Gut Health Presentation
advertisement
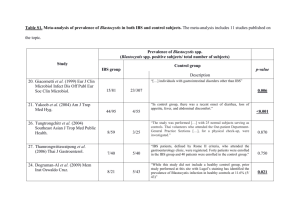
Gastrointestinal Balance: Do you have the guts for health? Mark Pettus MD, FACP February 18, 2014 I want to achieve immortality not through my work … I want to achieve it through not dying. Woody Allen The Proposition • All health and disease are byproducts of complex individualized geneenvironment interactions that may go back more than a generation before conception and continue throughout our lives. • Your genes i.e., your “Book of Life” have a Stone Age imperative, not often compatible with 21st century environmental inputs. • This incompatibility creates a distorted metabolic trajectory that forms the basis of chronic complex disease. • Through epigenomic alteration, our gene expression patterns can be profoundly modulated to promote optimal function and health. • This remains possible throughout life by aligning one’s environmental inputs with that which your genes are best suited for…this is the exit to a healthy life. Learning Objectives Examine the role that gastrointestinal health plays in the broader context of health, dis-ease, and quality of life. Explore the connection between gastrointestinal health, your gut’s ecosystem, inflammation-immune regulation, and your nervous system. Examine environmental inputs that lead to “leaky-ness” or increased permeability in the gut. Review the “4R-Model” for gastrointestinal health Digestive Disease in America Impacts 60-70% Americans GERD effects 45-60 million 7-10% Americans experience heartburn at least daily 20% (60 million) experience at least once monthly Irritable bowel disease (IBS) effects 30-45 million Gallstone disease 20-25 million Diverticular Disease 20 to 40 million Celiac estimated at 3 million (approx 1:100) Gluten sensitivity as much as ? 10% of Americans IBD 750,000 – 1 million Colorectal Cancer approximately 260,000 The IMS reports that Americans spent $307 billion on prescription drugs in 2010. The 10 drugs on which we spent the most were: •Lipitor, a cholesterol-lowering statin drug -- $7.2 billion •Nexium, an antacid drug -- $6.3 billion •Plavix, a blood thinner -- $6.1 billion •Advair Diskus, an asthma inhaler -- $4.7 billion •Abilify, an antipsychotic drug -- $4.6 billion •Seroquel, an antipsychotic drug -- $4.4 billion •Singulair, an oral asthma drug -- $4.1 billion •Crestor, a cholesterol-lowering statin drug -- $3.8 billion •Actos, a diabetes drug -- $3.5 billion •Epogen, an injectable anemia drug -- $3.3 billion Gut Health Immune/Inflammation Mind-Brain-Body Problems with gut health can promote/worsen… Allergy Asthma Autoimmunity Arthritis Metabolic Bone disease Skin problems Mood disorders Dementia Cancer Inflammation IBS associated with: • • • • • • • • GERD Interstitial cystitis Fibromyalgia Chronic Fatigue Syndrome Disrupted sleep Rosacea Migraine headaches Restless leg syndrome (RLS) GERD: Do we have all wrong? Celiac and gluten sensitivity associated with: Thyroid disease Neurologic diseases Osteoporosis Decreased fertility Recurrent UTIs Autoimmune disease Skin disorders e.g. eczema, rosacea RLS – restless leg syndrome David Relman MD Clin Prof Med-ID, Prof Microbiology-Immunology Stanford Ecology of human indigenous microbiology and relationship to health and disease. Irritable Bowel Syndrome Most common GI functional disorder diagnosed by gastroenterologists affecting about 5-10% of the population with female predominance of 2-3:1 Symptom complex including abdominal pain, altered bowel function, bloating, mucosal inflammation, exaggerated stress response, increases in plasma pro-inflammatory cytokines Stress (including early life stress) plays a major role in the onset and exacerbation of symptoms in IBS Recent studies have shown that there may be a brain-gut axis dysfunction involved in IBS Treatment options for IBS are symptom based and include: – Laxatives – Loperamide (Imodium) – Antispasmodics – Antidepressants – Serotonin receptor agonists/ antaginsts Increased Intestinal Permeability And molecular trafficking Common causes of increased intestinal permeability SAD: High animal fat, animal protein, high-sugar, low-fiber, processed diet Overuse of medications such as NSAIDs, antibiotics, acid blockers, steroids e.g. prednisone, chemotherapy Food sensitivities - allergies Low-grade bug imbalances (dysbiosis) involving yeast, bacterial overgrowth (SIBO) Toxins e.g. BPA, pthalates, pesticide residues Stress or the brain-gut connection Alcohol Stress and the gut Stress Activation of the HPA axis (ie CRF, ACTH, cortisol) • Increase in gut permeability • Increase in mucosal inflammation • Changes in GI motor function • Changes in gut flora The 4R Model Remove • Foods that one may be intolerant to (elimination diet: start with gluten and dairy). • Medications that may negatively influence an optimal GI environment (such as PPIs, H2 blockers, NSAIDs, antibiotics, steroids). • For IBS or persistent dyspepsia, consider SIBO and treat with xifaxin 200 mg, two tabs twice daily for 10-14 days • Consider a 2-4 week trial with Diflucan for yeast • Stress: how we interpret and respond Replace For persistent dyspepsia, indigestion, or long-term use of stomach acid suppression consider digestive enzymes to promote better macronutirent breakdown. These are usually plant-based (papaya, pineapple) compounds e.g. bromelain taken with each meal. Re-populate • Administer probiotics from the following three families that have been found to be beneficial for GI function: Bifidobacteria, Lactobacilli, and Saccharomyces. • Administer prebiotics (food that promotes beneficial bacterial growth) such as bananas, Jerusalem artichoke, onions, asparagus and garlic, whole grains. • Target at least 20-30 billion cfus/day Repair…nutritionally Eat whole, fresh, unprocessed foods-seasonal, organic, and local Fiber supports gut flora Avoid common food allergens Eat foods that taste good and allow your taste buds time to get used to new foods Eat in rhythm with meals scheduled at regular intervals throughout the day Eat in a mindful, relaxed state Stay a little hungry Eat foods YOU prepare Repair • Fiber: Consider psyllium or guar gum, 1 tsp in 8-10 oz of water before each meal if not getting enough fiber. • Whole Food Nutrition: Incorporate a hypoallergenic, nutrient rich diet. • Regular Exercise. • Zinc carnosine: 25-30 mg a day for one month. • Omega-3 fatty acids (EPA/ DHA) and/or Gamma Linolenic Acid (Evening primrose Oil, Borage Oil or Black Currant Oil):Total of 2 gms daily for one month. • L-Glutamine Powder: 5 gms twice daily for one month. Relaxation Supplements with some supportive research • • • • • • • • • • Aloe Vera juice – 3 oz. twice daily dgl-Licorice for GERD – 500mg chewtabs with meals Digestive enzymes – 1-2 caps with meals O-3 fish oils 4-6 grams/day EPA/DHA Ginger – 1,000 to 2,000 mg daily Glutamine 500-1,000 mg with meals Magnesium citrate or glycinate 400 – 800 mg daily Melatonin – 3-6 mg at bedtime for GERD Zinc carnosine 15-30 mg daily Vitamin D: 1,000 – 4,000 u/day to keep levels 40+ Thank you.