Medicine Powerpoint
advertisement

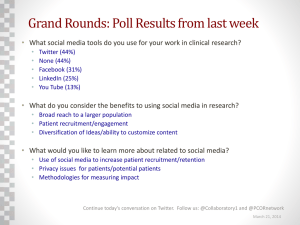
“Quality and Patient Safety 2008-09” A UF COM Educational Initiative Curriculum Committee June 10, 2008 UF COM Patient Safety Task Force Lou Ann Cooper Rick Davidson Marvin Dewar Tim Flynn Laura Gruber Nancy Hardt Heather Harrell Omayra Marrero, MS-3 Eric Rosenberg Amy Stevens Bob Wears Themes Why develop a UF Patient Safety/Quality Improvement Course… • Now? • For medical students? How did we go about drafting a curriculum? What are we proposing to do in each year – and especially the 3rd year? Why a Patient Safety/QI Course for Students… now? Institutional momentum • Ferrero Case • Influence of faculty trained in QI/safety to organize existing “bits and pieces” Organizational momentum • AAMC – “improving patient safety is our responsibility” (2004) • NSPF (VA), AMA, ACGME National momentum • CMS (“non-payment for non-performance/error”) (some) Preliminary Efforts Sub-I Introductory Lecture and Observed Case reporting (Heather Harrell, Eric Rosenberg) EBM, Clerkship Introductory talks (Rosenberg) Simulation Exercises (Armstrong, others) Students “get it” “my patient came into the ED for presyncope; she was getting Clonidine instead of “Klonipin” for her anxiety” “my patient refused to go to radiology to get a dialysis catheter placed; she was right to refuse -they had come for the wrong patient” “my patient told the team he was on the ‘same med list’ as before… we didn’t review his medications with him, we just recopied the old ones. He didn’t tell us that his cholesterol medication had been changed because he’d had rhabdomyolysis recently… he again developed rhabdomyolysis while on our service.” Table 2. Perceived Importance of Proposed Causes for Adverse Events by Student Discipline and Occasion. Medical Nursing (ABN) Potential Cause of Medical Error Pre (p1) Post (p2) p2-p1 Pre (p1) Post (p2) p2-p1 Overwork, stress, or fatigue on the part of health professionals. 83.0 81.1 -1.9 74.1 59.3 -14.8 Failure of health professionals to work together or communicate as part of a team. 64.2 69.8 5.7 44.4 37.0 -7.4 Understaffing of nurses in hospitals. 54.7 58.5 3.8 59.3 85.2 25.9* Complexity of medical care. 43.4 30.2 -13.2 3.7 7.4 3.7 Insufficient time spent by doctors with patients. 32.1 13.2 -18.9* 18.5 14.8 -3.7 Mistakes made by health professionals. 11.3 17.0 5.7 29.6 29.6 0.0 Poor training of health professionals. 7.5 1.9 -5.7 33.3 44.4 11.1 Poor supervision of health professionals. 1.9 1.9 0.0 3.8 0.0 -3.8 Uncaring health professionals. 1.9 0.0 -1.9 14.8 0.0 -14.8* Poor handwriting by health professionals. 0.0 26.4 26.4* 18.5 22.2 3.7 . Rosenberg, Cooper, Harrell, Menzel, Davidson (2008). How did we go about drafting a curriculum? 8 Task Force Meetings: 12/07 – 5/08 Surveyed published curricula Agreed on multi-year course integrated into existing courses, but with distinct identity, course directors Developed goals and objectives for each year Developed specific activities, options, and themes for each year Curriculum Goals: MS-1, MS-2 Understand patient safety fundamentals including the importance of an organizational culture that promotes teamwork and safety, the public focus on patient safety and adverse events, patient safety terminology, and the human impact of adverse events. Understand key aspects of methods to improve patient safety and clinical quality as well as the interaction between quality improvement efforts in the medical malpractice tort system. Curriculum Goals: MS-3 Recognize and describe adverse event and patient safety challenges unique to different specialties and be able to apply strategies and techniques designed to prevent or mitigate those events. Objectives: MS-3 Identify and analyze common clinical adverse events. Differentiate the impact of system failures and human factors in the development of adverse events and discuss approaches to preventing and mitigating those events. Identify and describe system level improvements which will improve patient safety and reduce adverse events. Identify and be able to apply individual strategies and approaches to improve patient safety and reduce adverse events. Curriculum Goals: MS-4 Demonstrate competence in key patient safety and quality improvement skills and conduct an individual project related to patient safety in the student’s specialty choice area. Patient safety curriculum to be incorporated longitudinally into existing curriculum Pre-orientation Pre-orientation assigned readings on the importance of developing a culture of safety in health care Year 1 • Quality and Safety Grand Rounds on the impact of medical errors on patients and families • Culture of safety workshop at the beginning of the EPC course to discuss the preorientation reading materials and follow up on the discussion questions handed out at the first Quality and Safety Grand Rounds • Epidemiology of medical error online module • Online module on national quality improvement and patient safety organizations • Quality and Safety Grand Rounds on the impact of medical errors on providers Year 2 • QI/PI workshops (at least two) on the application of common performance improvement techniques to a standard problem, including problem statement, process mapping and solution generation. • Multidisciplinary panel discussion on teamwork and communication issues. • Communication workshop that includes a focus on difficult communications and roleplaying around the use of structures communications (i.e., SBAR). • Panel discussion on safety lessons from other disciplines • Lecture on the effectiveness (or lack of effectiveness) of the medical malpractice system as a patient safety tool. • Portfolio reflections on quality and safety observations during the preceptorship experience. Year 3 • Pre-reading (examples of• residents, medical students who have successfully completed • patient safety interventions) • Clerkship CPCs devoted • to quality and safety topics • Workshops on QI • methods • Over time develop a • threaded hypothetical case to be used for • quality CPC across clerkships • Student reflection on errors seen on clerkship • with course directors/quality directors • Student maintains registry of opportunities for clinical improvement • to be discussed with departmental quality directors Year 4 Pre-reading (i.e. How Doctors Think by Jerome Groopman, M.D.) Simulator session: teamwork and spot the error Multi-disciplinary workshops re: communication SBAR Role playing exercise re: delivering bad news Root cause analysis workshop Self-directed individual learning project on future specialty patient safety issues Seminar to reflect on curriculum and identify opportunities to take leadership roles in quality and safety Seminar to reflect on gaps between ideal and optimal care systems vs. actual performance “Quality and Patient Safety: I – IV” Four, year-long segments (analogous to the EPC semester series) Lecture, seminar, online/independent study, reflective writing, clinical simulation activities integrated into existing preclinical and clinical coursework. Collaboration on quality improvement projects aligned with their specialty areas. https://medinfo.ufl.edu/courses/php/content.php Course Directors Eric Rosenberg – UF G’ville Internal Medicine • ACP Patient Safety (2002) – yearly CME program • DOM Physician Director for QI • Medication Safety Bob Wears – UF Jax Emergency Medicine • 1st presentations in 1998 • Faculty in U Wisconsic Human Factors & Engineering in Pt Safety short course X 4 years • Faculty in NWU Master's program in pt safety x 2 years • Multiple funded safety research efforts. • Multiple research publications and book chapters on subject • Editor of Patient Safety in Emergency Medicine Quality and Patient Safety I Online Module I: “The scope and gravity of adverse events” (A. Stevens) Online Module II: “The scope of quality problems in the U.S. medical system” (E. Rosenberg) Quality and Safety Student Grand Rounds I: “The Impact of Medical Harm on Patients and Families” (EPC-1) Workshop I: “Review of Readings and Grand Rounds I” (EPC-1) • “Executive Summary: To Err is Human” (IOM 1999) • “When Doctors Make Mistakes” (Atul Gawande) • Excerpts from executive summaries of IOM/Quality Chasm Reports • “The Nature and Frequency of Medical Errors” (Wachter, Ch 1) QPS I (cont’d) Quality and Safety Student Grand Rounds II: “The Impact of Medical Harm on Physicians and other Medical Professionals” (EPC) Workshop II: “Reflective Writing on Quality/Safety” (EPC-2) Clinical Skills Exam Module Quality and Patient Safety II Online Module III: “Introduction to Root Cause Analysis” Online Module IV: “Introduction to Quality Improvement” Workshop III: “Root Cause Analysis Exercise” (EBM) Workshop IV: “Quality Improvement Concepts” Workshop V: “The Hidden Patient Safety Curriculum: Current Reality on the Wards and in Clinic” / Ethical Issues Surrounding Safety (MS-4, residents, faculty) (Clerkship Orientation 2009; Ethics) QPS II (cont’d) Workshop VI: “Improving Interdisciplinary Communication” (Winter/Crawford) Workshop VII: “Improving Patient Communication: Assessing Barriers to Care” (EPC-3) Lecture I: “The Tort System and its Impact on Quality Improvement” (Ethics; J. Osgard SUF Self Insurance Trust Fund) Quality and Safety Student Grand Rounds III: “Interdisciplinary Communication and Teamwork Challenges” (outside speaker) Quality and Safety Student Grand Rounds IV: “Lessons from Industry” (outside speaker) Clinical Skills Exam Quality and Patient Safety III Students may consider a menu of options to choose from during the year to satisfy requirements We want to encourage a high degree of flexibility. 4 Multidisciplinary “Themes” • Role of Hospital Quality Depts. • Role of Nursing in QI • Avoidance of Medication Errors • Laboratory / Radiographic Errors QPS III Inter-Clerkship Seminar Series: “Case Studies in Patient Safety” • Presentation of Actual/Averted Errors with mock root cause analyses • Presentation/Analyses of Quality Data with discussion of methods of performance improvement Patient Safety Rounds at GAVAMC Clinical Skills Exam Clerkship Directors’ Proposals: June 6, 2008 ER (Jacksonville) • Daily shift-change w/ more student involvement -- focus on safety problems/hand off issues Family Medicine/Neurology • Root cause analysis case conference using errors reported by students on Medicine • Likely to incorporate root cause analysis into existing "doc in box" sessions Surgery • • • Day 1 orientation lecture focusing on surgical complication prevention M&M to focus on root cause analyses Increased involvement of subspecialty rotations OB/GYN • • Creating CPC series on quality/error prevention Incorporate TeamSTEPPS (http://dodpatientsafety.usuhs.mil/index.php?name=News&file=article&sid=31) Pediatrics • Students may identify errors and include as part of portfolio) or work through scenarios in conference geared towards specific pediatrics issues (wt. based dosing, etc.) Psychiatry • Ethics Case Conference series to focus on error prevention Quality and Patient Safety IV Workshop VIII: “Clinical Decision Making: “How Doctors Think” Online Module V: “Disclosing Errors to Patients” Online Module VI: “Anticipating Error to Avert Harm” Simulation Exercises • Harrell Professional Development and Assessment Center • “Disclosing Errors to Patients and Families” • “Discussion of Errors on Rounds” • Operating Room Simulation • “Spot the Error” Exercise (John Armstrong, Jane Carthy) • Anesthesiology simulators • Bedside Procedure Simulation QPS IV (cont’d) Workshop IX: “The Hidden Patient Safety Curriculum (cont’d) Development of CQI Project (with input from Physician Quality Directors) • Research/Write about quality of care issues surrounding a disease, procedure, patient population • Adopt a CQI project; participate in data collection, analysis of ongoing research at SUF Methods of Evaluation Non-credit, required course Attendance at all required course activities Final exam at close of 1st, 2nd, 3rd, (and 4th) year (incorporate into clinical skills exam series if possible) Completion of writing assignments Completion of Quality Improvement Project Who will teach it? We all will. We need more faculty development in this area, but a wide variety of “open source”, practical, case-based materials Many key concepts are intuitive for the experienced clinician • For example, to do a “root cause analysis”: describe the event, identify the immediate cause of the adverse event, identify the contributing causes (latent errors), create an action plan. How will we know if this is effective? Plan continuing evaluation, evolution of the curriculum Administration of surveys to gauge changes in attitudes, knowledge, skills Establishment of more formal curricula in UF residency training programs Impact on institutional culture, patient satisfaction, quality Is it safe to speak up? Speak up scripts “I need clarification” to avoid confrontational speech People may ignore you • Can’t change the world even though the world needs changing There are specific avenues to explore in the longer term – even if people are ignoring you in the short term • We can put you in touch with people interested in fixing this problem – it won’t be business as usual forever There are others to talk to in the hierarchy (dean, chairs, QI directors, clerkship directors) We can ask departments to make a general commitment to respond to those who report problems • • “We’ve made a general commitment to respond in a certain way” “We will engage and not attack people Wears: “perhaps the best test of whether safety culture exists is what happens when a lower status hierarchy person brings up a problem – and they’re mistaken about whose patient it is… if they don’t get beat up, that’s a healthy culture…” Quality is not just meeting Performance Measures “a hospital can be seen as a high quality organization – receiving awards for being a stellar performer and oodles of cash from P4P programs – if all of its “pneumonia” patients receive the correct antibiotics, all its “CHF” patients are prescribed ACE inhibitors, and all its “MI” patients get aspirin and beta blockers. Even if every one of the diagnoses was wrong.” – Bob Wachter