Dizziness in the ED: Its Enough to Make Your Head Spin!
advertisement
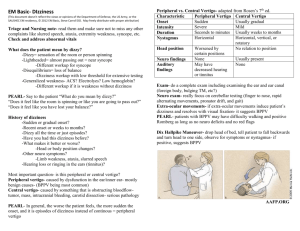
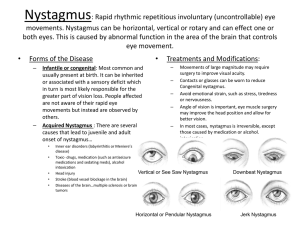
Dizziness in the ED: It’s Enough to Make Your Head Spin! Saurin Bhatt, MD/MBA Associate Staf f, Cleveland Clinic March 6, 201 2 Dizziness 2.3 - 2.6 million patients representing (about 1.5% of ED visits) over $1.6 billion in health care expenditures per year high incidence, cost, and potentially serious underlying causes of dizziness (TIA, stroke, arrhythmia) Proper Care of Your Dizzy Patient What does the patient mean? Vertigo, presyncope, syncope, weakness, anxiety, AMS Women and geriatric populations - atypical or under recognized symptoms of MI or stroke presenting as dizziness Elderly - several factors making them risky patients for cerebrovascular or cardiovascular disease Multiple causes of dizziness Who needs to get involved? Neurology/Neurosurgery, ENT, Cardiology, Toxicology, ICU, or Psychiatry Differentials of Dizziness Dizziness Subtype Type of Sensation Temporal Characteristics Selected Differentials Vertigo Spinning or Motion Sensation Episodic or Continuous BPPV Meniere’s Disease Labyrinthitis Vertebrobasilar Ischemia Cerebellar Infarction or Hemorrhage Presyncope Feeling Faint, or about to pass out Episodic, may last for seconds, may be alleviated by lying down Dehydration Anemia Cardiac Ischemia Arrhythmia Infection Hypo/Hyperglycemia Disequilibrium Unsteady feeling in Continuous, but may the lower extremities vary in intensity Multiple Sensory Deficits Peripheral Neuropathy Vision Loss Lightheadedness Vague complaints, nonspecific Medication Related Psychiatric Disorders including Anxiety, Depression, Panic Attacks Hyperventilation History is Key Obtaining a description of symptoms without using the word dizziness may be challenging at times Focus on: Timing Triggers Progression of the symptoms Associated symptoms PE Essentials Largely guided by history, but almost always entails a detailed neurologic examination. Full Neurologic examination Cranial Nerves, especially CN VII and VIII Gait, truncal ataxia, strength, sensation, DTR Pronator drift, FTN, Romberg tests Ear Examination Cardiovascular examination Carotid bruits, irregular rhythm. PE Essentials Eye examination Nystagmus Vestibular Ocular Reflex (Head Impulse Test) Skew Testing Conjugate gaze Nystagmus Evaluation Pattern Type Nystagmus Characteristic Cause Peripheral Upbeat Torsional Nystagmus with Dix Hallpike Maneuver Benign Paroxysmal Positional Vertigo Peripheral Unidirectional Spontaneous Nystagmus Vestibular Neuritis Central Vertical Nystagmus Strokes, Chiari Malformation, MS Central Direction Dependent Changes Medications (antiepileptic), Stroke, MS Central Downbeating with Dix Hallpike Chiari Malformation or cerebellar space occupying lesion Central Intranuclear Opthalmoplegia MS, Stroke Physiologic Unsustained Gaze Dependent Nystagmus Vestibular Ocular Reflex Head Thrust Maneuver Patient moves the head back and forth 20 degrees in each direction while gazing on a fixed object (your nose) Disruption during vertigo suggests peripheral cause Normal response in the setting of dizziness is suggestive of cerebellar stroke HEAD IMPULSE TESTING SKEW TESTING EXAMINATION IS BETTER THAN MRI! In an article published in Stroke September 2009, the HINTS examination (Head Impulse, Nystagmus testing, and Testing of Skew) was more sensitive than DWI MRI within the first 48 hours of symptoms. These three tests together take at most 2 minutes to perform and should be included in the examination of anyone complaining of persistent or constant dizziness. A Word about Imaging Sensitivity of CT for identifying any stroke in the acute setting in 2007 data is 26%. MRI is more sensitive (83%), but not many of emergency physicians have this access acutely Even then, sensitivity is lowest within 24 hours of onset and when the lesion is in the brainstem or cerebellum. Peripheral vs. Central Best way to rule out central disorder is to rule in a specific peripheral vestibular disorder Peripheral vs. Central Characteristics Characteristic Peripheral Central Onset Sudden Gradual Frequency Episodic, Recurrent Constant, Progressive Duration Seconds, Minutes Weeks, Months Nystagmus Horizontal Vertical Triggered by Movement? Yes Symptoms may worsen, but generally are not triggered with movement. Isolated Hearing Loss? Yes Other Neurologic findings are usually present. Fatigable Yes No Associated Symptoms Tinnitus, N/V Neurologic/Visual Symptoms Postural Instability No (may lean towards lesion) Yes Dix-Hallpike Maneuver Dix-Hallpike test for BPPV Person from sitting to supine position, head turned 45 o to one side and extended about 20 o backward Once supine, eyes typically observed for about 30 seconds. If no nystagmus ensues, the person is brought back to sitting. Delay about 30 seconds again, and then the other side is tested Positive Dix-Hallpike tests consists of a burst of nystagmus Epley Maneuver Have the patient sit upright Turn the patient’s head to the symptomatic side at 45 o angle, lie on the back Remain in this position until resolution of the nystagmus Turn the patient’s head 90 o to the other side Remain up to 1 minutes in this position Roll their body further in the same direction, so that the patient has their head facing nose down Remain up to 1 minute in this position. Go back to the sitting position and remain up to 30 seconds in this position. During every step of this procedure the patient may experience some dizziness Benefit of Residents… Decision Tree For Dizziness Use history and physical exam to determine category Are there any migraine symptoms? The ones to not send home… Diagnoses to not miss! Cerebellar stroke Vertebrobasilar stroke Space occupying Lesions NPH Hypoperfusion states MS (not emergent), but can be found on examination Cerebellar Stroke 20,000 of total strokes Often nonspecific findings (N,V, unsteady gait, or HA) and subtle neurologic findings (ataxia, dysarthria, and nystagmus) HINTS may be diagnostic Caution with negative neuroimaging; maintain a high index of suspicion. Vertebrobasilar Stroke more neurologic abnormalities than cerebellar strokes due to involvement of the posterior circulation HA, dizziness, vertigo, or confusion may be complaints PE findings include pupillary abnormalities, abnormal ocular movements, facial palsy, hemi/quadriplegia Space Occupying Lesion Cerebellopontine angle tumors - slow progress (weeks or months) Symptoms = vertigo, hearing loss, tinnitus, or facial weakness/ numbness (CN 7 and 8 involvement) Occipital HA can also be present With progression, look for signs of increased ICP: papilledema or mental status changes NPH Usually in 60’s or 70’s - classic triad of unsteady gait, dementia, urinary incontinence Gait is wide based, reduced step height and length, and decreased speed Urinary frequency and urgency are earliest manifestations Dementia - memory impairment with decreased attention, alertness, or speed of mental processing Ventriculomegaly can be discovered on CT or MRI Hypoperfusion States Decreased cerebral perfusion can lead to AMS or sensation of dizziness Shock may be apparent with vital signs changes, normally hypertensive patients with normal blood pressure or having certain beta blocker/calcium channel blockers may not have the traditional changes in vital signs Decreased cardiac output from ACS may present as hypotension, cooler skin, dyspnea, rales, confusion, AMS, or dizziness Multiple Sclerosis Typically young adults (25-45). Vertigo is the presenting symptom for 5% of patients 50% of MS patients have vertigo INO found during nystagmus testing indicates MLF involvement and due to heavy myelination of the MLF places MS high on the differential Prominent symptoms may include numbness or paresthesias As Emergency physicians we should evaluate for other disease processes and refer to neurology for workup Medical Treatment Options Goal - stabilize symptoms and identify treatable disorders BPPV can be treated with head repositioning maneuvers Symptomatic Medication options Dimenhydrinate IV (Dramamine) Meclizine PO (Antivert) Scopolamine transdermal patch Benzodiazepines Antinausea medication if prominent feature Corticosteriods and valacyclovir have been used for vestibular neuritis, but viral eitiology is rarely identified. KEY LECTURE POINTS HINTS examination has a great sensitivity for finding central lesions. The Dix-Hallpike Maneuver and Epley Maneuver not only diagnose BPPV, but also treat BPPV. Rule out a central lesion by ruling in a peripheral lesion. Always maintain a high degree of suspicion. A negative CT or MRI especially in the acute setting does not mean that there is no stroke! References Seminars in neurology: Vertigo presentations in the emergency department Academic emergency medicine : official journal of the Society for Academic Emergency Medicine: Nystagmus assessments documented by emergency physicians in acute dizziness presentations: a target for decision support? Annals of Emergency Medicine : Risk of vascular events in emergency department patients discharged home with diagnosis of dizziness or vertigo. Emergency Medicine Clinics of North America : Dizzy and confused: a step-by -step evaluation of the clinician's favorite chief complaint American family physician : Dizziness: a diagnostic approach Neurology: Approach to the Dizzy patient in Practical Neurology