Treatment for Insomnia
advertisement

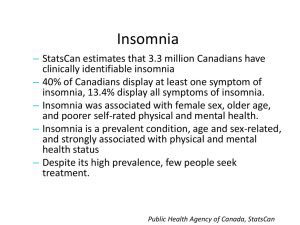
Treatment for Insomnia Presentation By: JJ Wojcik Presentation Outline What is Insomnia? Treatment of Insomnia Non-Pharmacological Pharmacological Benzodiazepines Benzodiazepine Receptor Agonists Melatonin-Receptor Agonists Anti-Depressants Future Treatments What is Insomnia? Classified as the inability to get enough sleep despite adequate time. Symptoms Include: Delayed Sleep Onset Early Morning Wake-Ups Unrefreshing Sleep Trouble Maintaining Sleep Causes many problems in daytime functioning Classifications of Insomnia Primary vs. Secondary This is based on what is causing a patient to suffer from lack of sleep Chronic vs. Acute This is based on how long the patient suffers from symptoms of insomnia Primary Insomnia Also referred to as Idiopathic This is diagnosed when a patient has no other cause of insomnia other than the fact they cannot sleep Also been known to be patient confusion and misconception around what is meant and understood to be sleep Secondary Insomnia This is also more commonly referred to as Comorbid Insomnia When insomnia is being caused by some other outside factor, illness, or disorder including: Drug Abuse Psychiatric Disorders Medical Problems Other Sleep Disorders disruptive to sleep Acute Insomnia This is when a patient suffers from insomnia fewer than 3 times a week for less than a month Typically stems from changes in the environment and a short illness the patient might have had Chronic Insomnia This will be diagnosed when a patient suffers from symptoms more than 3 times a week for a period longer than a month When insomnia becomes a chronic problem, it is typically said to be comorbid insomnia Causes of Insomnia Often caused by depression or other psychiatric problems Also caused by excess, lasting stress or racing thoughts at bedtime Symptoms of insomnia also could be cause by other sleeping disorders such as: Restless Leg Syndrome Sleep Apnea Somnolence Diagnosing Insomnia The diagnosis of insomnia can often be difficult and is a prolonged process Sleep logs Watching symptoms for weeks at a time It is often very underdiagnosed due to both patient and physician misunderstandings Doctors don’t routinely ask about it Patients don’t think it’s important enough to bring up in a normal check up Goes overlooked Treatment of Insomnia Insomnia is not a disorder that can necessarily be “cured” Symptoms treated in order to relieve patient of distress Treated by two different methods Non-Pharmacological Treatment Pharmacological Treatment Non-Pharmacological Treatment This is attempted before the use of pharmacological treatment, typically for at least 2-3 weeks This mainly has to do with attempting to improve sleep habits The different methods used are: Improving Sleep Hygiene Stimulus Control Therapy Restrictive Sleep Therapy Improving Sleep Hygiene Basically improving comfort when sleeping Decrease Ambient Noise Go to bed/wake up at a constant time Reduce Lighting Think Positively Not shown to be particularly effective on its own, though has been seen to be very critical to improving the efficacy of other non-pharmacological treatments Stimulus Control Therapy Learn to associate the bedroom with sleep alone Don’t go in the bedroom unless going to sleep Do not go to bed unless tired Leave the bedroom if haven’t fallen asleep in 15 minutes Be completely relaxed when in bed This method has been seen to be very effective if used for over a prolonged period of time Improved efficacy if sleep hygiene is also managed Sleep Restriction Therapy Restricting sleep during the day Cutting sleep short during certain nights Goal is to be excessively tired when time to sleep at night Shown the most promising results of all the nonpharmacological therapies and even more effective when sleep hygiene is improved Pharmacological Treatment This is the treatment of insomnia with the use of pharmacological agents Most often prescription agents Some supplements used 4 Classes of Prescription Agents Benzodiazepines Benzodiazepine Receptor Agonists Melatonin Receptor Agonists Antidepressants/Antipsychotics Some supplements are thought to help as well Benzodiazepines More than 45 years old and are potent hypnotics and anxolytics Improve sleep time, but not usually sleep latency (often one of the more desired effects) Disrupt normal sleep cycles Tend to cause bad “hangover” effects Very drowsy the following day Occasional impaired cognition Extremely high potential for abuse with prolonged use as well as tolerance Drugs in this class are Estazolam, Flurazepam, Quazepam, Temazepam, and Triazolam Triazolam Mechanism Interacts with the GABAA receptor to bind at the post synaptic membrane and induce chloride permeability to inhibit excitation By doing so, hypnotic effects are induced, and inducing sleep is therefore achieved Improves sleep onset, but not necessarily sleep maintenance Bad reported rebound insomnia with discontinued use Pharmacokinetics This has a very short half-life, as many of the other benzodiazepines, staying in the system about 2-5 hours The amount in the system (AUC) is proportional the dose Clearance and time for elimination are not dose dependent Other Benzodiazpeines Flurazepam Quazepam Temezepam Benzodiazepine Receptor Agonists Fewer hangover symptoms than benzodiazepines Claim amore restful night sleep Fewer problems with dependency, though still an issue Do not show deleterious effects to the sleep cycle Longer half-life than benzodiazepines so help with sleep maintenance Some drugs are dose dependent (Eszopiclone) Few are approved for long-term use: Eszopiclone Drugs in the class include: Zolpidem, Zaleplon, and Eszopiclone Eszopiclone (Lunesta) Mechanism Binds at the omega subunit of the GABAA receptor to increase chloride permeability and decrease excitation of the neuron This subunit is found more in the brain as opposed to the spine where the other class of the GABA receptors are found Thought to be safer than benzodiazepines, but still have serious potential for abuse, and reported rebound insomnia with discontinued use Effectiveness of the drug is dose dependent Pharmacokinetics This drug does have a relatively fast half-life and elimination time but can be delayed after a high fat meal Both the AUC and the Cmax were seen to be dose dependent in the patients examined CYP 3A4 and 2E1 were involved in the metabolism of the drug Mean elimination time was 5.8 hours Melatonin Receptor Agonists Newer class of drug Far less potential for abuse and dependency and is the only hypnotic that is not classified as a controlled substance Approved for long-term use more readily than other medications There have been complains of drowsiness, dizziness, and fatigue in the following days after use Only drug in this class thus far is Ramelteon Ramelteon Mechanism This works by selectively binds the Melatonin Receptors (MT)1 and MT2, that are thought to regulate the sleepiness and readjustment of the circadian rhythms, respectively Does not show any addictive or dependency in patients because it does not, nor do any of its metabolites, bind to any large ligand group receptors Pharmacokinetics Undergoes extensive first pass metabolism Half-life ranged from 1-3 hours All pharmacokinetic properties have been seen to be dose proportional Antidepressants/Antipsychotics Some physicians prefer this mode of treatment over benzodiazepines because of the far less potential for dependency Can produce anticholinergic effects if used too long: Constipation Weight Gain This is mostly used in patients who suffer from comorbid insomnia as a result from depression Non-Prescription Supplements There are certain different non-prescription supplements that are also used an thought to be effective These include: Antihistamines Melatonin Valerian Antihistamines Used because many people will experience sleep inducing side effects from this kind of medicine Typically in patients with acute insomnia who need a “quick fix” for a restless night here and there Tolerance can and most often will be gained if used too much Melatonin Naturally produced hormone in the pineal gland This hormone keeps the circadian rhythm There has not been a minimum dose established Not shown to be necessarily effective Valerian This is an herb that is thought to interact at the GABAA receptor because of it’s sedative properties similar to other drugs that act at that receptor Can cause some nausea, upset stomach, dizziness, and long-lasting fatigue Is included on the FDA’s Generally Recognized as Safe List Future Treatments Most future treatments have to do with other stimulations of the GABA receptor Some facing problems for their problems in pregnant women and their abuse/dependency issues There are also trials being done to assess the efficacy of the 5-HT receptor in treating insomnia Different agonists have shown to improve sleep onset and sleep maintenance Many other Melatonin Receptor Agonists are also being researched to go alongside Ramelteon in this class of drug Assigned Reading Monti, Jaime M. Primary and secondary insomnia: Prevalence, causes and current therapeutics. Current Medicinal Chemistry: Central Nervous System Agents (2004), 4(2), 127-134. Homework Question Explain the mechanismm of action of the benzodiazepam class of hypnotic agent. References Sullivan, Shannon S.; Guilleminault, Christian. Emerging drugs for insomnia : new frontiers for old and novel targets. Expert Opinion on Emerging Drugs (2009), 14(3), 411-422 Passarella, Stacy; Duong, Minh-Tri. Diagnosis and treatment of insomnia. American Journal of Health-System Pharmacy (2008), 65(10), 927-934 Hair, Philip I.; McCormack, Paul L.; Curran, Monique P. Eszopiclone : a review of its use in the treatment of insomnia. Drugs (2008), 68(10), 1415-1434 Silvestri, R.; Ferrillo, F.; Murri, L.; Massetani, R.; Perri, R. Di; Rosadini, G.; Montesano, A.; Borghi, C.; Giclais, B. De La. Rebound insomnia after abrupt discontinuation of hypnotic treatment: Double-blind randomized comparison of zolpidem versus triazolam. Human Psychopharmacology (1996), 11(3), 225-233 Nguyen, Nancy N.; Yu, Susan S.; Song, Jessica C. Ramelteon : a novel melatonin receptor agonist for the treatment of insomnia. Formulary (2005), 40(5), 146-150, 152-155