Emergency Lecture Series: Sign-out
advertisement

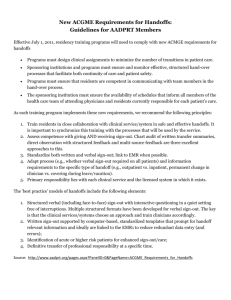
How to conduct an excellent sign-out Leora Horwitz, MD Medicine Boot Camp leora.horwitz@yale.edu Why is sign-out important? • Frequent • Skill set • Potentially dangerous Safety attitude questionnaire • Shift changes are problematic for patients in this hospital • Important patient care information is often lost during shift changes • Problems often occur in the exchange of information across hospital units • Things “fall between the cracks” when transferring patients from one unit to another How are we doing? 2013 Safety Culture Survey, YNHH Medicine, MD/PA/house staff only, N=341 What information is needed? • Name, age, gender, room, family contact info, language, attending, consultants • Code status • Past medical history, allergies, meds, labs • Admission diagnosis • Hospital course • Scheduled events • Clinical condition • To dos, anticipatory guidance Adding value to data Why written and oral sign-out? Why written and oral sign-out? Oral sign-out Written sign-out What’s new What’s new and old Most important info Highlights Complete info Details Interaction, read-back Critical thinking Memory aid Consistent info transfer How should we say it? • Consistently Standardization Sign-out structure S ick? DNR? I D line (name, age, gender, dx) G eneral info re: hospital course N ew events of day, scheduled events O verall health status (clinical condition) U pcoming possibilities + plan & rationale T asks to complete + plan & rationale ? Any questions? How should we say it? • Consistently • Concretely Vague language • “If the nurse calls you with increased sugars, can you start insulin?” • “Over the weekend he was unstable, but not any more.” • “He’s DNR/DNI, but kind of do things if they’re reversible.” Concrete language “And then his blood pressure, if it’s greater than 165/105, you can push 40 of iv labetalol or 10-20 of hydralazine iv. And then he has scheduled labetalol, and that should be given to him unless he’s really hypotensive, like less than 100/60 is what they’ve had.” How should we say it? • Consistently • Concretely • Closed loop Open loop language - “If her Doppler’s positive maybe you could look at the cat scan. I mean it’s not going to be helpful because there’s no contrast. But, she’s going to get that done. Otherwise, it’s not something that you absolutely need to follow up with.” - “OK.” Closing the loop Intern providing sign-out: “Neck CT is ordered, and I guess it got done today. I didn’t see anything in the computer, but the neck CT is to - in the setting of cervical lymphadenopathy and a breast mass, concern for malignancy…” Intern receiving sign-out: “OK. Is the neck CT something that needs follow-up?” Intern providing sign-out: “No, I think it won’t change management tonight.” How should we say it? • • • • Consistently Concretely Closed loop Concisely Concise, but… • This is a 56 year old male who presents with chest pain. • What is this patient’s probability of cardiac disease? Just the facts, ma’am? • This is a 56 year old male smoker with diabetes, hypertension, hyperlipidemia, who presents with several days of chest pain/pressure after walking up 2 flights of stairs, relieved by rest. Concise AND Clinical synthesis • This is a 56 year old male with multiple cardiac risk factors who presents with… Concise AND Clinical synthesis • This is a 56 year old male with multiple cardiac risk factors who presents with several days of classic exertional angina. How should we say it? • • • • • Consistently Concretely Closed loop Concisely, with clinical synthesis Question Is this a good handoff? Lack of interaction Intern providing sign-out: “This woman is a new person with COPD exacerbation. Severe COPD. Not really much going on. The resident ordered ambulatory O2 sat, just to pass on to the tomorrow morning people, just so they know.” Intern receiving sign-out: “OK.” Practice time • Recall our patient: – 64 year old man – Admitted with new non-valvular atrial fibrillation – HTN, DM2, GI bleed – EF 50%, mildly dilated left atrium – Unsuccessful cardioversion today • What will you say in oral sign-out? • What will you write? Sign-out structure S ick? DNR? I D line (name, age, gender, dx) G eneral info re: hospital course N ew events of day, scheduled events O verall health status (clinical condition) U pcoming possibilities + plan & rationale T asks to complete + plan & rationale ? Any questions? How are we doing? 2013 Safety Culture Survey, YNHH, MD/PA/house staff only, N=1,439 Signs of a bad hand-off Uncertainty • “She’s being heparinized. I think she’s had a heart attack.” • “And then the other thing is, what’s the other thing for him tonight? You know, he’s on antibiotics for a UTI. He’s on Zosyn. Or, zosyn or ceftaz? Or, one of those, for a UTI.” Omissions First sign-out, 4pm • Primary intern to on-call intern; 48 seconds • “[Ms. X]…went and had an EUS today and they found a pancreatic mass. And so they did brushings… They were not able to stent it with ERCP… Something happened during the procedure; they said submucosal contrast or something… They said if she has an increase in pain or spikes a fever, they said low threshold for CT of her belly and calling them. I started her on cipro iv.” Second sign-out, 7pm • On-call intern to night float intern • 12 seconds long – “Ms. X. She’s got obstructive jaundice. She was found to have a mass. They said it wasn’t able to be stented but I think they sent a biopsy. So there’s nothing to do tonight.” Delay “It was a step-down patient. And there was a question about the patient’s low blood pressure, but the patient was not on the sign-out… So it took a phone call to figure out who the patient’s attending was, who the last note was from, and then figure out indeed it’s [my cross-cover] patient, and then go and see the patient.” - Post-call interview Adverse event “I had a patient who I had to send to the unit. She had some unanticipated bronchospasm, and apparently she had been a little bit bronchospastic during the day, and this wasn’t an issue that had really been discussed.” - Post-call interview What it takes for an error to reach a patient Reason, 1990