Multiple Sclerosis - National Association of Disability Examiners
advertisement

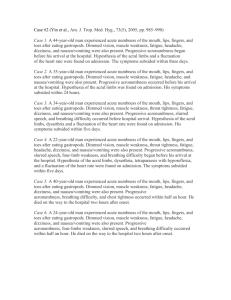
Multiple Sclerosis Diagnosis, Treatment, Disability J. Scott Pritchard, DO NADE National Training Conference - 2011 History • Other clinical names-encephalomyelitis disseminata -disseminated sclerosis • First described by Jean-Martin Charcot in 1868 – Charcot’s triad • Anecdotal histories suggest the disease has been recognized since 1200 - Halldora • First well documented case – Sir Frederick D' Este’s personal diary 1822 - 1846 • Inflammatory auto-immune disease affecting the fatty myelin sheaths of the brain/spinal cord axons • Demyelination and remyelination • Scarring – Sclerosis (plaques/lesions) • Loss of conduction – electrical signal • Genetic, environmental and infectious etiologies have been suggested • Progressive and incurable Great Mimic • The initial symptoms are varied, vague and extremely difficult to link to a specific cause • Numbness, tingling, muscle weakness, changes in cognition, nystagmus, optic neuritis, diplopia, difficulty swallowing or speaking, unexplained fatigue or depression • Symptoms often increased with stress or increased heat (Uhthoff’s phenomenon) exercise or environmental Physical examination • Often very non-focal. Mild motor weakness. Nondermatomal sensory loss • Lhermitte’s phenomenon • Optic Neuritis • INO-intranuclear ophthalmoplegia • Myelopathy-seen with transverse myelitis • Motor weakness. Fatigability of muscles with activity. Generalized fatigue • Spasticity – Ashworth scale – zero to four (severe) • Ataxia • MMSE Clinical testing • SSEP/VEP - evoked potentials • +CSF for increased IgG synthesis and oligoclonal bands • MRI-brain/spinal cord w/gadolinium • McDonald ‘s criteria-clinical, laboratory and radiographic evidence • NPS • Myelin Basic Protein- CSF • NMO antibodies Classification of MS • Relapsing-remitting-periods of clinical worsening that resolves with time. However, baseline function is not restored • Secondary progressive (galloping MS) • Primary progressive-later onset w/minimal recovery • Progressive relapsing-progressive decline with superimposed attacks (Devic’s dz) Treatment • The goal of all therapies is slow disease progression. • Inflammation – Solu-Medrol • Immunomodulation – Avonex/Rebif, Betaseron, Copaxone (ABC therapies) • Antineoplastics – Mitoxantrone • Monoclonal AB - Natalizumab (Tysabri) New Treatments • • • • • Extavia- Interferon -generic Cladribine- antineoplastic Rituximab- biologic agent-antineoplastic Myelin Basic Protein Supplement Oral therapies recently released 1. Ampyra – Improves gait in RR MS 2. BG – 12 - RRMS 3. Gilenya – decreases freq/severity Disability • 25 foot walk testnormal- 5 seconds- men - 6 seconds- women • EDSS-Expanded Disability Status Scale Steps from 0-10-Inviduals 1.0-4.5 are fully ambulatory. 5.0-9.5-increasing ambulatory impairment. 10-Death A claimant with an EDSS of 5.0 or > would typically be disabled. Listings • 11.09 A - Reference listing to 11.04 B • 11.09 B - Reference to listings 2.02,2.03,2.04 and 12.02 • 11.09 C –Reproducible, substantial motor weakness w/repetitive use or movement SSR 96 – 8p • DI 24510.057 • Sustainability of an RFC – consider the functional impact of fatigue and pain • Is the claimant able to sustain a 40 HR work week? Case Studies • 57 y/o clt. 1970- numbness of the face and double vision. 1982-RLE numbness that spread to the LLE not relieved by surgery.1983 OS visual loss w/Lhermitte’s phenomenon. Subsequent years intermittent numbness, diplopia. 1993 major exacerbation with difficulty walking. These episodes progressed to present. She reports mild impairment to mobility and ADL’s. Profound fatigue. #2 • 62 y/o clt. Onset of symptoms 1997. On Copaxone from 1998-2002. Four courses of Mitoxantrone. 2002-2003. Progressive weakness and fatigue. Last major relapse 2005. MRI’s document increasing plaque burden in the thoracic cord. • 25 foot walk-11 seconds with a walker • Progressive weakness in the afternoon #3 • 54 y/o clt – onset of R optic neuritis followed by L hemiparesis • Deep demyelinating lesion R hemisphere and cervical spine at C3 • Weakness occurs after walking 10-15 minutes • Spasticity of the LUE/LLE and 3/5 motor • Wide based gait and decreased RAM LUE #4 • 38 y/o clt – initial bout of optic neuritis at age 26. No other symptoms/clinical findings until the acute onset of midthoracic and abdominal pain. MRI documents a T12 lesion in the spinal cord A complete work-up rules out all other etiologies for her pain. Dx neuropathic pain secondary transverse myelitis at T12 All modalities to relieve pain were ineffective. Thank YOU !!!! Acknowledgements • Movies from the Neurologic Exam and PediNeurologic Exam were used with the permission of Paul d. Larsen, MD., University of Nebraska Medical Center and Suzanne S. Stensass, PhD. University of Utah School of Medicine. Additional materials were drawn from resources provided by Alejandro Stern, Stern Foundation, Buenos Aires, Argentina, Kathleen Digre, MD., University of Utah and Daniel Jacobson, MD., Marshfield Clinic, Wisconsin. The movies are licensed under a Creative Commons AttributionNon-commercial ShareAlike 2.5 license