Initial Therapy - MCE Conferences
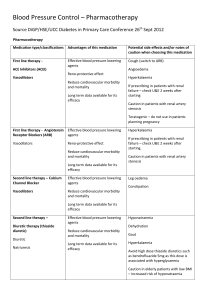
advertisement

Evaluation and Treatment of Hypertensive Patients Herbert L. Muncie, Jr., M.D. Proper technique to measure Blood Pressure (JNC VII) Sitting, back supported, arm at level of heart Feet on floor, legs uncrossed Rest at least five minutes Proper cuff size (> 80% of arm with bladder) Inflate & palpate radial pulse to approximate BP – deflate cuff Inflate 20-30 mm above palpable systolic Measure Korotkoff I (onset sounds - systolic) and V (disappearance sounds - diastolic) WatchBP Office Question A 58 year old African American female with three separate BP readings averaging 164/92. According to JNC VII, what is her BP classification? a) b) c) d) Normal Prehypertension Stage 1 hypertension Stage 2 hypertension Classification of Blood Pressure – JNC VII Systolic Normal < 120 Prehypertension 120-139 Hypertension Stage 1 140-159 Stage 2 > 160 And Or Or Or Diastolic < 80 80-89 90-99 > 100 Highest value (systolic or diastolic) determines Stage Treat Prehypertension? It is not a disease category (JNC VII) Treatment with ARB (candesartan) for 4 years Relative risk reduction of developing Stage 1 hypertension 15.6% Patients with prehypertension are not candidates for drug therapy (JNC VII) Lifetime Risk For men or women who are normotensive at age 55 or 65 and Who survive to age 80 - 85 90% will develop hypertension Tests after Initial Diagnosis Target organ damage? ECG Urinalysis CBC BUN & creatinine Secondary causes? Electrolytes, calcium Other cardiovascular risk factor? Lipid profile, glucose Whom to consider evaluating for 2o causes Onset of hypertension before age 30 or after age 55 Initial diastolic BP is > 110 mm Patient with unexplained hypokalemia Patient with resistant or difficult to control BP especially if initially good control Signs of Cushing’s disease Signs or symptoms of pheochromocytoma Pheochromocytoma Measure plasma free metanephrine (99% sensitive, 89% specific) < 61 ng/L excludes diagnosis > 236 ng/L confirms diagnosis If 62 - 235 ng/L more testing required 24 hour urine metanephrine alone highly sensitive and specific, but often incomplete collection Renal artery stenosis Abdominal bruit suggestive often absent If high index of suspicion & normal renal function [Hartman 2009] MRA CTA If high index of suspicion & diminished renal function MRA Duplex Doppler ultrasonography Primary hyperaldosteronism Screen with plasma aldosterone/renin ratio (cutoff > 25) β-blockers & DHCCBs stop for 2 weeks Spironolactone & loop diuretics stop for 6 weeks Plasma aldosterone should be > 20 ng/dL to make the diagnosis (Nl – 2 – 16 ng/dL – supine) Renin – nl 12 – 79 mu/dL (supine) Cushing Syndrome 24 hr urine free cortisol useful screening (cutoff > 90 mcg/day) Sensitivity 41 – 70% Specificity – almost 100% Overnight dexamethasone suppression test equally sensitive, less specific 1 mg dexamethasone midnight – plasma cortisol next morning (cutoff > 100 nmol) What if you find a o 2 Cause? Renal artery stenosis For atherosclerotic etiology Medical therapy is cornerstone [Dworkin 2009] Stenting no better than medical but more complications May be helpful with recurrent CHF or pulmonary edema For fibromuscular dysplasia – balloon angioplasty is worthwhile White coat hypertension White coat hypertension Elevated office BP but normal outside office Normal would be either 24-hour BP with mean < 125/79 or home BP < 132/82 If out of office BP consistently < 130/80 & no evidence of target organ damage 24 hour monitoring or drug therapy can be avoided (JNC VII) Increased risk of progressing to sustained hypertension [Mancia 2009] Masked hypertension Masked hypertension Normal office BP but elevated outside office Suspect if patient with normal office BP has cardiovascular event Increased risk of cardiovascular events Pharmacotherapy is indicated Deserves “an aggressive diagnostic & therapeutic approach” [Messerli 2007] Mrs. Jones Mrs. Jones is a 58 year old white female treated for hypertension for the past 6 years. Her BP today in the office is 168/94. Which number should you focus on in deciding on modifying treatment? a) b) Systolic BP Diastolic BP Treatment of Patients > 50 y.o. Patients > 50 years old achieve diastolic goal when systolic goal achieved Focus on systolic control for patients > 50 years old because: Systolic BP continues to rise with age Diastolic BP levels off around age 50 & will remain at that level or fall after age 50 Non-pharmacologic Therapy Weight reduction alone reduces BP Regardless of weight - DASH diet helpful in lowering BP Increase potassium (6-8 fruits or vegetables a day) Increase fiber with whole grains (breads, cereals) Increase calcium intake (low fat dairy) Decrease salt (DASH-low Na) No added salt Non-pharmacologic Therapy Stage 1 can be treated with lifestyle only (JNC VII) For one year if no other risk factors For 6 months with other risk factors You do not have to start medication immediately with Stage 1 (BP < 160/100) Audience Question Patients who successfully lose 3 - 9% of their body weight with lifestyle changes can expect to see their average BP decrease how many mm? a) b) c) d) 3 5 7 10 Weight loss & BP - EBM Dieting to lose weight may lower BP in overweight people but the effects are modest & dieting may not be effective alone Cochrane Review 18 randomized trials found weight loss of 3-9% Associated with decreases of roughly 3 mmHg systolic & diastolic http://www.chochrane.org/reviews/en/ab000484.html Lifestyle changes Combining intensive lifestyle counseling & physician feedback was not successful longterm (18 month) in achieving BP control [Svetkey 2009] Some early success (6 months) faded over time Dietary choices influence control success Salt restriction is central especially in those requiring intensive pharmacotherapy Increase fresh fruits & vegtables Maximum 1 restaurant meal/week Question A 50 yo African American male with BP 155/95 (avg.) requires initiating drug therapy. What would be your initial choice of medication class for this patient? a) b) c) d) e) Thiazide diuretic Calcium channel blocker (CCB) Beta blocker Angiotensin-converting enzyme inhibitor (ACE) Angiotensin receptor blocker (ARB) Initial Therapy JNC VII – a thiazide-type diuretic should be initial therapy unless compelling indication Most patients with Stage 1 will experience better BP control & lower CVD risk when taking a thiazide-type diuretic Most patients with Stage 2 disease will experience better BP control & lower CVD risk when taking a multidrug regimen that includes a thiazide-type diuretic Initial Therapy No treatment alters the natural progression of the disease BP will continue to rise as the patient ages regardless of which medications are used Therefore, every patient will eventually need for more than one medication to control their BP Initial Therapy Dr. Chobanian (Chair JNC VII) now suggests flexibility in choice of initial drug [Chobanian 2009] – he suggests Stage 1 – ACE, ARB, CCB or diuretic Stage 2 – two of those 4 drugs to start With exception of β-blockers after an MI & CCBs effect on CVA risk, all drugs lowered CVD events for a given reduction in BP [Law 2009] Initial Therapy To increase drug persistence & compliance with therapy [Friedman 2010] Choose medications that will lower BP with few complications & is taken less often Persistence is lower with more side effects Compliance is lower in males, lower SES groups & in urban environments Question A 50 yo African American male with BP 155/95 (avg.) requires initiating drug therapy. What would I choose? a) b) c) d) e) Thiazide diuretic Calcium channel blocker (CCB) Beta blocker Angiotensin-converting enzyme inhibitor (ACE) Angiotensin receptor blocker (ARB) STITCH Therapy Simplified Treatment Intervention to Control Hypertension (STITCH) STITCH vs Canadian Hypertension Education Program guideline (CHEP) CHEP is similar to JNC VII approach STITCH Treatment Initiate therapy with ½ tablet of low dose combination - diuretic & ACEI or ARB Increase that combination to highest dose tolerated Then add CCB & increase to highest tolerated dose Then add non-first-line agents Alpha-blocker Beta-blocker Spironolactone STITCH Therapy At 6 months [Feldman 2009] 64.7% controlled on STITCH 52.7% controlled on CHEP (P = 0.03) Pharmacologic Efficacy Average reduction in BP for major classes of drugs At standard dosage - 9.1 mm (SBP)/5.5 mm (DBP) drop With half standard dosage 7.1 mm (SBP)/4.4 mm (DBP) When BP > 20 (SBP) or 10 mm (DBP) above goal (Stage 2) start two medications initially Question A 52 year old African American female has not achieved BP control on diuretics. You add an ACE inhibitor to the regimen. You order electrolytes, BUN and creatinine in 1 week. Her creatinine increased from 0.9 baseline to 1.14 mg/dL, a 26.7% increase. What should you do about her ACEI? a. b. c. d. Discontinue the ACEI & add a different class Reduce the ACEI dose 50% Reduce the ACEI dose 25% Make no change in the ACEI dosage Initiating Therapy – Change in Renal Function After initiating treatment, common to get decline in renal function If ≤ 30% non-progressive increase in creatinine Represents a functional response (reduced intraglomerular pressure) & no change in treatment required This response is associated with long-term renal protection If > 30% increase in creatinine, D/C medication & choose another class Question A 52 year old African American female has not achieved BP control on diuretics. You add an ACE inhibitor to the regimen. You order electrolytes, BUN and creatinine in 1 week. Her creatinine increased from 0.9 baseline to 1.14 mg/dL, a 26.7% increase. What should you do about her ACEI? a. b. c. d. Discontinue the ACEI & add a different class Reduce the ACEI dose 50% Reduce the ACEI dose 25% Make no change in the ACEI dosage Diuretic - Classes Thiazide Hydrochlorothiazide (HCTZ) dosage best if ≤ 25 mg & preferably 12.5 mg Outcome benefits have not been established for these dosages of HCTZ Increasing to 50 mg minimally lowers BP further but significantly increases side effects Hyponatremia & hypokalemia more common in women 12 combinations with HCTZ available Diuretic - Classes Thiazide Chlorthalidone 25 mg provided better 24 hr BP control than HCTZ 50 mg Milligram for milligram twice as potent as HCTZ Outcome data available regarding reduced CV events Only 2 combinations available Chlorthalidone/clonidine (Clorpres®) – 15/0.1,0.2, 0.3 Atenolol/chlorthalidone (Tenoretic®) – 25/50, 25/100 Diuretic - Classes Loop If only treating hypertension - use loop diuretics only with renal insufficiency (CrCl < 30 - 40 ml/min) Discontinue thiazides at this CrCl – not effective Dosage frequency for BP treatment Furosemide (Lasix®) – BID QD dosage may lead to reactive Na+ retention mediated by renin/angiotensin system Torsemide (Demadex®) – QD Diuretic - Classes Potassium sparing Combined with thiazide - reduces risk sudden death and hypokalemia Do not combine with continuous K+ supplements or give with renal insufficiency Increased risk hyperkalemia Especially with ACE or ARB combination Should be stopped temporarily if diarrhea or vomiting occurs Selective aldosterone receptor antagonist Eplerenone (Inspra®) first approved in new class Primary focus in heart failure Add-on to anti-hypertensive Rx Side effects Hyperkalemia Contraindicated with hyperkalemia, creatinine > 1.8 men, > 2.0 women, or creatinine clearance < 50 ml Caution in use with ACE or ARB Diuretics – diabetes & hyperlipidemia? Diuretics can raise glucose & lipid levels short-term However, no long-term adverse effects in diabetics Fasting glucose increases in older adults regardless antihypertensive drug Diuretics may be safely used in patients with diabetes or hyperlipidemia Beta-Blockers Available evidence does not support their use as 1st line treatment alone Weak effect in reducing CVA Absent effect on CAD [Wiysonge - Cochrane 2007] Lower heart rate with beta-blocker therapy associated with increased risk CV events & death Compelling indications (JNC VII) Heart failure Chronic stable angina Post MI Tachyarrhythmia Beta-Blockers Side effects Increased risk developing type 2 DM Decreased exercise tolerance Increased risk of Raynaud’s phenomenon Increased insomnia & risk of delirium Abrupt withdrawal can precipitate myocardial ischemia in at risk patients Beta-Blockers & Diabetes In diabetics beta-blockers blunt heart rate & BP response to hypoglycemia However, no increase in severe hypoglycemia in Type 1 or Type 2 DM Do not worsen glycemic control when used with ACE/ARB Carvedilol (Coreg®) & nebivolol (Bystolic®) have neutral or even favorable effect on CHO & lipid metabolism Angiotensin-Converting Enzyme (ACE) Inhibitors Compelling indications (JNC VII) Heart failure Post MI - systolic dysfunction Diabetics with proteinuria Reduce cardiovascular & all-cause mortality As effectively as diuretics, β-blocker or CCB [SOR-A] Diabetics may retain sodium Add diuretic to enhance response ACE Inhibitors Side effects Cough (5-15%) - women 2x men’s risk Angioedema (0.1-0.2%) – African Americans and Asians 3 - 4 x risk increase Hyperkalemia with renal insufficiency If patient has bilateral renal artery stenosis Can cause renal insufficiency Measure creatinine initially & one week after starting ACE If > 30% increase in creatinine or hyperkalemia 1st 2 months – D/C ACE Angiotensin Receptor Blocker (ARB) Three trials found ARBs effective in reducing CV events (LIFE, SCOPE, VALUE) But not as effectively as ACE Reduce the risk end-stage renal disease in diabetics No evidence reduce mortality in diabetics with renal disease Reserve for patients who cannot tolerate ACE Angiotensin Receptor Blocker (ARB) Low incidence of dizziness or other side effects Cough not a problem Caution with renal insufficiency or K+ supplements Angiotensin Receptor Blocker (ARB) Less effective if high salt intake Measure serum creatinine initially & 1 week after starting drug Can worsen renal failure Not proven to improve survival post MI ACE & ARB should not be used in pregnancy Combining ACE & ARB CHARM-Added trial found combination reduced CV events & mortality in patients with heart failure However, in patients without heart failure Combination lowered BP without CV benefit over ACE alone (ONTARGET) But did increase hypotension, syncope & renal dysfunction Ca-Channel Blockers (CCB) More effective in African Americans than diuretic or ACE as initial therapy ALLHAT – if African American cannot take diuretic – CCB preferred initial drug Greater risk CVA, CHD, CVD, angioedema with ACE Combination of benazepril/amlodipine was more effective slowing progression of renal disease than benazepril/HCTZ (ACCOMPLISH trial) Ca-Channel Blocker Risks CCB & diuretics are associated with best stroke prevention Could be due to less visit-to-visit variability Caution combining non-dihydropyridine CCB (diltiazem; verapamil) with beta blocker Potential additive negative inotropic effect Can cause heart failure or complete heart block Direct Renin Inhibitor Aliskiren (Tekturna®) Monotherapy or combined Modestly lowers BP High fat meals decrease absorption Older hypertensive medications should be considered 1st (Medical Letter 2007) Alpha Adrenergic Blockers Peripheral sympatholytics Do not produce tachycardia & palpitations Not initial drug of choice Associated with increased risk of MI Alpha Adrenergic Blockers Side effects Marked hypotension especially with first dose Careful in elderly, volume depleted patients, or in patients taking other antihypertensive drugs Start with lowest dose at bedtime Not recommended for patients with CHF regardless of BP status May benefit males with BPH symptoms JNC VII Compelling Indications Compelling Indic. Diuretic BB CHF X Post MI ACEI ARB CCB AlDO ANT X X X X High CAD Risk X X X Diabetes Mellitus X X X Chronic Kidney Disease Recurrent CVA Prevention X X X X X X X X X X Treatment Goal For most patients goal BP is < 140/90 Does a lower target (< 135/85) reduce risk? Cochrane review found lower targets did not change mortality, MI, CVA, CHF, major cardiovascular events or ESRD [Arguedas 2009] In the very old (> age 80) with CAD, a suggestion of increased risk of adverse outcomes with SBP < 140 & DBP < 70 [Denardo 2010] Treatment Goal For diabetics or patients with CKD • ADA/AHA Goal BP is < 130/80 • INVEST trial of diabetics with CAD found tight BP control did not improve CVD outcomes over usual control Was associated with increase in all-cause mortality Emphasis should focus on maintaining SBP between 130 – 139 mm Hg for these patients Question Your 52 y.o. African American female patient with a 6 year history of hypertension comes in for a routine office visit. No symptoms. BP 142/92. No change in therapy. When would you want to see her again for follow-up? a) Two (2) weeks b) One (1) month c) Three (3) months d) Six (6) months Monitoring Treatment No evidence based guidelines address the frequency of monitoring treatment [Keenan 2009] Monitoring at short intervals increases probability of false positives due to within person variability Longer intervals (years) increase probability observed increase is real Monitoring Treatment Chance of detecting a true increase in BP is better if: Abnormal BP is signal for repeat readings at short intervals Using calibrated sphygmomanometer Set times to measure BP in relation to drug therapy Taking mean of several measurements Or perhaps self-monitoring Monitoring Treatment What is the significance of visit-to-visit (V2V) variability, maximum SBP and episodic hypertension? V2V & maximum SBP are strong predictors of stroke, independent of mean SBP (Rothwell 2010) Interindividual variation is reduced with CCB & non-loop diuretics but increased with ACE, ARB and β-blockers Does not yet prove a causal link Telemonitoring & selftitration Using automated BP measurement with information sent to the office, patients on 2 meds without control [McManus 2010] Having patients request additional medicine if their BP remained uncontrolled for two consecutive months resulted in lower SBP difference of 3.7 mm (95% CI 0.8 – 6.6) Combinations of Medications Beyond studies of 2 drug combinations, little data on the efficacy of 3 or more drugs Advice largely empiric and/or anecdotal Triple therapy amlodipine/valsartan/HCTZ (Tribenzor®) better BP control than dual therapy [Calhoun 2009] ASCOT study found ACE & DHPCCB better than B blocker with diuretic In reducing CV mortality In reducing new onset DM In reducing incidence of fatal & nonfatal CVA Combination therapy Maximal dosage of one drug increases risk of side effects Using ½ standard dose resulted in decrease of side effects 81% for CCBs (pedal edema) 80% for thiazides (hypokalemia) 27% for beta blockers (bradycardia/fatigue) 0 % for ACE/ARB (which are not dose related) Combination therapy Therefore, use lower dosages of two drugs [Wald 2009] Combining drugs from 2 classes will get 5 times greater reduction in BP than doubling one drug If appropriate consider fixed dose combinations May improve compliance May reduce total costs Some Combinations Everything is combined with HCTZ Amlodipine & benazepril (Lotrel®) Slowed nephropathy more than benazepril & HCTZ [Bakris 2010] Amlodipine & an ARB With olmesartan (Azor®) With telmisartan (Twynsta®) With valsartan (Exforge®) Persistence? Do patients continue to take their medication? As many as 25% of patients stop taking their medications by 6 months Many variables influence this rate (side effects, cost, patient’s understanding, physician’s ability to explain, etc.) One new variable is modification of dosage or drug before the end of the 1st prescription – more persistent if adjusted [Tamblyn R 2010] Caution in Elderly What appears as refractory BP control may be sclerotic arteries – ‘pseudo hypertension’ If radial artery palpable when brachial artery is occluded with cuff (Osler maneuver) Measure intra-arterial pressure Hypertension and Elderly Criteria for diagnosis unchanged due to age Treatment reduced incidence CVA, CAD, CHF and death from all causes Treatment initially proven beneficial up to age 80 Treatment after age 80 is now proven beneficial Hypertension and Elderly Aggressiveness of treatment influenced by patient's physiologic age and life expectancy Life expectancy should be at least as long as time required to see a clinically meaningful decrease in: Stroke - 3 years CHF - 4.5 years Heart attack - 7 years Isolated Systolic Hypertension Treatment recommendations: Diuretics Long-acting dihydropyridine CCBs Strong evidence treatment helpful if > 160 mm Evidence less strong for 140 - 159 mm In oldest old males (> 85 yo) higher systolic BP associated with lower mortality Resistant Hypertension BP remains above goal in spite of at least 3 medications at optimal dose Ideally one of which should be a diuretic Patients controlled on 4 or more medications should be considered resistant to treatment Resistant Hypertension Treatment Restrict salt intake Increase dose of diuretic If CrCl is below 30-50 ml/min use loop diuretic Add aldosterone antagonist Since up to 20% - raised aldosterone/renin ratio Consider evaluating for 2o causes Future treatment? Radiofrequency ablation renal sympathetic nerve 23 mm drop in systolic BP in 89% patients Incidental Hypertension Elevated BP found incidentally during visit No consensus on how to evaluate or treat in the acute care setting VA Cooperative Trial (1967) – 143 patients with DBP 115 -130 No adverse outcomes vs placebo initial 3 mo Close follow-up and perhaps treatment is all that is required Incidental Hypertension Prospective randomized trial of 64 asymptomatic patients with DBP 116 -139 Oral clonidine load vs placebo then maintenance oral clonidine No clinical difference in BP at 7 days No evidence demonstrating improved morbidity or mortality with acute treatment of BP in ED Key Points – Lessons from clinical trials BP is the key driver of benefit from medications Drugs that deliver less effective BP control have never produced superior clinical outcomes The choice of initial treatment defines the initial BP response to treatment & the longer term quality of BP control usually requiring fewer add-on drugs Patients with treated hypertension remain at higher risk of CVD Key Points – Lessons from clinical trials If after formal estimate of global risk, their risk of CVD is high, offer statin & ASA therapy Treatment of pre-hypertension with lifestyle changes might prevent development of severe hypertension, target organ damage & diminish risk of dementia What Questions do you have?