Handout #1
advertisement

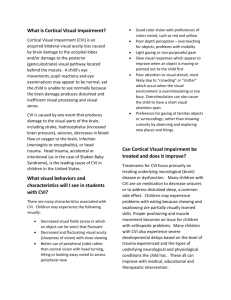
What are the characteristics of children with visual impairment in the era without Dr. James E. Jan? A review of the first 10 years since his retirement. Carey Matsuba, MD CM Visual Impairment Program BC Children’s Hospital Sunny Hill Health Centre Objectives • To review criteria for visual impairment • To discuss comment on the presentation of visual impairment in children • To review the common co-morbid conditions associated with visual impairment • To discuss challenges in diagnosis Background • The Visual Impairment Program is in its 5th decade of existence. • Initially founded by Dr. James E. Jan, the program offers consultative assessment services to assist children and adolescents with visual impairment throughout the British Columbia and the Yukon. James E. Jan • Recognized that different visual diagnoses were associated with unique characteristics. • The following represents the first 10 years of children who presented with visual impairment. Methods • In this period, 939 new patients were referred for assessment of which 691 patients met criteria for visual impairment. • The range of ages for the first assessment was from birth to 16 years of age. • Using this cohort, the distribution of visual impairment and co-morbid characteristics will be described. Criteria of Visual Impairment (Canada) • Visual Impairment is defined as a reduction in visual acuity or loss in visual field. • Most provinces use – 20/70 or worse for low vision – 20/200 or worse for blindness – Less than 10 degrees from central fixation Criteria for Visual Impairment (ICD-10) Category Worse than Equal to or better 0 Mild / No VI 6/18; 3/10; 20/70 1 Moderate 6/18; 3/10; 20/70 6/60; 1/10; 20/200 2 Severe 6/60; 1/10; 20/200 3/60; 1/20; 20/400 3 Blindness 3/60; 1/20; 20/400 1/60; 1/50; 20/1200 4 Blindness 1/60; 1/50; 20/1200 Light Perception 5 Blindness 9 No Light Perception Undetermined or Unspecified If the extent of the visual field loss is taken into account, patients with a field no greater than 10 degrees, but greater than 5 degrees around central fixation should be placed in category 3 and patients with a field no greater than 5 degrees around central fixation should be placed in category 4, even if the central acuity is not impaired Visual Impairment NLP Blind Visual Impairment Normal Vision Vision develops over time • It relies on – Opportunity – Practice – Experience – Interaction – Development Aetiology of Visual Impairment DVM CVI/CNS ONA ONH Retinal Structure Nystagmus Not VI Referrals Age at Presentation (n = 691) Age by Diagnosis Other Visual Diagnosis Nystagmus Structure Nystagmus Structure Retinal Retinal ONH ONH ONA ONA CVI CVI/CNS 0 10 20 30 40 50 60 70 Diagnosis vs Severity Low Vision 20/200 FC LP / B DVM 2 11 3 CVI/CNS 95 118 98 ONA 16 16 5 ONH 14 15 24 Retinal* 56 59 26 Structure 19 31 20 Nystagmus 38 24 0 *1 patient was not testable at assessment At last follow-up (n = 507) Not VI Low Vision 20/200 FC LP / B / (D) DVM 4 3 1 0 (1) CVI/CNS 30 76 76 40 (8) ONA 7 9 7 5 (1) ONH 8 9 15 8 (3) Retinal 15 39 32 15 (2) Structure 3 21 19 11 Nystagmus 10 21 7 0 (D) = died before follow-up assessment An additional 3 patients moved out of the area The acuity was not adjusted for age. (1) Hearing Nystagmus Structure Retinal ONH Confirmed Suspected ONA CVI/CNS DVM 0 5 10 15 20 Cognitive Nystagmus Structure Retinal ONH GDD / MR LD / ASD ONA CVI/CNS DVM 0 20 40 60 80 100 Motor Nystagmus Structure Retinal ONH CP Delayed ONA CVI/CNS DVM 0 20 40 60 80 Seizures Seizures Nystagmus Structure Retinal ONH Seizures ONA CVI/CNS DVM 0 20 40 60 80 Challenges • Cortical Visual Impairment • Retinal Abnormalities • Function Cortical Visual Impairment • Dr. Jan described patients with CVI – Reduction in visual acuity that could not be explained by anterior pathway disease – Physiological reason for an impairment – the aetiology for bilateral occipital pathology; identified by imaging and/or electrophysiological studies – Clinical characteristics – light gazing, colour preference, variability in visual attention Can you have CVI without clinical characteristics? Maybe… • A patient with isolated (focal) bilateral occipital damage (eg infarction) may present with a reduction in visual acuity without the clinical characteristics of CVI • These patients are more in keeping with “cortical blindness”. Retinal Dystrophies • There hundreds of different aetiologic conditions that can lead to retinal dystrophies. • The clinical presentation can be quite variable; as a result some will have a reduction in visual acuity in the first decade, while others may be clinical asymptomatic until well into adulthood. When should you be diagnosed with visual impairment in retinal dystrophy? Trends in Diagnosis • Over the past decade, our program has had a number of referrals as a result of abnormalities in the fundi exam and an abnormal ERG; but normal or near normal visual acuity • The patients in the past would not have presented until they were symptomatic. Challenges in the context of “normal” or “near normal acuity” • Inability to predict course of the condition, even if there is a family history • The importance of using vision to understand concepts vs the introduction of non-visual strategies Should we consider function in the diagnosis of visual impairment? Pros • Represents how a person uses their vision in the context of the individual’s skill within the environment Cons • Everyone can have functional difficulties • Function is highly dependent on ability, familiarity, perspective. • There is no clear measure to determine “functional visual difficulties”. For example, some would consider dyslexia as functional difficulty Conclusions • The epidemiological features of childhood visual impairment has remain similar over the past decade. • There has been some new challenges in the diagnosis of visual impairment that needs further discussion Questions Contact: cmatsuba@cw.bc.ca