Comprehensive version - Tufts University School of Medicine
advertisement
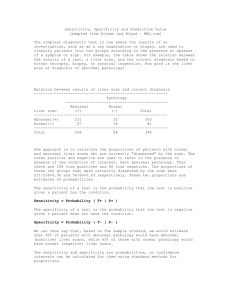
Is it True? Evaluating Research about Diagnostic Tests The Case of Baby Jeff The Case of Baby Jeff CPK testing for Muscular Dystrophy Prevalence: 1 in 5,000 (0.02%) • Sensitivity: 100% • Specificity: 99.98% Prevalence 20 will have=M.D. 1 in 5,00099,980 = .02%– = no20M.D. newborn boys 20 correctly 20 false Sensitivity positive 100% positive 0 false negative 99,960 correctly Specificity 99.98% negative 40 positive tests 99,960 negative tests 50% truly positive 100% truly negative 50% falsely positive 0 falsely negative 50% PPV 100% NPV Negative results Positive results 100,000 newborn boys Why this is important http://today.msnbc.msn.com/id/42829175 Other examples Lyme disease Echocardiogram as part of executive physical • Sensitivity= 95%; specificity= 95% • High prevalence (20%): PPV =83% • Low prevalence (2%): PPV = 28% • Prevalence = 10%; PPV = 50% Technical vs. Clinical Precision Technical precision Clinical precision Sensitivity Positive predictive value The percentage of patients with The percentage of patients with the disease who have a positive a positive test who have the test disease Specificity The percentage of patients without disease who test negative Negative predictive value The percentage of patients with a negative test who are without disease. Predictive Values Positive Predictive Value • The percentage of patients with a positive test who have the disease Negative Predictive Value • The percentage of patients with a negative test who don’t have the disease Let’s practice Task 1. A serum test screens pregnant women for babies with Down’s syndrome. The test is a very good one, but not perfect. Roughly, 1% of babies have Down’s syndrome. If the baby has Down’s syndrome, there is a 90% chance that the result will be positive. If the baby is unaffected, there is still a 1% chance that the result will be positive. A pregnant woman has been tested and the result is positive. 1,000 similar Positive: 90% correctly identified Negative: 99% correctly identified Negative results Positive results Prevalence = 1% = ___ patients/1,000? 1,000 similar Positive: 90% correctly identified Negative: 99% correctly identified Negative results Positive results Prevalence = 1% = ___ patients/1,000? Down’s Syndrome 1,000 similar patients 9Positive: correctly 10 false 90% positive correctly identified positive 1 false negative 980 correctly Negative: 99% negative correctly identified 19 positive tests 981 negative tests 47.5% truly positive 99.99% truly negative 52.5 falsely positive 0.001% falsely negative Negative results Positive results 10 – Downs = 1% = 10 with Prevalence 990 No Downs Downs Task 2 A 45-year-old woman presents with a sore throat and cough but without fever, tonsillar exudate, or cervical nodes. Using a clinical decision rule, you determine her likelihood of having strep throat is 1%. However, according to your office protocol, your medical assistant already has performed a rapid strep (antigen) test, which is positive. What is the likelihood the patient has strep throat now? Antigen test -- Sensitivity: 88% Specific: 96% Strep throat 100,000 similar patients 880 correctly 3,960 false Sensitivity positive 88% positive 120 false negative 95,040 correctly Specificity 96% negative 4840 positive tests 95,160 negative tests 18% truly positive 99.87% truly negative 82% falsely positive 0.126% falsely negative 18% PPV 99.87% NPV Negative results Positive results 1,000 Prevalence – Strep = 1% = 1,000 99,000 with – viral strep Adopting new screening/diagnostic tests Sensitivity/specificity not enough Testing as an intervention • Did the authors study an outcome patients care about? Levels of “POEMness” for Diagnostic Tests 1. 2. 3. 4. 5. Sensitivity & specificity Does it change diagnoses? Does it change treatment? Does it change outcomes? Is it worthwhile (to patients and/or society)? (examples: HbA1C for DM, CPK vs T4/PKU in newborns, electron beam tomography for CAD) Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11:88-94 Screening pulse oximetry for CHD Diagnostic performance of abnormal pulse oximetry for congenital heart defects for all major congenital defects * sensitivity 49.06% * specificity 99.016% * positive predictive value 13.33% * negative predictive value 99.86% for critical congenital defects * sensitivity 75% * specificity 99.12% * positive predictive value 9.23% * negative predictive value 99.97% Lancet 2011 Aug 27;378(9793):785 Screening pulse oximetry for CHD Jaundice, terminating breast-feeding, and the vulnerable child Breast-feeding was more common in the jaundiced group (61% vs 79%). By 1 month, more mothers of jaundiced infants had completely stopped breast-feeding (19% vs 42%). They were more likely to have never left the baby with anyone else (including the father) or left the baby at most one time for less than 1 hour (15% vs 31%), more well-visits, more ED visits (2% v 11%, not including bili measurements). Thus, may increase the risk for premature termination of breastfeeding and for development of the VULNERABLE CHILD SYNDROME. Pediatrics 1989 Nov;84(5):773-8 Naming is not curing In the 1600s, astrology dominated medicine as a healing profession. Neither worked but astrology was much more popular because it focused on fixing people's problems. Medicine, on the other hand, focused mainly on categorizing illnesses (i.e., diagnosing) and not so much on treatment. 400 years later there is still a priority on categorizing, regardless of whether it's helpful. A correct diagnosis is only useful when it results in the selection of a treatment that benefits the patient; otherwise, it's only a label. James Burke. The day the Universe Changed. Boston: Little, Brown and Company, 1985, p. 333. TEST + TEST - Disease No disease True Positive (TP) False Positive (FP) ab cd False Negative (FN) True Negative (TN) Sensitivity TEST + TEST - Disease No disease True Positive (TP) False Positive (FP) ab cd False Negative (FN) True Negative (TN) Specificity TEST + TEST - Disease No disease True Positive (TP) False Positive (FP) ab cd False Negative (FN) True Negative (TN) Positive Predictive Value TEST + TEST - Disease No disease True Positive (TP) False Positive (FP) ab cd False Negative (FN) True Negative (TN) Negative Predictive Value TEST + TEST - Disease No disease True Positive (TP) False Positive (FP) ab cd False Negative (FN) True Negative (TN) Likelihood Ratios Similar to the concepts of “ruling in” and “ruling out” disease Pre Test Odds x LR = Post Test Odds The problem – we don’t think in terms of odds Clinical decision rules: Do the hard math for us, be we need to enter the appropriate data and interpret results II. Are The Results Valid? Diagnostic test compared with the “Gold standard” on all patients Blinded comparison Independent testing Consecutive patient enrollment (adequate spectrum of disease) (Must have all for LOE = 1b) II. Are The Results Valid? What are the results? • • • Sensitivity, specificity and predictive values Likelihood ratio calculation Prevalence of disease in the study population • Typical? • Similar to your practice? Levels of “POEMness” for Diagnostic Tests 1. 2. 3. 4. 5. Sensitivity & specificity Does it change diagnoses? Does it change treatment? Does it change outcomes? Is it worthwhile (to patients and/or society)? (examples: HbA1C for DM, CPK vs T4/PKU in newborns, electron beam tomography for CAD) Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11:88-94