OCULAR PHARMACOLOGY
advertisement

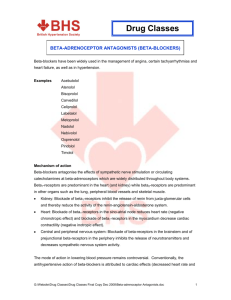
OCULAR PHARMACOLOGY for ASSISTANTS AND TECHNICIANS John W. Snead MD, MBA, FACS Lynn Lawrence, CPOT, ABOC ROLE of the ASSISTANT AND TECHNICIAN Recording Patient Education NEVER Work in Doubt! PATIENT CASE HISTORY General Health Medications Allergies VITAMIN SUPPLEMENTS CLASSIFICATIONS Solutions Suspensions Ointments DIAGNOSTIC AGENTS DPA’s treat symptoms, unknown disease Topical Anesthestics Mydriatics Cycloplegics Dyes/Stains Fluress Gonioscopic Solutions Topical Anesthetics Proparacaine Tetracaine Cocaine Alcaine Mydriatics & Cycloplegics Tropicamide Phenylephrine Cyclogyl Atropine Homatropine Scopalomine Dilation Hazards Cross Contamination Narrow anterior chamber angle Potential risk in dilating … opt vs oph Plan for acute angle glaucoma attack Make sure you are far enough away not to Touch the patient Dyes & Stains Fluorescein Rose Bengal Lissamine Green Fluress Gonioscopy Solutions Goniosol Gonioscopic Celluvisc CLINICAL ADMINISTRATION Patient History Clinical Procedures Which May Be Influenced by Medications The ERx Option Ophthalmic Drug Complications Giving people medications may seem routine, but there are possible negative consequences. Not all people are tolerant of all medications. If given a drug they can’t tolerate, a patient may have an allergic or toxic reaction. As an eye technician administering drugs to people on a daily basis, it’s important you understand and recognize what is occurring if a patient does have a reaction. You also need to understand how drugs affect the body’s autonomic nervous system (ANS), to include the sympathetic and parasympathetic divisions. THERAPEUTIC AGENTS TPAs treat disease, known problem Antibiotics Anti-virals Drugs that lower IOP Anti-inflammatory agents Non-Steroidal Combinations GLAUCOMA MANAGEMENT Pilocarpine Beta-Blockers Carbonic Anhydrase Inhibitors Adrenergic Agonists OCULAR INFLAMMATION Corticosteroids Steroid-Antibiotic Combinations Non-Steroidal Anti-inflammatory Drugs (NSAIDS) Oral Analgesics OCULAR INFECTIONS Topical Antibiotics Oral Antibiotics Anti-Viral Analgesics Antibiotic Biotic means relating to, produced by, or caused by living organisms The prefix anti "against" the referent of the stem to which the prefix is affixed OCULAR SURFACE Artificial Tears Lubricating Ointments Punctal Occlusion OCULAR ALLERGIES Artificial Tears Antihistamine-Decongestants Corticosteroids Cap Color Code Tan- antibiotics Pink- anti-inflammatory/steroids Red- mydriatics/cycloplegics Grey- NSAIDS Green- miotics Yellow or Blue- beta-blockers Purple- adrenic agonists Orange- carbonic anhydrase inhibitors Turquoise- Prostaglandin analogues IN-OFFICE PROCEDURES Patient Instruction- Solutions and Suspensions Wash hands thoroughly before administration Tilt head backward or lie down and gaze upward Gently grasp lower eyelid below eyelashes and pull the eyelid away from the eye to form a pouch Place dropper directly over the eye. Avoid contact of the dropper with the eye, finger or any other surface Release the lid slowly and close the eye Occlude punta for 2-3 minutes Wait 5 minutes before administering a second medication or drop Patient Instruction- Ointment Wash hands thoroughly Tilt head backward or lie down and gaze upward Gently pull down the lower lid to form a pouch Place .25 to .50 inch of ointment with a sweeping motion Close the eye for 1-2 minutes Temporary blurring of vision may occur. Remove excess ointment with a tissue Wait 10 minutes before applying the second ointment Continuous release delivery A medication device placed in the eye and lasting for a week is quite a benefit to patients who have trouble keeping up with their drops. The most common of these devices is the Pilocarpine Ocusert®, which permits continuous delivery of medication 24 hours a day for seven days. Retro-Bulbar Injection Subconjunctival injections Injections may be administered under the conjunctiva to deliver medications in large doses and longer durations (fig. 4–4). The subconjunctival medication gains access to the eye by absorption into the bloodstream through the episcleral and conjunctival vessels. Subconjunctival injections are used primarily in the treatment of intraocular infection or acute uveitis cases. ABBREVIATIONS Examples ad lib- freely as needed ac – before meals bid- twice a day gtt- Drops hs- at bedtime pc -after meals po- by mouth prn- as needed Examples- con’t oint- ointment q- every qh- every hour q4h- every four hours qid- 4 times a day sig- instructions sol- solution susp- suspension Examples- con’t tab- tablet tid- three times a day top- topically ung- ointment ut dict- as directed Abbreviation Meaning Abbreviatio n Meaning Prescription abbreviations (ante cibum) before meals ac q (quaque) every (ad libitum) as much as wanted qd (quaque die) every day aq Water qh (quaque hora) every hour bid (bis in die) twice a day qid (quater in die) 4 times a day (gutta; guttae) drop; drops ql ad lib gt; gtt (quaque quarta hora) every four hours h hora) hour hs (hora somni) at bedtime qs quantity sufficient mg Milligram Rx (recipe) prescription (non repetatur) do not repeat Sol solution pc (post cibum) after meals Tid (ter in die) three times a day po (per os) by mouth, orally ung (unguentum) ointment prn (pro re nata) as needed non rep qqh or q4h (quantum libet) as much as desired Mydriatic Mydriasis is the dilation of the pupils, so, logically, a mydriatic drug causes dilation. The main reason the eyes is dilated is to allow the doctor to perform a thorough exam of the posterior portion of a patient’s eyes. A big pupil allows a wider field of view and gives the examiner a chance to see the vast majority of the retina, rather than the very small amount seen in an undilated eye. Mydriasis is also useful in allowing you to take fundus photographs of the macula, optic nerve, and any retinal anomalies present. Cycloplegics These drugs cause mydriasis like mydriatics, but they also cause cycloplegia, which is paralysis of the ciliary muscle. Remember, the ciliary muscle controls focusing of the light rays entering the eye by changing the shape of the crystalline lens. Cycloplegics are used in dilating the pupils to facilitate examination of the fundus, prevent ciliary spasm and pain in iritis patients, and prevent a patient (usually a suspected hyperope) from constantly accommodating while the doctor is trying to refract the patient and figure out the prescription. Cycloplegics are also used to perform entrance eye exams on flyers to find what their true refractive error is. Again, this is accomplished by paralyzing the focusing mechanism of the eyes (temporarily) while the doctor refracts the patient. Cycloplegics almost always come in bottles with red caps. Tropicamide (Mydriacyl®; Opticyl®) The information you need to know about tropicamide is: • Preparation: Solution, 0.5 – 2 percent (most common usage is 1 percent). • Dosage: Instill one drop in each eye. Repeat if the doctor requests it. • Action and uses: Produces mydriasis and cycloplegia. Onset of action is rapid (20 – 30 minutes) and duration varies from one-half to four hours. Used primarily in conjunction with phenylephrine when dilating patients for routine fundus exams. May be used for unofficial Beta-Blockers Beta-blockers are the current drugs of choice in lowering IOP. Timoptic®, Betoptic®, and Betagan® are some of the most popular drugs being used to lower IOP today. Introduced in the late 1970s, they quickly became the initial drug of choice for lowering IOP. One reason beta-blockers are so popular is, on average, they reduce IOP by 25 percent. Another reason is they can be used once or twice daily, unlike most previous medications that were used up to four times a day. Finally, most of the previous drugs used to lower IOP caused miosis (pupillary constriction), dim vision (due to constricted pupil size), eyebrow ache, and stimulation of accommodation (which can blur vision). Fortunately, beta-blockers work without these side effects. However, this does not mean they are perfect, as they also have some side effects. Beta-Blocker Complications Beta-blockers block the beta–1 and beta–2 receptors from doing their jobs in the body. This is good because one of the jobs of the receptors involves maintaining normal production of aqueous humor. By slowing down aqueous production, the IOP can be lowered. The downside is some of the other jobs beta–1 and beta–2 receptors include proper heart rate and breathing. Basically, if a patient systemically absorbs a beta-blocking medication, it slows the heart rate and makes breathing difficult. Not a great thing to have happening when you consider the age and general health of a lot of your glaucoma patients. Risk of Complications Thus, patients with certain systemic diseases warrant special consideration by a doctor trying to decide whether the person should use beta-blockers or not. The following is a very general list of systemic conditions contraindicating beta-blocking medication usage. • Asthma. • Heart or circulatory problems. • Chronic obstructive pulmonary disease (COPD). In addition, patients already on systemic beta-blockers (e.g., Inderal® for high blood pressure) should be considered high-risk candidates for use of any of the beta-blocker medications. Patients may be better off using one of the cholinergic medications, carbonic anhydrase inhibitors, or prostaglandin inhibitors instead. Some of the common side effects of beta-blockers (especially the more medication the patient systemically absorbs) are: • Bradycardia—the slowing down of the heart rhythm (leading to low blood pressure and dizziness). • Induced asthma. • Mood changes. Cholinergic agents (direct-acting miotics) These drugs are the traditional medications used to lower IOP. They have fallen out of the widespread usage once enjoyed before the beta-blockers and prostaglandins came along. However, they still play a role in the management of IOP as there are times betablockers alone do not lower IOP enough or patients require specific treatment working on the outflow of aqueous humor rather than just slowing its production. These cholinergic drugs lower IOP by causing the longitudinal muscle of the ciliary body to pull on the sclera near the base of the iris and the trabecular meshwork. Pulling in the ciliary body causes an opening or rearranging of the trabecular meshwork, allowing the aqueous to drain from the eye faster. Since these drugs work directly to cause contraction of the ciliary muscle, they are considered to be direct-acting miotics and are primarily used in the treatment of angle-closure glaucoma. While the primary action desired from these miotic medications is to increase aqueous humor Topical Steroids Durezol Pred Forte Prednisone Omnipred Econopred Avoid using steroids on viral infections Contraindications for Steroids Cataracts. Increased IOP. Fungal overgrowth. Delayed wound healing. Decreased wound healing. Decreased resistance to infection. Proliferation of herpes simplex virus NOTE: Virtually all of these side effects are quite rare when the proper dosage of topical steroid is used in a short-term manner as prescribed by the doctor. Topical NSAIDS Bromday – Prolenza Nevanec Used often for pre/post cataract surgery Cap Color Drug Class Antibiotics, Antivirals, Antifungals CAP Colors Pink Anti-inflammatory/Steroids treats allergic reactions, swelling, Tan redness (slows healing can cause cataracts and glaucoma). Do not use on fungal infections Red Mydriatics/Cycloplegics (dilate pupil) Grey Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) control inflammation caused by ocular allergies without steroidal sideeffects Green Miotics (stimulates sphincter and causes pupil constriction) Yellow or Blue Beta-Blockers traditionally used to treat glaucoma, reduce IOP by decreasing aqueous humor Purple Adrenic Agonists (reduce IOP) Orange Carbonic Anhydrase Inhibitors (reduce IOP) Turquoise Prostaglandin Analogues (reduce IOP by increasing aqueous outflow) HOW TO WRITE AN Rx Medication Administration Read the doctors orders Check the medication twice Name Dosage Amount Expiration date Wait 5 min between gtts Punctal Occlusion Put ung in last Preparation 1. Wash your hands. 2. Triple check the medication you are going to instill to ensure it is what the doctor ordered. 3. Advise the patient of what you are going to do. 4. Recline the patient or gently tilt the patient’s head back. Always ask the patient about neck or back problems before tilting his or her head. Do not tilt a Down’s syndrome patient’s neck due to the high risk of cervical fracture. 5. With one hand, hold the upper lid and, with a finger of the other hand (the one holding the little bottle of medication), pull down gently on the lower lid (fig. 4–1). 6. Have the patient look down. 7. Keep the bottle about ½″ above the eye. This should be high enough to avoid contamination by the patient’s eyelashes in the event the patient inadvertently blinks, while still allowing good control of where the drop goes. Now, squeeze the bottle to dispense a drop in the eye. Ideally, the drop hits just above the upper limbus, causing minimal reaction by the patient (since the very sensitive cornea isn’t hit directly), but allowing a good percentage of medication to flow across the cornea before it gets diluted by tears. CAUTION: Keep the eye dropper tip well away from the eye so, even if the patient blinks, the lashes do not touch it. If the dropper tip comes into contact with the patient’s eyes, lids, or lashes, the bottle is considered contaminated and must be thrown away after you finish with the patient. Do not attempt to use it on another patient. Make sure that you include: Full name of patient Address can be optional Date of Rx Inscription: name of drug; concentration Subscription: amount to be dispensed Instructions: route of administration; number of drops or tablets; frequency of use; refill What else? Make sure that it is legible! Type in correctly Verify Questions What type of drug is used to lower IOP? A. Mydriactic B. Antibiotic C. Beta Blocker How often is the following medications taken? Maxitrol ophthalmic ung apply BID OU for 14 days: A. Once a day B. Twice a Day C. Three times a Day Questions What drug is used to stain the cornea? A. Mydriacyl B. Carbachol C. Flourescein How often is the following medications taken? Pred Forte ophthalmic 1gtt qid q 6h OD 7 days then 1gtt bid q 12h for 7 more : ****No help**** Questions What drug is used to destroy bacteria? A. Bromday B. Antibiotic C. Beta Blocker What drug is used increase aqueous outflow? A. Vigamox B. Pilocarpine C. Mydriacyl Questions What drug is used to dilate the pupil? A. Miotic B. Mydriacyl C. Beta Blocker What drug is used as an anti-inflammatory? A. Durezol B. Vigamox C. Besivance Examples ad lib- ________ ac – ________ bid- _________ gtt- _________ hs- _________ pc -__________ po- __________ prn- __________ Examples ad lib- freely as needed ac – before meals bid- twice a day gtt- drops hs- at bedtime pc -after meals po- by mouth prn- as needed References and resources Ophthalmic Drug Facts 2002 Ophthalmic Medications and Pharmacology Review of Optometry: 2002 Clinical Guide to Ophthalmic Drugs (Melton and Thomas) May issue THANK YOU!