Study to Assess Longer-term Opioid Medication Effectiveness
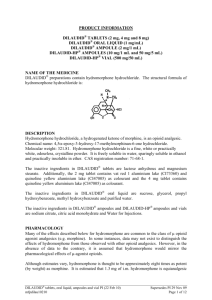
advertisement
SALOMÉ Study to Assess Longer-term Opioid Medication Effectiveness Rationale NAOMI: blinding was not broken among those receiving hydromorphone; almost identical treatment effect compared to diacetylmorphine (not powered). Hydromorphone: licensed drug in North America; similar pharmacodynamic profile of that of morphine, similar pharmacology of that of diacetylmorphine; commonly used as the ‘challenge’ drug in behavioral experiments studying heroin dependence; less stigma attached Rationale Health Canada denied compassionate access for diacetylmorphine in May 2008: In the course of reviewing your request, we determined that there are other options (i.e., marketed drugs) that we would consider alternative to diamorphine at this time. While studies have shown that diacetylmorphine and hydromorphone produce similar effects, hydromorphone has never been evaluated as a substitution treatment option for opioid dependency. Investigators Aslam Anis (Health Economics) Suzanne Brissette Julie Bruneau Amin Janmohamed (Study Pharmacist) Michael Krausz (Principal Investigator) Bohdan Noysk (Health Economics) Eugenia Oviedo-Joekes (Principal Investigator) Martin Schechter Christian Schultz General objectives 1) to evaluate if the closely supervised provision of injectable, hydromorphone is as effective as injectable diacetylmorphine in recruiting, retaining, and benefiting long-term opioid-dependent individuals who are not benefiting sufficiently from available treatments, and 2) to evaluate if a switch to the oral equivalent of hydromorphone and diacetylmorphine after six-months is as effective as remaining on the injectable medication. Planned sample n=322 Randomization Injectable DAM Injectable HDM Phase I Double blind Non-Inferiority of HDM to DAM 6 months evaluation Treatment effectiveness Randomization Double blind 12 months evaluation Treatment effectiveness 18 months evaluation Follow-up + Oral HDM Injectable DAM + Injectable HDM Non-Inferiority of Oral vs. Injecting Phase II Oral DAM Double blind Primary Hypotheses: Is injectable hydromorphone not inferior to injectable diacetylmorphine in reducing illicit heroin use in chronic intravenous opioid users after six months of treatment? (Stage I) Following at least six-months of treatment with injection opioids, is a switch to the oral form of the medication not inferior to continued injection treatment over the following six-months? (Stage II). non-inferiority trial Participants: inclusion criteria “chronic injection opioid users who did not benefit previously from the available therapies” Opioid Dependence as confirmed by DSM IV diagnostic criteria; 19 years of age or older; At least 5 years of opioid use; Injecting opioids regularly in the past year; At least two episodes of opioid addiction treatment (methadone maintenance, detoxification, residential care, etc), including one or more episodes of substitution treatment; Poor physical, psychological, mental or psychosocial functioning; PRIMARY OUTCOME MEASURE For both Stages I and II will be change in illicit heroin use from baseline: Use of illicit heroin at a time point is defined as the number of days of illicit (“street”) heroin use in the prior 30 days by means of self report (EuropASI). SECONDARY OUTCOME MEASURES Health Status including HIV risk behaviours Treatment retention Methadone use Treatment satisfaction Alcohol, tobacco and illicit drugs use Urinalysis for markers of street heroin use Criminal involvement OTHER EVALUATIONS Safety (Adverse events) Success of the blinding (potential use of hydromorphone open-label) Treatment effectiveness among women Treatment effectiveness among Aboriginal people. Histories of victimization Health economics (cost-effectiveness) Sample size Calculated based on illicit heroin use as the primary outcome, for a non-inferiority trial: For stage II, with an expected decline of 20 days from baseline, a margin of 4 days, a power of 0.955, an expected loss-to-follow-up rate of 0.05 and a one-sided alpha level of 0.05, requires 274 participants (137 per group). Thus, in order for 274 participants to enter into stage II, we will need to randomize 322 volunteers into stage I. The latter will yield a Stage I non-inferiority trial with a margin of 4 days, a one-tailed alpha level of 0.05, and a power of approximately 0.965. TREATMENT: DOUBLE-BLIND HYDROMORPHONE AND DIACETYLMORPHINE, INJECTABLE AND ORAL prescribed and self-administered in the study clinic under supervision. self-administered by injection or orally up to three times daily medication dosage will be prescribed in DAM-equivalent mg patients can at any time switch partially or totally to oral methadone study treatments will be provided for 12 months followed by a 1month transition period primary outcome measures will be assessed before any tapering or transition began. each client will be assigned a psychosocial support worker and will have access to a defined range of primary care services matched to the prevalent conditions seen in injection drug users. in keeping with the Health Canada Best Practices documents for methadone maintenance, all services will be delivered in a patient-centred fashion. IF HYDROMORPHONE IS DEMONSTRATED TO BE NON-INFERIOR TO DIACETYLMORPHINE … We will have established that this more widely acceptable drug can be used to stabilize the most adversely affected cases of opioid dependency in a medically prescribed injection program. Further study will also be required to show that open-label hydromorphone can also successfully attract patients into care and retain them. Current status Funding: CIHR grant: approved on March 31, 2009. Providence Health Care: 4 years funding for the clinical portion of the study (Crosstown Clinic). Fundraising: Innerchange Foundation to match CIHR’s funding, St. Paul’s Hospital Foundation. Health Canada: Therapeutic Products Directorate: No objection to our CTA. Dispensing of the medications upon stability and sterility testing results. Office of Controlled Substances: Section 56 Exemption obtained on June 2011.