Improving Evidence-Based Care for Heart Failure
in Outpatient Cardiology Practices: Primary
Results of the Registry to Improve Heart Failure
Therapies in the Outpatient Setting (IMPROVE HF)
Gregg C. Fonarow, Nancy M. Albert, Anne B. Curtis, Wendy Gattis
Stough, Mihai Gheorghiade, J. Thomas Heywood, Mark L. McBride,
Patches Johnson Inge, Mandeep R. Mehra, Christopher M. O'Connor,
Dwight Reynolds Mary N. Walsh , Clyde W. Yancy
Fonarow GC et al. Circulation. 2010;122:585-596
Disclosures
• The IMPROVE HF registry is sponsored by Medtronic.
• The sponsor had no role or input into the selection of endpoints or
quality measures used in the study.
• Outcome Sciences, Inc, a contract research organization,
independently performed the practice site chart abstractions for
IMPROVE HF, stored the data, and provided benchmarked quality of
care reports to practice sites. Outcome Sciences received funding
from Medtronic.
• Individually identifiable practice site data were not shared with either
the steering committee or the sponsor.
• Individual author disclosures are provided in the manuscript.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Heart Failure Care in the Outpatient
Cardiology Practice Setting
• There are well documented gaps, variations, and
disparities in the use of evidence-based, guideline
recommended therapies for heart failure in inpatient and
outpatient care settings.
• As a result many heart failure patients may have
hospitalizations and fatal events that might have been
prevented.
• Hospital-based performance improvement programs have
improved the quality of care for heart failure patients.
• Similar programs in the outpatient setting have not been
tested.
Fonarow GC, et al. Circulation. 2010;122:585-596.
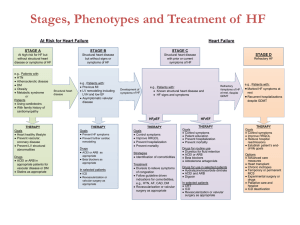
ACC/AHA 2005 HF Guidelines:
Implementation of Guidelines
I IIa IIb III
I IIa IIb III
Academic detailing or educational outreach visits are
useful to facilitate the implementation of practice
guidelines
Chart audit and feedback of results can be effective to
facilitate implementation of practice guidelines
The use of reminder systems can be effective to
facilitate implementation of practice guidelines
I IIa IIb III
The use of performance measures based on practice
guidelines may be useful to improve quality of care
Hunt SA, et al. ACC/AHA 2005 Practice Guidelines. Available at http://www.acc.org.
IMPROVE HF Study Overview
• Largest, most comprehensive performance improvement
study for HF patients in the outpatient setting
• Designed to enhance quality of care of HF patients by
facilitating adoption of evidence-based, guidelinerecommended therapies:
– Evaluate utilization rates of evidence-based, guidelinerecommended HF therapies at baseline and over the course of
the performance improvement intervention (chart audit and
feedback; use of performance measures)
– Multifaceted, practice-specific performance improvement toolkit
including clinical decision support tools (reminder systems)
– Sites attended an educational workshop to set treatment goals
and develop a customized clinical care pathway (educational
outreach)
Fonarow GC et al. Am Heart J, 2007;154:12-38.
Methods: Guideline-Recommended
Quality Measures
• Seven quality measures with strong evidence prospectively selected:
– Angiotensin-converting enzyme inhibitor (ACEI) or angiotensin II receptor
blocker (ARB)*
– ß-blocker*
– Aldosterone antagonist
– Anticoagulation therapy for atrial fibrillation/flutter (AF)*
– Cardiac resynchronization therapy with or without ICD (CRT)
– Implantable cardioverter defibrillator with or without CRT (ICD)
– Heart failure (HF) education*
• Patients deemed eligible for individual quality measure based on
meeting guideline criteria, without contraindications, intolerance, or
other documented reasons for non-treatment.
• Steering committee selected quality measures based on potential to
improve patient outcomes, definition precision, construct and content
validity, feasibility.
* Included as ACC/AHA outpatient HF performance measure, endorsed by National Quality Forum.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Methods: Patient Selection, Practice
Selection, Data Collection and Management
• Patient Inclusion:
– Clinical diagnosis of HF or prior MI
with at least 2 prior clinic visits
within 2 years
– LVEF ≤ 35% or moderate to severe
left ventricular dysfunction
• Patient Exclusion:
– Cardiac transplantation
– Estimated survival <1 year from
non-cardiovascular condition
• Average of 90 eligible patients per
practice randomly selected for
each of 3 study cohorts
• Practices: Outpatient cardiology
(single specialty or multi-specialty)
practices from all regions of the
country
Fonarow GC, et al. Circulation. 2010;122:585-596.
• Data quality measures
– 34 trained, tested chart review
specialists
– Training oversight by study
steering committee members
– Monthly quality reports
– Automated data field range,
format, unit checks
• Chart abstraction quality
– Interrater reliability averaged 0.82
(kappa statistic)
– Source documentation audit
sample concordance rate range of
92.3% to 96.3%
• Coordinating center: Outcome
Sciences, Inc. (Cambridge, MA)
– Individual practice data not shared
with sponsor or steering committee
Methods: Study Objectives
Practice
Level
Patient
Level
Changes for each of the 7 quality measures at 24 months
X
X
≥ 20% relative improvement in 2 or more quality measures at
24 months
X
Xa
Changes in 7 quality measures patients with both baseline
and 24 month data
X
X
Changes in 2 summary care measures at 24 months
X
X
Changes in 7 quality measures in single-time point cohorts
compared with baseline
X
X
Primary Analyses of Quality Measures:
Other Analyses:
a
Pre-specified primary objective
Practice level analysis: proportion of eligible patients receiving therapy for each practice
Patient level analysis: proportion of eligible patients receiving therapy for aggregate of all practices
Fonarow GC, et al. Circulation. 2010;122:585-596.
Methods: Study Design and Patient
Disposition
Baseline
Chart Review
12 Month
Chart Review
24 Month
Chart Review
167 sites
15,177 patients
155 sites
9,386 patients
155 sites
7,605 patients
Longitudinal
Cohort
Process Improvement Intervention (165 sites)
6 Month
Chart Review
18 Month
Chart Review
154 sites
9,992 patients
151 sites
9,641 patients
• Longitudinal cohort included the same patients
reviewed at 3 time points.
• Single-time-point cohorts included separate
patients from the same practices and unique
from the longitudinal cohort, as well as from
each other.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Two SingleTime-Point
Cohorts
Total Sites
Patients Enrolled
Total Chart Reviews
Total # of Site Visits
167
34,810
63,143
782
Methods: Practice Specific Performance
Improvement Intervention
1-day workshop after baseline
data collected
Guideline-based, clinical
decision tool kit*
Web-based quality of care
reports*
Included study goals, guidelines,
intervention tool kit, performance
improvement methods, tips to
promote practice change, effective
use of collected data.
Treatment algorithms, clinical
pathways, standardized encounter
forms, checklists, pocket cards, chart
stickers, patient education materials.
Tools available at
www.ImproveHF.com.
Practice specific reports from chart
audit data with benchmarking
capability.
Bimonthly educational,
collaborative Web based
seminars*
* Use or participation was encouraged but not mandatory. Practices could adopt or modify tools.
Practice Survey:
• 96% adopted one or more performance improvement strategies
• 85% used benchmarked quality reports
• 60% employed one or more IMPROVE HF tools
Fonarow GC, et al. Circulation. 2010;122:585-596.
IMPROVE HF Practice Specific Education
and Implementation Tools
Evidence Based Algorithms
and Pocket Cards
Clinical Trials and
Current Guidelines
Clinical Assessment
and Management
Forms
www.improvehf.com
Patient Education
Materials
Dissemination of best practices:
- Webcasts
- Online Education
- Newsletters
IMPROVE HF Performance Intervention:
Benchmarked Practice Profile Report
Adherence to Guidelines
Practice or
Single
Physician
On-Demand
Performance
Measures
across
all physicians
within practice
Benchmarking
Benchmarking
Capability:
region,
practice,
individual
physician
Patient Characteristics
Characteristic
Age, median, years
Male, %
Race: White, black, unavailable, %
Insured, not documented, uninsured, %
Heart failure origin, ischemic, %
Prior MI, %
History of CABG, %
History of PCI, %
History of atrial fibrillation/flutter, %
History of peripheral vascular disease, %
History of diabetes, %
History of hypertension, %
History of COPD, %
History of depression, %
Fonarow GC, et al. Circulation. 2010;122:585-596.
Longitudinal Cohort
18-Month
All Patients
24-Month
Cohort
N = 15,177
N = 7,605
N = 9,641
70.0
71.0
70.0
71.1
71.3
70.7
42.4, 9.2, 46.7 42.6, 9.0, 46.5 55.9, 11.5, 31.0
92.2, 6.3, 1.2 95.2, 3.7, 1.0 90.6, 7.6, 1.8
65.4
67.0
65.9
40.0
51.7
41.6
31.2
34.1
31.2
25.6
30.0
29.1
30.7
41.2
34.0
11.5
16.0
12.3
34.1
37.8
35.6
62.2
75.1
69.7
16.7
21.8
18.0
9.0
15.7
10.7
Patient Characteristics (Continued)
Longitudinal Cohort
Baseline
N = 15,177
24-Month
N = 7,605
18-Month
Cohort
N = 9,641
34.7, 36.6,
20.7, 2.6, 5.5
38.0, 43.5,
16.4, 1.4, 0.7
32.0, 44.8,
21.1, 1.6, 0.5
LVEF, median, %
25.0
30.0
25.0
Systolic blood pressure, median, mmHg
120
120
120
Diastolic blood pressure, median, mmHg
70
70
70
Resting heart rate, median, bpm
71
70
72
Sodium, median, mEq/L
139
139
139
Blood urea nitrogen, median, mg/dL
22
22
21
Creatinine, median, mg/dL
1.2
1.2
1.2
BNP, median, pg/mL
387
314
373
124
132
122
(n = 10,225)
(n = 3,788)
(n = 7,511)
Characteristic
NYHA I, II, III, IV, unavailable, %
QRS duration, median, ms
Fonarow GC, et al. Circulation. 2010;122:585-596.
IMPROVE HF Practice Characteristics
Characteristic
Census region: South, Northeast, Central, West, Missing, %
Practice setting: University, Non-university teaching, Nonuniversity, non-teaching, % (n=157)
Multispecialty, %
Hospital-based, %
Transplant center, %
Suburban or rural location, %
HF clinic in practice, % (n=163)
HF nurse in practice, %
Device clinic in practice, %
No. of physicians in practice, 1-10, 11-20, >20, %
Number of electrophysiologists in practice, median
Interventionalist in practice, %
Annual number of patients managed by practice, median
Practice Sites (N = 167*)
38.9, 32.3, 15.6, 12.0, 1.2
7.8, 21.6, 64.7
24.0
27.5
9.6
71.3
41.3
34.7
78.4
48.5, 27.5, 18.0
1.0
87.4
1837.5
*Two sites did not provide any survey data. N=165 for these characteristics unless otherwise noted.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Results: Improvement in Quality Measures at 24
Months (Practice Level Analysis)
Longitudinal Cohort
123 of 155 practices (79%) with ≥ 20% relative improvement in 2 or more care measures
Absolute
Improvement
Relative
Improvement
(95% CI)
(95% CI)
P-value
85.1%
(83.4 – 86.8)
+ 6.8%
(4.8 – 8.8)
+ 19.4%
(-1.1 – 39.8)
0.063
86.0%
(84.3 – 87.7)
92.2%
(90.6 – 93.8)
+ 6.2%
(4.8 – 7.6)
+ 7.6%
(5.1 – 10.2)
<0.001
34.5%
(31.5 – 37.4)
60.3%
(56.1 – 64.4)
+ 25.1%
(20.7 – 29.6)
+ 86.5%
(67.1 – 105.9)
<0.001
68.0%
(65.5 – 70.5)
67.8%
(65.0 – 70.7)
- 0.1%
(-3.0 – 2.8)
+ 1.0%
(-3.6 – 5.5)
0.673
CRT-P/CRT-D
37.2%
(32.2 – 42.2)
66.3%
(61.6 – 71.1)
+ 29.9%
(23.6 – 36.2)
+ 124.5%
(85.5 – 163.5)
<0.001
ICD/CRT-D
50.1%
(47.3 – 52.8)
77.5%
(74.8 – 80.1)
+ 27.4%
(24.6 – 30.2)
+ 70.9%
(61.0 – 80.8)
<0.001
HF education
59.5%
(55.7 – 63.2)
72.1%
(68.3 – 75.9)
+ 12.6%
(8.2 – 17.0)
+ 50.6%
(27.1 – 74.2)
<0.001
Baseline
24 Months
(95% CI)
N = 167
(95% CI)
N = 155
ACEI/ARB
78.3%
(76.5 – 80.2)
ß-blocker
Quality Measure
Aldosterone
antagonist
Anticoagulation
for AF
Fonarow GC, et al. Circulation. 2010;122:585-596.
Results: Improvement in Quality Measures at 24
Months (Patient Level Analysis)
Longitudinal Cohort
Prespecified primary objective met: Relative improvement ≥ 20% in 3 quality measures
Absolute
Improvement
Relative
Improvement
(95% CI)
(95% CI)
P-value
86.5%
(85.6 – 87.3)
+ 6.7%
(5.6 – 7.8)
+ 8.4%
(7.0 – 9.7)
<0.001
86.2%
(85.6 – 86.8)
93.6%
(93.0 – 94.2)
+ 7.4%
(6.6 – 8.2)
+ 8.6%
(7.7 – 9.6)
<0.001
34.4%
(32.7 – 36.1)
61.8%
(59.2 – 64.5)
+ 27.4%
(24.3 – 30.6)
+ 79.7%
(70.5 – 89.0)
<0.001
68.6%
(67.2 – 70.0)
69.3%
(67.5 – 71.0)
+ 0.7%
(-1.5 – 2.9)
+ 1.0%
(-2.2 – 4.2)
0.546
CRT-P/CRT-D
37.7%
(35.2 – 40.1)
68.5%
(65.8 – 71.3)
+ 30.9%
(27.2 – 34.5)
+ 81.9%
(72.2 – 91.7)
<0.001
ICD/CRT-D
48.8%
(47.8 – 49.8)
79.1%
(78.0 – 80.2)
+ 30.3%
(28.8 – 31.8)
+ 62.1%
(59.1 – 65.1)
<0.001
HF education
61.8%
(61.0 – 62.5)
70.8%
(69.8 – 71.9)
+ 9.1%
(7.8 – 10.4)
+ 14.7%
(12.6 – 16.8)
<0.001
Baseline
24 Months
(95% CI)
N = 15,177
(95% CI)
N = 7,605
ACEI/ARB
79.8%
(79.2 – 80.5)
ß-blocker
Quality Measure
Aldosterone
antagonist
Anticoagulation
for AF
Fonarow GC, et al. Circulation. 2010;122:585-596.
Results: Improvement in Quality Measures at 24
Months (Patient Level Analysis)
Significant Improvement in 6 of 7 Quality Measures at 12 and 24 Months
Pre-specified Primary Objective Met: Relative Improvement ≥ 20% in 3 Quality Measures
100%
Eligible Patients Treated
*
*
80%
84%
*
87%
*
93% 94%
86%
*
80%
79%
*
60%
*
*
69% 69% 69%
69%
*
62%
*
71%
69%
*
71%
62%
58%
*
51%
49%
40%
38%
34%
20%
0%
ACEI/ARB
ß-blocker
Aldosterone Anticoagulant
Antagonist
for AF
Baseline
Fonarow GC, et al. Circulation. 2010;122:585-596.
12 months
CRT
24 months
ICD
HF Education
* P<0.001 vs. baseline
P-values are for
relative change
Longitudinal Cohort with Complete Follow-up at 24
Months: Modified Intention to Treat Analyses
Patient Level Analysis
Improvement in 6 of 7 Quality Measures
Absolute
Improvement
Relative
Improvement
(95% CI)
(95% CI)
P-value
86.5%
(85.6 – 87.3)
+ 3.5%
(2.3 – 4.8)
+ 4.3%
(2.8 – 5.7)
<0.001
88.5%
(87.7 – 89.2)
93.6%
(93.0 – 94.2)
+ 5.1%
(4. – 6.1)
+ 5.8%
(4.7 – 6.9)
<0.001
Aldosterone
antagonist
35.4%
(32.8 – 38.1)
61.8%
(59.2 – 64.5)
+ 26.4%
(22.6 – 30.1)
+ 74.4%
(63.9 – 84.9)
<0.001
Anticoagulation
for AF
72.2%
(70.3 – 74.1)
69.3%
(67.5-71.0)
- 2.9%
(-5.5 – -0.3)
- 4.1%
-7.7 – -0.5)
0.026
CRT-P/CRT-D
41.2%
(37.4 – 44.9)
68.5%
(65.8 – 71.3)
+ 27.4%
(22.7 – 32.0)
+ 66.5%
(55.2 – 77.7)
<0.001
ICD/CRT-D
54.4%
(53.0 – 55.8)
79.1%
(78.0 – 80.2)
+ 24.7%
(23.0 – 26.5)
+ 45.4%
(42.4 – 48.6)
<0.001
HF education
59.7%
(58.6 – 60.8)
70.8%
(69.8 – 71.9)
+ 11.2%
(9.7 – 12.7)
+ 18.7%
(16.2 – 21.2)
<0.001
Baseline
24 Months
(95% CI)
N = 7,605
(95% CI)
N = 7,605
ACEI/ARB
83.0%
(82.1 – 83.8)
ß-blocker
Quality Measure
Fonarow GC, et al. Circulation. 2010;122:585-596.
Newly Documented Contraindications/Intolerance and Newly
Treated patients at 24 months—Paired Longitudinal Cohort
Newly documented
contraindication/
Intolerance at 24 mo.
in patients initially
eligible at baseline
Newly treated at 24
mo. in patients
initially eligible at
baseline
(N=7,605), %
(N=7,605), %
Newly treated at 24
mo. in patients not
initially eligible at
baseline, but
eligible at 24 mo.
ACEI/ARB
9.8% (699/7138)
7.6% (546/7138)
67.1% (49/73)
ß-blocker
5.5% (381/6905)
6.3% (434/6905)
83.9% (208/248)
16.4% (210/1278)
10.3% (132/1278)
54.2% (396/730)
8.8% (181/2061)
6.9% (143/2061)
58.1% (493/848)
1.8% (12/673)
23.5% (158/673)
59.3% (377/636)
3.9% (198/5028)
15.3% (769/5028)
71.1% (857/1205)
0.0% (0/7605)
26.3% (2003/7605)
0.0% (0/0)
Quality Measure
Aldosterone
antagonist
Anticoagulation
for AF
CRT-P/CRT-D
ICD/CRT-D
HF education
Fonarow GC, et al. Circulation. 2010;122:585-596.
Results: Summary Measures Significantly
Improved at the Patient Level
Composite Score: % of total
indicated quality measures
17% Relative Increase, P<0.001
All or None Care: % of patients
receiving each indicated quality
measure
81% relative increase, P<0.001
43.9%
80.1%
68.4%
24.3%
Baseline
24 months
Patient level analysis
Fonarow GC, et al. Circulation. 2010;122:585-596.
Baseline
24 months
Patient level analysis
Single Time Point Cohorts: Improvement
at 18 Months
Directionally similar, smaller magnitude improvements than longitudinal cohort
Absolute
Improvement
Relative
Improvement
(95% CI)
(95% CI)
81.3%
(80.5 – 82.1)
91.9%
(91.3 – 92.5)
38.0%
(35.8 – 40.3)
69.9%
(68.2 – 71.5)
44.1%
(41.1 – 47.1)
+ 1.5%
(0.4 – 2.5)
+ 5.7%
(4.9 – 6.6)
+ 3.6%
(0.8 – 6.5)
+ 1.3%
(-0.9 – 3.5)
+ 6.4%
(2.6 – 10.3)
+ 1.9%
(0.5 – 3.2)
+ 6.7%
(5.7 – 7.6)
+ 10.6%
(2.3 – 18.8)
+ 1.9%
(-1.3 – 5.1)
+ 17.1%
(6.8 – 27.4)
48.8%
(47.8 – 49.8)
55.9%
(54.7 – 57.0)
+ 7.0%
(5.5 – 8.6)
+ 14.4%
(11.3 – 17.6)
<0.001
61.8%
(61.0 – 62.5)
75.8%
(75.0 – 76.7)
+ 14.1%
(12.9 – 15.2)
+ 22.8%
(20.9 – 24.7)
<0.001
Baseline
18 Months
(95% CI)
N = 15,177
(95% CI)
N = 7,605
79.8%
(79.2 – 80.5)
86.2%
(85.6 – 86.8)
34.4%
(32.7 – 36.1)
68.6%
(67.2 – 70.0)
37.7%
(35.2 – 40.1)
ICD/CRT-D
HF education
Quality Measure
ACEI/ARB
ß-blocker
Aldosterone
antagonist
Anticoagulation
for AF
CRT-P/CRT-D
P-value
0.006
<0.001
0.012
0.237
0.001
Patient level analysis
Fonarow GC, et al. Circulation. 2010;122:585-596.
Study Limitations
• Patient eligibility and utilization rates determined by accuracy and
completeness of medical records and their abstraction
– Reasons for preventing treatment may not have been documented
• Potential for ascertainment bias
– Self-selected cardiology practices, primary care setting not included
• Not randomized—secular trends may have influenced results
• Follow-up not available for all patients
– Practices dropped out, patients died or were lost to follow-up
– Paired analyses revealed similar improvements
• Clinical outcomes could not be evaluated with the design
• Unable to measure use of therapies outside of guidelines
• Relative efficaciousness of intervention components could not be
determined
Fonarow GC, et al. Circulation. 2010;122:585-596.
Conclusions
• IMPROVE HF is the largest outpatient cardiology heart
failure practice performance improvement program.
• Implementation of a defined and scalable performance
improvement intervention may improve the use of
evidence-based, guideline-recommended heart failure
therapies in real-world cardiology practices.
• Study findings may serve as a model for existing and
future performance improvement programs.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Clinical Implications
Implementation of a defined and scalable practice specific
performance improvement intervention enhances use of
evidence-based, guideline-recommended HF therapies
demonstrated to improve outcomes
In all care settings where HF patients are managed,
programs to provide practitioners with useful reminders
based on the guidelines and to continuously assess the
success achieved in providing these recommended
therapies to the patients who can benefit from them should
be implemented
Fonarow GC, et al. Circulation. 2010;122:585-596.
Back-up Slides
Practice-Level Use of Guideline-Recommended Therapies in
the Longitudinal Cohort with Complete Follow-up at 24
Months
N=155 practices
Quality Measure
ACEI/ARB
ß-blocker
Aldosterone
antagonist
Anticoagulation
for AF
CRT-P/CRT-D
ICD/CRT-D
HF education
All-or-none care
Composite care
Baseline
24 Months
Absolute
Improvement
(95% CI)
(95% CI)
(95% CI)
(95% CI)
80.7%
(78.5 – 82.8)
87.9%
(86.1 – 89.8)
34.5%
(30.6 – 38.6)
69.5%
(66.4 – 72.6)
36.8%
(30.7 – 43.0)
54.1%
(51.0 – 57.1)
58.9%
(55.0 – 60.8)
25.5%
85.9%
(84.3 – 87.5)
92.8%
(91.3 – 94.3)
61.8%
(57.6 – 66.0)
68.4%
(65.5 – 71.4)
67.2%
(62.5 – 72.0)
77.7%
(75.0 – 80.4)
72.5%
(68.7 – 76.3)
44.1%
(41.0 – 47.2)
79.6%
(78.1 – 71.1)
+ 5.3%
(3.0 – 7.5)
+ 4.8%
(3.5 – 6.2)
+ 25.1%
(20.6 – 29.6)
–1.1%
(-4.1 – 1.8)
+ 30.4%
(23.5 – 37.3)
+ 24.1%
(22.1 – 26.2)
+ 13.5%
(9.1 – 11.9)
+ 18.6%
(15.4 – 21.7)
+ 10.5%
(9.1 – 11.9)
+ 5.7%
(3.6 – 7.7)
+ 6.6%
(4.5 – 8.6)
+ 88.5%
(65.2 – 111.7)
+ 0.3%
(-5.2 – 5.9)
+ 66.1%
(39.1 – 93.0)
+ 55.5%
(48.8 – 62.2)
+ 53.7%
(30.1 – 77.2)
+ 125.1%
(86.8 – 163.4)
+ 16.7%
(14.0 – 19.4)
(23.4 – 27.7)
69.1%
(67.6 – 70.6)
Fonarow GC, et al. Circulation. 2010;122:585-596.
Relative
Improvement
P-value
<0.001
<0.001
<0.001
0.903
<0.001
<0.001
<0.001
<0.001
<0.001
Odds Ratios for the Use of Guideline-Recommended Therapies in
the Longitudinal Cohort with Complete Follow-up at 24 months
Relative to Baseline in GEE Models
Unadjusted Odds Ratio
Quality Measure
(95% CI)
P-value
Adjusted Odds Ratio
(95% CI)
P-value
ACEI/ARB
1.079 (0.993 – 1.772)
0.0715
1.108 (0.985 – 1.247)
0.0889
ß-blocker
1.680 (1.513 – 1.865)
<0.0001
1.678 (1.474 – 1.910)
<0.0001
Aldosterone
antagonist
1.836 (1.538 – 2.192)
<0.0001
2.102 (1.610 – 2.744)
<0.0001
Anticoagulation
for AF
1.040 (0.952 – 1.135)
0.3873
1.053 (0.949 – 1.168)
0.3302
CRT-P/CRT-D
4.092 (3.167 – 5.286)
<0.0001
6.500 (4.386 – 9.633)
<0.0001
ICD/CRT-D
2.401 (2.243 – 2.571)
<0.0001
2.523 (2.229 – 2.854)
<0.0001
HF education
1.642 (1.540 – 1.750)
<0.0001
1.725 (1.582 – 1.887)
<0.0001
All-or-none care
2.182 (2.049 – 2.324)
<0.0001
2.360 (2.152 – 2.587)
<0.0001
Model controlled for within-patient and within-practice correlations. The multivariate model included all
patient and practice characteristics that were significant at the P < 0.10 level in univariate analysis.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Use of Guideline-Recommended Therapies in the
Longitudinal Cohort at Baseline for the Entire Cohort, and by
Patient status at 24 Months
Quality Measure
ACEI/ARB
ß-blocker
Aldosterone
antagonist
Anticoagulation
for AF
CRT-P/CRT-D
ICD/CRT-D
HF education
Total cohort
(N=15,177)
Alive and with
24-month
follow-up
(N=7,605)
Subsequently
lost to followup
(N=5,003)
Subsequently
died
(N=2,569)
Subsequently
lost or died
(N=7,572)
79.8%
83.0%
79.0%
71.6%
76.6%
(11,165/13,987)
(5,921/7138)
(3,624/4,588)
(1,620/2,261)
(5,244/6,849)
86.2%
88.5%
85.3%
81.1%
83.9%
(11,868/13,772)
(6,109/6,905)
(3,870/4,537)
(1,889/2,330)
(5,759/6,867)
34.4%
35.4%
32.1%
35.9%
33.5%
(987/2,870)
(453/1,278)
(313/976)
(221/616)
(534/1,592)
68.6%
72.2%
65.3%
64.9%
65.1%
(2,910/4,244)
(1,488/2,061)
(835/1,278)
(587/905)
(1,422/2,183)
37.7%
41.2%
36.1%
33.5%
34.9%
(580/1,540)
(277/673)
(174/482)
(129/385)
(303/867)
48.8%
54.4%
41.4%
45.7%
43.0%
(4,799/9,830)
(2,736/5,028)
(1,262/3,048)
(801/1,754)
(2,063/4,802)
61.8%
59.7%
65.1%
61.3%
63.8%
(9,373/15,177)
(4,539/7,605)
(3,259/5,003)
(1,575/2,569)
(4,834/7,572)
Fonarow GC, et al. Circulation. 2010;122:585-596.
Odds Ratios for the Use of Guideline-Recommended Therapies in
the 18-Month Single-Point-in-Time Cohort Relative to the
Longitudinal Baseline Cohort in GEE Models
Unadjusted Odds Ratio
Quality Measure
(95% CI)
P-value
Adjusted Odds Ratio
(95% CI)
P-value
ACEI/ARB
1.079 (1.008 – 1.556)
0.0284
1.036 (0.941 – 1.140)
0.04745
ß-blocker
1.736 (1.580 – 1.907)
<0.0001
1.685 (1.474 – 1.927)
<0.0001
Aldosterone
antagonist
1.107 (0.975 – 1.257)
0.1166
1.018 (0.875 – 1.183)
0.8194
Anticoagulation
for AF
1.063 (0.958 – 1.180)
0.2489
1.025 (0.894 – 1.174)
0.7243
CRT-P/CRT-D
1.334 (1.132 – 1.573)
0.0006
1.361 (1.136 – 1.629)
<0.0001
ICD/CRT-D
1.310 (1.231 – 1.395)
<0.0001
1.269 (1.138 – 1.8415)
<0.0001
HF education
2.024 (1.910 – 2.146)
<0.0001
2.072 (1.894 – 2.267)
<0.0001
All-or-none care
1.552 (1.464 – 1.645)
0.0001
1.684 (1. 568 – 1. 810)
<0.0001
Model controlled for within-practice correlations. The multivariate model included all patient and
practice characteristics that were significant at the P < 0.10 level in univariate analysis.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Eligible Patients for Each Quality Measure
by Cohort
Longitudinal
Baseline
Single Time Point
12 Months 24 Months 6 Months 18 Months
Total patients
15,177
9,386
7,605
9,992
9,641
ACEI/ARB
13,987
7,968
6,183
9,130
8,685
ß-blocker
Aldosterone
antagonist
Anticoagulation
for AF
CRT-P/CRT-D
13,772
8,274
6,608
8,930
8,519
2,870
1,656
1,291
1,862
1,804
4,244
3,219
2,719
2,967
2,951
1,540
1,173
1,096
1,052
1,034
ICD/CRT-D
9,830
6,575
5,331
6,907
6,859
HF education
15,177
9,386
7,605
9,992
9,641
Fonarow GC, et al. Circulation. 2010;122:585-596.
Results: Summary of Baseline Patient
Characteristics
•
•
•
•
•
Mean and median age: 68.7 and 70.0 years
Sex: 71.1% male
Mean LVEF: 25.4%
Ischemic etiology: 65.4%
Comorbidities:
–
–
–
–
Hypertension 62.2%
Diabetes 34.1%
AF 30.7%
Chronic obstructive pulmonary disease 16.7%
• Median blood pressure: 120/70 mm Hg
• Median Creatinine: 1.2 mg/dL
• NYHA functional class: 34.7% Class I, 36.6% Class II, 20.7%
Class III, 2.6% Class IV, 5.5% undocumented
Fonarow GC, et al. Circulation. 2010;122:585-596.
IMPROVE HF Primary Objective
• To observe over the aggregate of IMPROVE HF
practice sites a relative ≥20% improvement in at least
2 of the 7 performance measures at 24 months
compared with baseline
Fonarow GC et al. Improving the use of evidence-based heart failure therapies in the outpatient setting: the
IMPROVE HF performance improvement registry. Am Heart J, 2007; 154:12-38.
Results: Baseline Practice Characteristics
Practice setting (n=157)
Census region (n=167)
South
38.9%
Northeast
7.8%
32.3%
Central
Nonuniversity,
teaching
15.6%
West
Missing
University
21.6%
Nonuniversity,
nonteaching
12.0%
64.7%
1.2%
Physicians in practice (n=167)
1 - 10
48.5%
Other characteristics (n=167)
Not mutually exclusive
Hospital-based
27.5%
Suburban/rural
11 - 20
> 20
71.3%
27.5%
HF clinic
18.0%
Device clinic*
>1 APN
Fonarow GC, et al. Circulation. 2010;122:585-596.
41.3%
78.4%
34.7%
APN, advanced practice nurse.
* n=163
Results: Improvement in Quality Measures at 24
Months (Practice Level Analysis)
100%
*
91% 92%
85%
Eligible Patients Treated
80%
Improvement in 5 of 7 Quality Measures
123 of 155 practices (79%) with ≥ 20% Relative
Improvement in 2 or more Quality Measures
86%
*
82%
78%
*
78%
*
60%
*
68% 68% 68%
70%
69%
66%
60%
72%
60%
56%
50%
48%
40%
37%
35%
20%
0%
ACEI/ARB
ß-blocker
Aldosterone Anticoagulant
Antagonist
for AF
Baseline
12 months
CRT
24 months
N = 167 practices at baseline and 155 practices at 12 and 24 months
Fonarow GC, et al. Circulation. 2010;122:585-596.
ICD
HF Education
* P<0.001 vs. baseline
(P-values for 12 months
vs. baseline not reported)
P-values are for
relative change
Longitudinal Cohort with Complete
Follow-up at 24 Months
Improvement in 6 of 7 quality measures
100%
Eligible Patients Treated
*
*
80%
83%
86% 87%
93% 94%
89%
*
72% 71%
*
60%
79%
†
69%
69%
69%
62%
60%
71%
60%
54%
52%
40%
*
73%
*
41%
35%
20%
0%
ACEI/ARB
ß-blocker
Aldosterone Anticoagulant
Antagonist
for AF
CRT
Baseline 12 months 24 months
Patient level analyses
Fonarow GC, et al. Circulation. 2010;122:585-596.
ICD
HF Education
* P<0.001 vs. baseline
† P=0.026 vs. baseline
P-values are for
relative change
Single Time Point Cohorts: Quality
Measures at 18 Months
Directionally similar, smaller magnitude improvements than longitudinal cohort
100%
Eligible Patients Treated
*
†
80%
90% 92%
86%
80% 81% 81%
*
76%
69% 69% 70%
68%
60%
*
54%
*
‡
40%
34%
37% 38%
62%
56%
49%
44%
38% 38%
20%
0%
ACEI/ARB
ß-blocker
Aldosterone Anticoagulant
Antagonist
for AF
CRT
Baseline 6 months 18 months
Patient level analyses
Fonarow GC, et al. Circulation. 2010;122:585-596.
ICD
HF Education
* P ≤ 0.001 vs. baseline
† P = 0.006 vs. baseline
‡ P = 0.012 vs. baseline
P-values are for
relative change
Results: Summary Measures at Practice
Level
Composite Score: % of total indicated quality
measures provided
All-or-None Care: % of patients receiving each
indicated quality measure
345.5% relative increase, p < 0.001
19.2% relative increase, p < 0.001
68.7%
75.2%
67.1%
23.5%
Baseline
(n=167)
24 months
(n=155)
Practice level analysis
Fonarow GC, et al. Circulation. 2010;122:585-596.
Baseline
(n=167)
24 months
(n=155)
Practice level analysis
Baseline Quality of Outpatient HF Care
Conformity with Quality Measures at Baseline
100%
CRT-D
Eligible Patients Treated
86.2%
80%
CRT-P only
ICD only
79.8%
68.6%
61.8%
60%
48.8%
40%
37.7%
34.4%
31.7%
31.4%
20%
17.2%
6.3%
0%
ACEI/ARB
N=
11,165/
13,987
Beta-blocker
11,868/
13,772
Aldosterone
Antagonist
987/
2,870
Anticoagulation
for AF
2,910/
4,244
CRT
ICD
580/
1,540
4,799/
9,830
HF education
9,373/
15,177
Methods: Study Design and Patient
Disposition
34,810 patients enrolled • 167 total sites • 63,143 chart reviews
Baseline
Chart Review
12 Month
Chart Review
24 Month
Chart Review
167 sites
15,177 patients
155 sites
9,386 patients
155 sites
7,605 patients
Longitudinal
Cohort
Process Improvement Intervention (165 sites)
6 Month
Chart Review
18 Month
Chart Review
154 sites
9,992 patients
151 sites
9,641 patients
• Longitudinal cohort included the same patients
reviewed at 3 time points.
• Single-time-point cohorts included separate
patients from the same practices and unique
from the longitudinal cohort, as well as from
each other.
Fonarow GC, et al. Circulation. 2010;122:585-596.
Two SingleTime-Point
Cohorts
Longitudinal Cohort Patient Disposition
Longitudinal cohort baseline
Died
Did not complete 24 mo FU
From practices without 24 mo FU
Status unknown
Alive with 24 mo FU
FU, Follow Up
15,177
- 2,569
- 1,446
- 1,049
- 2,508
7,605
IMPROVE HF Performance Improvement
Tools
• As part of an enhanced treatment plan, IMPROVE
HF provided evidence-based best-practices
algorithms, clinical pathways, standardized encounter
forms, checklists, pocket cards, chart stickers, and
patient education and other materials to facilitate
improved management of outpatients with HF.
• The materials can be downloaded from
www.improvehf.com
• The materials are also included in the Circulation
online-only Data Supplement
Fonarow GC, et al. Circulation. 2010;122:585-596.