein et al (2007) NEJM 356;1620-30
Dal-VESSEL and Dal-Plaque
Dal-Vessel (ESC 2011) recently reported 600 mg
dalcetrapib to increase HDL 31% relative to placebo,
but no improvement (or worsening) in FMD.
Dal-Plaque (Lancet, 9/13/11) showed in 130 pts with
CAD or high risk dalcetrapib 600 mg vs. placebo to
also raise HDL-C 31% and regression in MRI
assessed plaque of 4mm2 relative to placebo, as well
as reduced uptake of 18F-FDG suggesting an antiinflammatory effect.
dal-OUTCOMES Study design
● Objective: To evaluate the potential of dalcetrapib to reduce cardiovascular morbidity and mortality in patients who are
clinically stable after recent ACS and to evaluate the long term safety profile of dalcetrapib
● A double-blind, randomized, placebo-controlled, parallel-group multicenter outcomes study in 15,600 patients with stable
CHD after recent ACS
Pre-randomization
phase
Double-blind
Until 1600 events occur
but at least a minimum
of
2 years
dalcetrapib 600 mg
Single-blind
placebo run-in
4–12 Weeks
placebo
background of standard medication for ACS
(including aspirin, antihypertensives and statins)
Visit 1
Visit 2
Visit 3
Randomization
Schwartz et al. Am Heart J. 2009;158:896-901.
Follow up 1st year:
every 3 months Following years: every 4 months
At least 2 years;
at least 80% of patients followed for 2.5
years
Lp-PLA2 and vascular disease
LpPLA2 Studies Collaboration (2010) Lancet 375; 1536-154
Novel anti-atherosclerotic agents
Darapladib in animal models and clinical trials
STABILITY Stabilization of
Effects of Lp-PLA2 inhibition by darapladibAtherosclerotic Plaque by Initiation
in diabetic, hypercholesterolemic pigs of Darapladib Therapy
Estimated enrolment 15,500
• Darapladib vs placebo in well
treated patients with CHD plus
other risk.
• 1ary endpoint major coronary
event
SOLID – TIMI52 Stabilization
Wilensky et al (2008) Nature Medicine (in press)
of plaques using darapladib.
• Incidence of major coronary
events in patients with ACS
•Darapladib 160 mg vs placebo
started within 30 days of index
ACS event.
NCEP ATP III: Evaluation—
Major Risk Factors for CAD
Age (men 45 y; women 55 y)
Cigarette smoking
Hypertension (BP 140/90 mm Hg or
antihypertensive medication)
HDL-C <40 mg/dL
Family history of premature CAD
<55 y in first-degree male relative
<65 y in first-degree female relative
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
Revised ATP III (AHA/NHLBI) Metabolic Syndrome
Definition 2005
Risk Factor
Abdominal obesity†
(Waist circumference‡)
Men
Women
TG
HDL-C
Men
Women
Blood pressure
Fasting glucose
Defining Level
>102 cm (>40 in)
>88 cm (>35 in)
150 mg/dL or Rx for ↑ TG
<40 mg/dL
<50 mg/dL or Rx for ↓ HDL
130/85 mm Hg or on HTN Rx
100 mg/dL or Rx for ↑ glucose
*Diagnosis is established when 3 of these risk factors are present.
†Abdominal obesity is more highly correlated with metabolic risk factors than is BMI.
‡Some men develop metabolic risk factors when circumference is only marginally
increased.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA. 2001;285:24862497; Updated AHA/NHLBI Statement Oct 18, 2005: Grundy et al. Circulation 2005; 112 (epub).
NCEP ATP III: Evaluation—
Need for Framingham Calculation
Risk Profile
10-Year Risk
for CAD
Need for
Framingham
Calculation
1 RF
<10%
No
0%-10%
Yes
10%-20%
Yes
>20%
No
2 RF
CAD or CAD risk
equivalent
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
NCEP ATP III: Evaluation—
CAD Risk Equivalents
Diabetes
Atherosclerotic disease
Peripheral artery disease
Abdominal aortic aneurysm
Symptomatic carotid artery disease
CAD 10-year risk >20%
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
ATP III Framingham Risk Scoring
Assessing CHD Risk in Men
Step 1: Age
Years
20-34
35-39
40-44
45-49
50-54
55-59
60-64
65-69
70-74
75-79
Step 4: Systolic Blood Pressure
Points
-9
-4
0
3
6
8
10
11
12
13
Step 2: Total Cholesterol
TC
Points at
at Points at
(mg/dL)
Age 20-39
70-79
<160
0
160-199
4
200-239
7
240-279
9
280
11
Step 3: HDL-Cholesterol
HDL-C
(mg/dL)
60
Points
-1
50-59
0
40-49
1
<40
2
Systolic BP
(mm Hg)
<120
120-129
130-139
140-159
160
Points at
Points
Points
if Untreated if Treated
0
0
0
1
1
2
1
2
2
3
Points at
Points
Age 40-49 Age 50-59 Age 60-69 Age
0
3
5
6
8
0
2
3
4
5
0
1
1
2
3
0
0
0
1
1
Step 5: Smoking Status
at
70-79
Nonsmoker
Smoker
Points at
Points at
Age 20-39
0
8
Step 6: Adding Up the Points
Points at
Age
Total cholesterol
HDL-cholesterol
Systolic blood pressure
Smoking status
Point total
Step 7: CHD Risk
Point Total 10-Year Risk
Risk
<0
<1%
0
1%
1
1%
2
1%
3
1%
4
1%
5
2%
6
2%
7
3%
8
4%
9
5%
10
6%
Points at
Points
Point Total 10-Year
11
12
13
14
15
16
17
8%
10%
12%
16%
20%
25%
30%
Age 40-49 Age 50-59 Age 60-69 Age
0
5
0
3
0
1
0
1
Note: Risk estimates were derived from the experience of the Framingham Heart Study,
a predominantly Caucasian population in Massachusetts, USA.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486-2497.
© 2001, Professional Postgraduate Services®
www.lipidhealth.org
ATP III Framingham Risk Scoring
Assessing CHD Risk in Women
Step 1: Age
Years
20-34
35-39
40-44
45-49
50-54
55-59
60-64
65-69
70-74
75-79
Step 4: Systolic Blood Pressure
Points
-7
-3
0
3
6
8
10
12
14
16
Systolic BP
(mm Hg)
<120
120-129
130-139
140-159
160
Points
Points
if Untreated if Treated
0
0
1
3
2
4
3
5
4
6
HDL-C
(mg/dL)
60
Points
-1
50-59
0
40-49
1
<40
2
Age
Total cholesterol
HDL-cholesterol
Systolic blood pressure
Smoking status
Point total
Step 7: CHD Risk
Step 2: Total Cholesterol
TC
Points at
at Points at
(mg/dL)
Age 20-39
70-79
<160
0
160-199
4
200-239
8
240-279
11
13
Step 280
3: HDL-Cholesterol
Step 6: Adding Up the Points
Points at
Points at
Points
Age 40-49 Age 50-59 Age 60-69 Age
0
3
6
8
10
0
2
4
5
7
0
1
2
3
4
0
1
1
2
2
Step 5: Smoking Status
at
Points at
Points at
Age 20-39
70-79
Nonsmoker
0
Smoker
from
the experience9of
Points at
Point Total 10-Year Risk
Risk
<9
<1%
9
1%
10
1%
11
1%
12
1%
13
2%
14
2%
15
3%
16
4%
17
5%
18
6%
19
8%
Points at
Point Total 10-Year
20
21
22
23
24
25
11%
14%
17%
22%
27%
30%
Points
Age 40-49 Age 50-59 Age 60-69 Age
0
0
7
4
Note: Risk estimates were derived
the Framingham
Heart Study,
a predominantly Caucasian population in Massachusetts, USA.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486-2497.
0
2
0
1
© 2001, Professional Postgraduate Services®
www.lipidhealth.org
hs-CRP Adds to Predictive Value of TC:HDL Ratio in
Determining Risk of First MI
Relative Risk
5.0
4.0
3.0
2.0
1.0
0.0
High
Medium
High
Medium
Low
Total Cholesterol:HDL Ratio
Ridker et al, Circulation. 1998;97:2007–2011.
Low
JUPITER
Why Consider Statins for Low LDL, high hsCRP Patients?
AFCAPS/TexCAPS Low LDL Subgroups
LowLDL,
LDL,Low
LowhsCRP
hsCRP
Low
[A]
LowLDL,
LDL,High
HighhsCRP
hsCRP
Low
[B]
0.50.5
StatinEffective
Effective
Statin
1.01.0
RR
2.02.0
StatinNot
NotEffective
Effective
Statin
However, while intriguing and of potential public health importance, the
observation in AFCAPS/TexCAPS that statin therapy might be effective
among those with elevated hsCRP but low cholesterol was made on a
post hoc basis. Thus, a large-scale randomized trial of statin therapy was
needed to directly test this hypotheses.
Ridker et al, New Engl J Med 2001;344:1959-65
JUPITER
Trial Design
JUPITER
Multi-National Randomized Double Blind Placebo Controlled Trial of
Rosuvastatin in the Prevention of Cardiovascular Events
Among Individuals With Low LDL and Elevated hsCRP
Rosuvastatin 20 mg (N=8901)
No Prior CVD or DM
Men >50, Women >60
LDL <130 mg/dL
hsCRP >2 mg/L
4-week
run-in
Placebo (N=8901)
MI
Stroke
Unstable
Angina
CVD Death
CABG/PTCA
Argentina, Belgium, Brazil, Bulgaria, Canada, Chile, Colombia, Costa Rica,
Denmark, El Salvador, Estonia, Germany, Israel, Mexico, Netherlands,
Norway, Panama, Poland, Romania, Russia, South Africa, Switzerland,
United Kingdom, Uruguay, United States, Venezuela
Ridker et al, Circulation 2003;108:2292-2297.
JUPITER
Ridker et al NEJM 2008
Primary Trial Endpoint : MI, Stroke, UA/Revascularization, CV Death
0.08
HR 0.56, 95% CI 0.46-0.69
P < 0.00001
Placebo 251 / 8901
0.04
0.06
- 44 %
Rosuvastatin 142 / 8901
0.00
0.02
Cumulative Incidence
Number Needed to Treat (NNT5) = 25
0
1
2
4
Follow-up (years)
Number at Risk
Rosuvastatin
Placebo
3
8,901
8,901
8,631
8,621
8,412
8,353
6,540
6,508
3,893
3,872
1,958
1,963
1,353
1,333
983
955
544
534
157
174
UPITER population – high CRP (>2mg/l), low LD
Dual Target Analysis: LDL-C <70 mg/dL, hsCRP <2 mg/L
0.08
placebo HR 1.0
(referent)
Cumulative Incidence
P <0.0001
0.06
LDL >70 mg/dL
and / or
hsCRP >2 mg/L
HR 0.64 (0.49-0.84)
0.04
LDL <70 mg/dL
and hsCRP <2 mg/L
HR 0.35 (0.23-0.54)
0.02
0.00
0
Number at Risk
rosuvastatin
placebo
1
2
3
4
Follow-up (years)
7,716
7,832
7,699
7,806
7,678
7,777
6,040
6,114
3,608
3,656
1,812
1,863
1,254
1,263
913
905
508
507
145
168
Ridker PM et al. Lancet 2009;373:1175–1182
NCEP ATP III Guidelines: Treatment
Risk
Category
1 RF
2 RFs
CAD or
CAD risk
equivalent
LDL-C Level
LDL-C LDL-C Level
to Initiate
Goal
to Initiate Drug Therapy
(mg/dL) TLC (mg/dL)
(mg/dL)
<160
160
190
(10-year risk
0%-10%)
<130
130
160
(10-year risk
10%-20%)
<130
130
130
<100
100
130
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
Statins in ACS - Guidelines
• Who - Initiate therapy regardless of baseline LDL.
• When – Pre-discharge; but no difference in benefit
when initiated immediately or days post event (ESC
<4 days).
• What – Evidence base is for high dose statin (but
not 80mg simvastatin).
• Goal - <70 mg/dl (2.0 mmol/l) LDL cholesterol.
ACC/ AHA 2007 in JACC (2008) 51; 210-47
ESC 2007 in Eur Heart J (2007) 28; 1598-1660
Lipid Management Goal: Persons
with Pre-existing CHD
I IIa IIb III
LDL-C should be less than 100 mg/dL
I IIa IIb III
Further reduction to LDL-C to < 70 mg/dL is
reasonable
If TG >200 mg/dL, non-HDL-C should be < 130 mg/dL*
*Non-HDL-C = total cholesterol minus HDL-C
NCEP ATP III: Setting Goals—
Secondary–Non-HDL-C
(Patients With TG 200)
Risk Category
Non–HDL-C Goal (mg/dL)
1 RF
<190
2 RFs
(CAD risk 20%)
<160
CAD or
CAD risk equivalent
(CAD risk >20%)
<130
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
ATP III Classification of Other Lipoprotein Levels
Total Cholesterol
HDL-Cholesterol
Level (mg/dl)
Classification
Level (mg/dl)
Classification
<200
Desirable
>40
Minimum goal*
200-239
Borderline High
40-50
Desired goal*
>240
High
>50
High
Triglyceride
Level (mg/dl)
Classification
<150
Normal
150-199
Borderline High
200-499
High
>500
Very High
HDL=High density lipoprotein
*These goals apply to men. For women, the minimum goal is >50 mg/dL
Source: Expert Panel on Detection, Evaluation, and Treatment of High Blood
Cholesterol in Adults. JAMA 2001;285:2486-97
NCEP ATP III Guidelines: Treatment
Therapeutic
Lifestyle Change (TLC)
Pharmacologic
Treatment
Improve diet
Statins (HMG-CoA
reductase inhibitors)
Weight reduction
Physical activity
Fibrates
Niacin
Bile acid sequestrants
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
Lipid Management
Recommendations
For all patients
I IIa IIb III
Start dietary therapy (<7% of total calories as saturated
fat and <200 mg/d cholesterol)
I IIa IIb III
I IIa IIb III
Adding plant stanol/sterols (2 gm/day) and viscous fiber
(>10 mg/day) will further lower LDL
Promote daily physical activity and weight
management.
Encourage increased consumption of omega-3 fatty
acids in fish or 1 g/day omega-3 fatty acids in capsule
form for risk reduction.
Therapeutic Lifestyle Changes
Nutrient Composition of TLC Diet
Nutrient
Recommended Intake
Saturated fat
Less than 7% of total calories
Polyunsaturated fat
Up to 10% of total calories
Monounsaturated fat
Up to 20% of total calories
Total fat
25–35% of total calories
Carbohydrate
50–60% of total calories
Fiber
20–30 grams per day
Protein
Approximately 15% of total calories
Cholesterol
Less than 200 mg/day
Total calories (energy)
Balance energy intake and expenditure
to maintain desirable body weight
Possible Benefits From Other Therapies
Therapy
Result
• Soluble fiber in diet (2–8 g/d)
(oat bran, fruit, and vegetables)
LDL-C 1% to 10%
• Soy protein (20–30 g/d)
LDL-C 5% to 7%
• Stanol esters (1.5–4 g/d)
(inhibit cholesterol absorption)
LDL-C 10% to 15%
• Fish oils (3–9 g/d)
(n-3 fatty acids)
Triglycerides 25% to 35%
Jones PJ. Curr Atheroscler Rep. 1999;1:230-235.
Lichtenstein AH. Curr Atheroscler Rep. 1999;1:210-214.
Rambjor GS et al. Lipids. 1996;31:S45-S49.
Ripsin CM et al. JAMA. 1992;267:3317-3325.
Dietary Adjuncts
TLC for patients with LDL-C = 160
Dietary Component
Low saturated fat/dietary cholesterol
Viscous fiber (10–25 g/d)
Plant stanols/sterols (2 g/d)
Total
LDL-C (mg/dL)
–12
–8
–16
–36 mg/dl
Walden CE et al. Arterioscler Thromb Vasc Biol 1997;17:375-382.
Jenkins DJ et al. Curr Opin Lipidol 2000;11:49-56.
Cato N. Stanol meta-analysis. Personal communication, 2000.
Moderate physical activity at least 30-60 minutes 5
days a week or longer will help to raise HDL-C, lower
total and LDL-C, lower TG, lower glucose, insulin,
and blood pressure levels.
Effect of Lipid-modifying Therapies
TC
LDL
HDL
TG
Patient
tolerability
Bile acid
sequestrants
7-10%
10-18%
3%
Neutral or
Poor
Nicotinic acid
10-20%
10-20%
14-35%
30-70%
Poor to
reasonable
Fibrates
(gemfibrozil)
19%
4-21%
11-13%
30%
Good
19-37%
25-50%
4-12%
14-29%
Good
13%
18%
1%
9%
Good
Therapy
Statins*
Ezetimibe
TC–total cholesterol, LDL–low density lipoprotein, HDL–high density lipoprotein,
TG–triglyceride. * Daily dose of 40mg of each drug, excluding rosuvastatin.
Questran® Prescribing Information, Colestid ® Prescribing Information, WelChol ® Prescribing
information, Niaspan ® Prescribing Information, Lopid ® Prescribing Information, TriCor ®
Prescribing Information, Lipitor ® Prescribing Information, Zocor ® Prescribing Information,
Mevaco ® r Prescribing Information, Lescol ® Prescribing Information, Pravacol ® Prescribing
Information; Zetia ® Prescribing Information.
When LDL-lowering drug therapy
is employed in high-risk or
moderately high risk patients,
intensity of therapy should be
sufficient to achieve a 30–40%
reduction in LDL-C levels.
Effect of Statin Therapy on LDL-C
Levels: “The Rule of 6”
Lovastatin 20/80
28
Pravastatin 20/40
27
Simvastatin 20/80
Highest
recommended dose
6
35
Fluvastatin 20/80
Starting dose LDL-C
12
19
12
12
Atorvastatin 10/80
37
0
10
20
18
30
40
Reduction of LDL Cholesterol (%)
Illingworth DR. Med Clin North Am. 2000;84:23-42.
50
60
Percentage Change From Baseline in
LDL-C at Week 6 by Dose (ITT)1,2
Mean Percent Change From
Baseline in LDL-C (SE)
Dose
0
10 mg
20 mg
40 mg
80 mg
Rosuvastatin
Atorvastatin
Simvastatin
Pravastatin
–10
–20
–30
–40
*
–50
**
†
–60
*P<.002 vs atorvastatin 10 mg; simvastatin 10 mg, 20 mg, 40 mg; pravastatin 10 mg, 20 mg, 40 mg
**P<.002 vs atorvastatin 20 mg, 40 mg; simvastatin 20 mg, 40 mg, 80 mg; pravastatin 20 mg, 40 mg
† P<.002 vs atorvastatin 40 mg; simvastatin 40 mg, 80 mg; pravastatin 40 mg
1.Jones PH, Davidson MH, Stein EA, et al. Am. J. Cardiology 2003; 93: 152-160.
2.Data on file, DA-CRS-02 AstraZeneca Pharmaceuticals LP, Wilmington, DE.
Doses of Statins Required to Attain
30-40% Reduction of LDL-C
Dose, mg/d
LDL Reduction,
%
Atorvastatin
10
39
Lovastatin
40
31
Pravastatin
40
34
Simvastatin
20-40
35-41
Fluvastatin
40-80
25-35
Rosuvastatin
5-10
39-45
HMG-CoA Reductase Inhibitor:
Adverse Effects
74,102 subjects in 35 randomized clinical trials with statins
• 1.4% incidence of elevated hepatic
transaminases (1.1% incidence in
control arm)
• Dose-dependent phenomenon that is
usually reversible
Hepatocyte
• 15.4% incidence of myalgias*
(18.7% incidence in control arm)
• 0.9% incidence of myositis (0.4%
incidence in control arm)
• 0.2% incidence of rhabdomyolysis
(0.1% incidence in control arm)
Skeletal myocyte
*The rate of myalgias leading to discontinuation of atorvastatin in the TNT
trial was 4.8% and 4.7% in the 80 mg and 10 mg arms, respectively.
Source: Kashani A et al. Circulation 2006;114:2788-97
HMG-CoA Reductase Inhibitor:
Adverse Effects
Risk Factors for the Development of Myopathy*
Concomitant Use of Meds
Other Conditions
Fibrate
Advanced age (especially >80 years)
Nicotinic acid (Rarely)
Women > Men especially at older age
Cyclosporine
Small body frame, frailty
Antifungal azoles**
Multisystem disease‡
Macrolide antibiotics†
Multiple medications
HIV protease inhibitors
Perioperative period
Nefazadone
Alcohol abuse
Verapamil, Amiodarone
Grapefruit juice (>1 quart/day)
*General term to describe diseases of muscles
**Itraconazole, Ketoconazole
†Erythromycin, Clarithromycin
‡Chronic renal insufficiency, especially from
diabetes mellitus
Source: Pasternak RC et al. Circulation
2002;106:1024-1028
Why combination therapy?
Few patients achieve LDL-C goal on
monotherapy
Uptitration of dosage is rare
LDL-C goals are getting more aggressive
High-dose statins increase risk of side effects
Can address mixed dyslipidemia (e.g., few pts
achieve adequate control of HDL-C and
triglycerides on monotherapy)
Options for Patients who Fail to Reach
LDL-C Goal on Statin Monotherapy
Addition of:
• Niacin
• Bile acid sequestrant
• Cholesterol absorption inhibitor
Pharmacologic Therapy: Niacin
Reduces HDL catabolism and VLDL production
Primarily used to treat low HDL-C (15%-35%)
and elevated TG (20%-50% )
LDL-C 5%-25%
Side effects
Hepatotoxicity, hyperglycemia, hyperuricemia,
upper GI distress, flushing, itching
Contraindicated in patients with liver disease,
gout, peptic ulcer
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
NIACIN: a broad-spectrum antidyslipidemic agent
Niacin Decreases
Niacin Increases
Total cholesterol
HDL cholesterol
Total triglycerides
HDL2 cholesterol
VLDL-C
HDL3 cholesterol (less than HDL2)
LDL-C
Apolipoproteins A-I, A-II
Small dense LDL
LP A-I
Lp(a)
LP A-I + A-II (less than LP A-I)
Apo B
Pre-beta HDL
Total cholesterol/HDL-C
LDL-C/HDL-C
LDL particle size
Apo B/A-I
Tavintharan S and Kashyap ML.2001,Current Atheroscler Reports 3:74
Nicotinic Acid Evidence:
Effect on Lipid Parameters
30%
Mean change from Baseline
30
15%
20
10
26%
–9%
-10
–14%
–5%
–17%
–11%
-30
–22%
–21%
LDL-C
–28%
-40
–35%
-50
Dose (mg)
HDL-C
10%
0
-20
22%
30%
–39%
500
1000
1500
2000
2500
–44%
TG
3000
HDL-C=High density lipoprotein cholesterol, LDL-C=Low
density lipoprotein cholesterol, TG=Triglyceride
Source: Goldberg A et al. Am J Cardiol 2000;85:1100-1105
Bile Acid Sequestrants
Major actions
Reduce LDL-C 15%-30%
Raise HDL-C 3%-5%
May increase TG
Side effects
GI distress/constipation
Decreased absorption of other drugs (1st generation)
Contraindications
Dysbetalipoproteinemia
Elevated TG (especially >400 mg/dL)
New Bile Acid Sequestrant:
Colesevelam
Lower dose for effect
Fewer GI complaints than with other bile
acid sequestrants
Reduces absorption of -carotene
Requires 4-6 tablets/day
Davidson et al. Expert Opin Investig Drugs. 2000;9:2663.
% Change from baseline
at wk 24
Colesevelam Monotherapy: Efficacy
15
LDL-C
10
10
†
5
0
TG
HDL-C
3
5
0
-1
-5
-10
-15
-20
-15
*
*P<0.001 vs placebo.
†P=0.04 vs placebo.
Insull et al. Mayo Clin Proc. 2001;76:971.
Placebo (n=88)
Colesevelam 3.8 g/d (n=95)
Pharmacologic Therapy: Fibrates
Inhibit hepatic TG production and increase HDL production
Used to treat elevated TG (20%-50% )
and low HDL-C (10%-20% )
Variable effect on LDL-C
Side effects
Dyspepsia, gallstones, myopathy
Increased with statins
Contraindicated in patients with severe renal or hepatic
disease
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults.
JAMA. 2001;285:2486.
Limitations of Current
Intestinal-Acting Agents
Bile acid sequestrants
Noncompliance
GI tolerability
Reduced absorption of lipid-soluble vitamins
May increase TG in patients with hypertriglyceridemia
Plant stanol and sterol esters
Lack of selectivity
Some patients may find difficult to incorporate into
diet
May reduce absorption of lipid-soluble vitamins
Ezetimibe —
Localizes at Brush Border of Small Intestine
Ezetimibe, a selective cholesterol absorption
inhibitor, localizes and appears to act at the
brush border of the small intestine and inhibits
cholesterol absorption
This results in
A decrease in the delivery of intestinal cholesterol to
the liver
A reduction of hepatic cholesterol stores and an
increase in clearance of cholesterol from the blood
Ezetimibe and Statins
Complementary Mechanisms
Ezetimibe reduces the delivery of cholesterol to the liver
Statins reduce cholesterol synthesis in the liver
The distinct mechanism of ezetimibe is complementary to
that of statins
The effects of ezetimibe, either alone or in addition to a
statin, on cardiovascular morbidity or mortality have not
been established
Knopp RH. N Engl J Med. 1999;341:498–511.
Coadministration:
Simvastatin + Ezetimibe
Placebo
(n = 11)
SIMVA 10 mg
(n = 12)
SIMVA 10+
EZE 10 mg
(n = 11)
Mean Percent Change in
LDL-C From Baseline
0
-10
-3.2
-20
-30
-34.9*
-40
-50
*P < 0.01 vs placebo
†P < 0.01 vs simvastatin 10 mg
-60
Stein, E. Eur Heart J. 2001;3(suppl E):E14.
17%
-51.9*†
w-3 Fatty Acids Evidence:
Effect on Lipid Parameters
27 patients with hypertriglyceridemia and low HDL-C treated
with w-3 fatty acid (4 grams/day) for 7 months
Triglyceride
% Reduction
0
Total
Cholesterol
-10
-20
-21*
-30
-40
-50
-46*
HDL-C=High-density lipoprotein cholesterol
*P<0.05
Source: Abe Y et al. Arterioscler Thromb Vasc Biol 1998;18:723-731
w-3 Fatty Acids Evidence:
Primary and Secondary Prevention
Japan Eicosapentaenoic acid Lipid Intervention
Study (JELIS)
18,645 patients with hypercholesterolemia randomized to EPA (1800 mg)
with a statin or a statin alone for 5 years
Years
w-3 fatty acids provide CV benefit, particularly in secondary prevention
CV=Cardiovascular, EPA=Eicosapentaenoic acid
*Composite of cardiac death, myocardial infarction, angina, PCI, or CABG
Source: Yokoyama M et al. Lancet. 2007;369:1090-8
w-3 Fatty Acids Evidence:
Secondary Prevention
Diet and Reinfarction Trial (DART)
All cause mortality (%)
2,033 men with a history of a MI randomized to a diet of reduced fat with an
increased ratio of polyunsaturated to saturated fat, increased fatty fish
intake*, or increased fiber intake for 2 years
8.0%
7.0%
6.0%
5.0%
w-3 Fatty Acids
4.0%
Placebo
3.0%
2.0%
1.0%
0.0%
w-3 fatty acids reduce all cause mortality** after a MI
EPA=Eicosapentaenoic acid, MI=Myocardial infarction
*Corresponds to 2.5 grams of EPA (PUFA)
**p<0.05
Source: Burr ML et al. Lancet 1989;2:757-761
w-3 Fatty Acids Evidence:
Secondary Prevention
Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto
miocardico (GISSI-Prevenzione)
Percent of patients
11,324 patients with a history of a MI randomized to w-3 polyunsaturated
fatty acids [PUFA] (1 gram), vitamin E (300 mg), both or none for 3.5 years
16
14
12
10
8
6
4
2
0
P=0.048
P=0.053
P=0.023
P=0.008
w-3 PUFA
Placebo
Death,
NF MI,
NF stroke
(2 way)
CV
death,
NF MI,
and NF
stroke
Death,
NF MI,
NF stroke
(4 way)
CV
death,
NF MI,
and NF
stroke
w-3 fatty acids provide significant CV benefit after a MI
CV=Cardiovascular, MI=Myocardial infarction, NF=Nonfatal, PUFA=Polyunsaturated fatty acids
Source: GISSI Investigators. Lancet 1999;354:447-455
w-3 Fatty Acids Evidence:
Secondary Prevention
OMEGA Trial
Rate of reinfarction,
stroke, or death* (%)
3,827 patients 3-14 days following a MI randomized to w-3 fatty acids (460
mg EPA + 380 mg DHA) or placebo for 1 year
12
10.4
8.8
8
4
0
P=0.10
Placebo
Fatty acids
w-3 fatty acids provide no benefit following a MI in those with high
utilization of risk reducing therapies
DHA=Docosahexaenoic acid, EPA=Eicosapentaenoic
acid, MI=Myocardial infarction
*This is a secondary endpoint
Source: Senges J et al. Presented at the Annual Scientific Sessions of the
American College of Cardiology, March 2009, Orlando, FL
CONCLUSIONS
Many persons with normal total or LDL-C levels still
suffer CHD events.
While statin-based clinical trials significantly reduce risk
of CHD, residual risk still exists.
Non-HDL-C, which reflects all the atherogenic lipid
fractions, appears to be a stronger predictor of CHD
events than LDL-C.
The measurement of non-HDL-C and its use as a
secondary therapeutic target is warranted to better
address residual CHD risk.
Lifestyle therapies as well as pharmacologic
approaches, particular combination therapy with statins
and other agents, are important for optimizing the entire
lipid profile.