Information Challenges
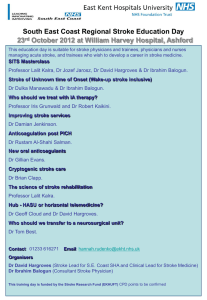
advertisement

Quality Standards: Information challenges in clinical practice (Stroke) Tony Rudd What are the problems that need solving? Unacceptable variation in the quality of care between hospitals Variable quality of clinical and managerial leadership Variable resources provided for stroke care UK slow to adopt new technologies e.g. Thrombolysis Still a belief amongst many people (professionals and public) that stroke untreatable disease of old people National Initiatives for Change NAO 2005 National Stroke Strategy 2007 National Sentinel Stroke Clinical Audit 2010 Round 7 Stroke Improvement Programme NICE Acute Stroke and TIA Guidelines No shortage of policy documents! ICSWP Stroke Guidelines 2008 Data requirements for Stroke Accelerated metrics NICE Quality Standards Integrated Performance Measures Reporting (Vital signs) Local stroke and cardiac network requirements Commissioning Outcomes Framework Quality Outcomes Framework National audits SINAP Sentinel carotid HES Data Patient satisfaction CQC Stroke Quality Standards: criteria for inclusion Standards covering whole pathway (therefore not just those in NICE Acute stroke and TIA guidelines). Used RCP National Clinical Guidelines Important clinically and some areas resistant to change Measurable, achievable and comparable between units Evidence based or very strong clinical consensus Excluded secondary prevention because already well covered by QOF Largely process measures where the process is known to affect outcome Using Quality Standards Setting the national agenda for Quality improvement Informing providers Including the QS in quality accounts Comparing performance between provider units Informing the users Public release of data on performance Using Quality Standards Informing commissioners Providing framework for commissioning of services But cannot be used as the exclusive document for defining components that are needed for a service. Indicative of the type of care needed Challenging the conventional models of care Use for CQUINS (Commissioning for Quality Improvements) and for World Class Commissioning Informing the regulators Informing the politicians No. NICE Quality Standards for Stroke 1 Patients with stroke are assessed and managed by stroke nursing staff and at least one member of the specialist rehabilitation team within 24 hours of admission to hospital, and by all relevant members of the specialist rehabilitation team within 72 hours, with documented multidisciplinary goals agreed within 5 days. 2 Patients with suspected stroke are admitted directly to a specialist acute stroke unit and assessed for thrombolysis, receiving it if clinically indicated. Patients who need ongoing inpatient rehabilitation after completion of their acute diagnosis and treatment are treated in a specialist stroke rehabilitation unit. All patients discharged from hospital who have residual stroke-related problems are followed up within 72 hours by specialist stroke rehabilitation services for assessment and ongoing management. 3 4 5 Patients with stroke are offered a minimum of 45 minutes of each active therapy that is required, for a minimum of 5 days a week, at a level that enables the patient to meet their rehabilitation goals for as long as they are continuing to benefit from the therapy and are able to tolerate it. 6 (a) People seen by ambulance staff outside hospital, who have sudden onset of neurological symptoms, are screened using a validated tool to diagnose stroke or transient ischaemic attack (TIA). (b) People with persisting neurological symptoms who screen positive using a validated tool, in whom hypoglycaemia has been excluded, who have a possible diagnosis of stroke, are transferred to a specialist acute stroke unit within 1 hour. Patients with acute stroke receive brain imaging within 1 hour of arrival at the hospital if they meet any of the indications for immediate imaging. Patients with acute stroke have their swallowing screened by a specially trained healthcare professional within 4 hours of admission to hospital, before being given any oral food, fluid or medication, and they have an ongoing management plan for the provision of adequate nutrition. 7 8 9 10 11 All patients after stroke are screened within 6 weeks of diagnosis, using a validated tool, to identify mood disturbance and cognitive impairment. Patients with stroke who have continued loss of bladder control 2 weeks from diagnosis are reassessed for the cause of incontinence, and have an ongoing treatment plan involving both patient and carer/s. Carers of patients with stroke are provided with a named point of contact for stroke information, written information about the patient’s diagnosis and management plan, and sufficient practical training to enable them to provide care. National Sentinel Audit Data 2004-2010 SINAP Audit 2011 Thrombolysis 5% of patients received altepase in 2010 Sentinel Audit (increased from 1.8% in 2008) 14% of patients should be receiving it (presented within 3 hours, 80 yrs or under, infarction) Still many areas of the country where hyperacute stroke care not adequately provided SINAP Audit 2011 Thrombolysis rates in London after introduction of London Stroke Strategy 16% Thrombolysis rates have increased since implementation began to a rate higher than that reported for any large city elsewhere in the world Feb – Jul 2009 AIM Feb – Jul 2010 14% 12% 12% 10% 10% 8% 6% 4% 2% 0% 3.5% No. NICE Quality Standards for Stroke 1 Patients with stroke are assessed and managed by stroke nursing staff and at least one member of the specialist rehabilitation team within 24 hours of admission to hospital, and by all relevant members of the specialist rehabilitation team within 72 hours, with documented multidisciplinary goals agreed within 5 days. 2 Patients with suspected stroke are admitted directly to a specialist acute stroke unit and assessed for thrombolysis, receiving it if clinically indicated. Patients who need ongoing inpatient rehabilitation after completion of their acute diagnosis and treatment are treated in a specialist stroke rehabilitation unit. All patients discharged from hospital who have residual stroke-related problems are followed up within 72 hours by specialist stroke rehabilitation services for assessment and ongoing management. 3 4 5 Patients with stroke are offered a minimum of 45 minutes of each active therapy that is required, for a minimum of 5 days a week, at a level that enables the patient to meet their rehabilitation goals for as long as they are continuing to benefit from the therapy and are able to tolerate it. 6 (a) People seen by ambulance staff outside hospital, who have sudden onset of neurological symptoms, are screened using a validated tool to diagnose stroke or transient ischaemic attack (TIA). (b) People with persisting neurological symptoms who screen positive using a validated tool, in whom hypoglycaemia has been excluded, who have a possible diagnosis of stroke, are transferred to a specialist acute stroke unit within 1 hour. Patients with acute stroke receive brain imaging within 1 hour of arrival at the hospital if they meet any of the indications for immediate imaging. Patients with acute stroke have their swallowing screened by a specially trained healthcare professional within 4 hours of admission to hospital, before being given any oral food, fluid or medication, and they have an ongoing management plan for the provision of adequate nutrition. 7 8 9 10 11 All patients after stroke are screened within 6 weeks of diagnosis, using a validated tool, to identify mood disturbance and cognitive impairment. Patients with stroke who have continued loss of bladder control 2 weeks from diagnosis are reassessed for the cause of incontinence, and have an ongoing treatment plan involving both patient and carer/s. Carers of patients with stroke are provided with a named point of contact for stroke information, written information about the patient’s diagnosis and management plan, and sufficient practical training to enable them to provide care. SINAP Audit 2011 No. NICE Quality Standards for Stroke 1 Patients with stroke are assessed and managed by stroke nursing staff and at least one member of the specialist rehabilitation team within 24 hours of admission to hospital, and by all relevant members of the specialist rehabilitation team within 72 hours, with documented multidisciplinary goals agreed within 5 days. 2 Patients with suspected stroke are admitted directly to a specialist acute stroke unit and assessed for thrombolysis, receiving it if clinically indicated. Patients who need ongoing inpatient rehabilitation after completion of their acute diagnosis and treatment are treated in a specialist stroke rehabilitation unit. All patients discharged from hospital who have residual stroke-related problems are followed up within 72 hours by specialist stroke rehabilitation services for assessment and ongoing management. 3 4 5 Patients with stroke are offered a minimum of 45 minutes of each active therapy that is required, for a minimum of 5 days a week, at a level that enables the patient to meet their rehabilitation goals for as long as they are continuing to benefit from the therapy and are able to tolerate it. 6 (a) People seen by ambulance staff outside hospital, who have sudden onset of neurological symptoms, are screened using a validated tool to diagnose stroke or transient ischaemic attack (TIA). (b) People with persisting neurological symptoms who screen positive using a validated tool, in whom hypoglycaemia has been excluded, who have a possible diagnosis of stroke, are transferred to a specialist acute stroke unit within 1 hour. Patients with acute stroke receive brain imaging within 1 hour of arrival at the hospital if they meet any of the indications for immediate imaging. Patients with acute stroke have their swallowing screened by a specially trained healthcare professional within 4 hours of admission to hospital, before being given any oral food, fluid or medication, and they have an ongoing management plan for the provision of adequate nutrition. 7 8 9 10 11 All patients after stroke are screened within 6 weeks of diagnosis, using a validated tool, to identify mood disturbance and cognitive impairment. Patients with stroke who have continued loss of bladder control 2 weeks from diagnosis are reassessed for the cause of incontinence, and have an ongoing treatment plan involving both patient and carer/s. Carers of patients with stroke are provided with a named point of contact for stroke information, written information about the patient’s diagnosis and management plan, and sufficient practical training to enable them to provide care. Duration of Rehabilitation Research evidence to show a link between intensity of therapy after stroke and outcome In UK majority of rehabilitation resources concentrated in hospitals Length of hospital stay falling after stroke (reduced from mean of 35 days to 20 days over last 10 years) Patients frequently complain that they sit in hospital doing nothing for long periods of time time (min.) 160 140 Belgium 120 England 100 Switzerland 80 Germany 60 40 20 0 total therapy physio-therapy occupational therapy speech therapy other therapies Appropriateness for Therapy Intensity of Therapy Received How deliver increased intensity? Different patterns of working e.g. Cutting down on bureaucracy Less one to one therapy and more group treatment Using non specialist therapists to provide cover Focussing treatment just on patients likely to benefit e.g. Stopping treatment earlier More therapists Stroke Data Collection in the Future: Sentinel Stroke National Audit Programme (SSNAP) Replacing all other statutory data collection (except IPMR!). Includes data needed for: NICE QS NHS Outcomes Framework Accelerated metrics COF Funded by HQIP Information Challenges Need to link datasets to cover the stroke pathway: Ambulance trust data (often without an NHS number) Acute hospital and primary care data Social care data Patient reported data Data protection requirements and the Information Commissioner making life unbelievably complex to obtain section 251 approval Information Challenges Freedom of information act: We will be reluctant to collect any data that might be in any way experimental We will be reluctant to do analyses of data that are exploratory We will be reluctant to collect any data that might be misinterpreted or not be statistically robust because of sample size issues Information Challenges Intellectual property rights HQIP issues with IPR to the audits it funds including those of commercial web developers HQIP (presumably therefore DH) wanting control over data analysis and publishing. Therefore at risk of losing clinical independence over national audit data Information Challenges Failure to make data collection in healthcare mandatory Proliferation of private companies offering third rate data collection tools at great expense resulting in failure to adequately collect data in a format that can be used for national data reporting Organisations that publish without any regard to accuracy or data quality Information Challenges Demands for reporting outcome data at a level that is clinically meaningless and misleading e.g. Individual stroke physician/hospital Numbers too small Difficulty adjusting for case mix Outcomes dependent upon large teams working in collaboration Conclusions NICE Quality Standards alongside other quality initiatives have undoubtedly resulted in improvements in clinical practice We need to simplify data collection; currently too great a burden for clinicians Major threats to our ability to conduct national audit