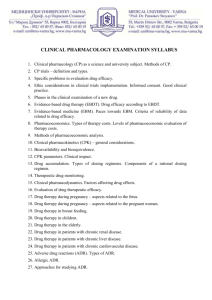
Introduction to Pharmacology
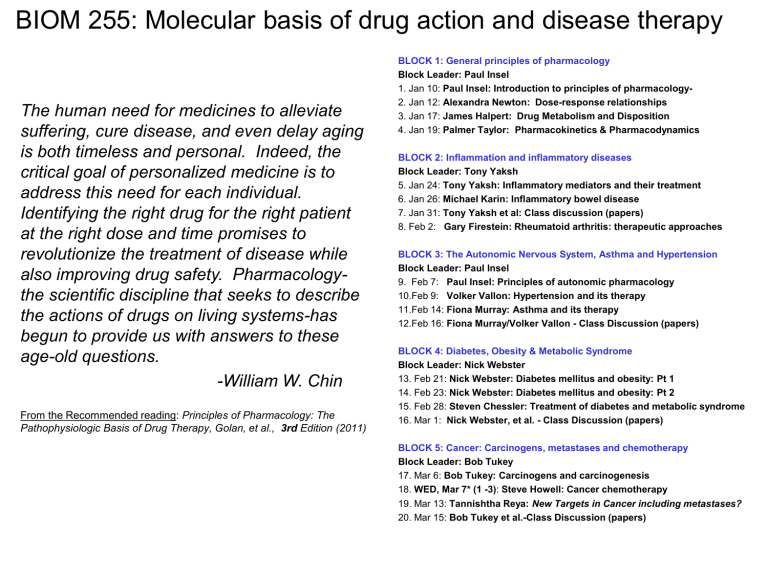
BIOM 255: Molecular basis of drug action and disease therapy
The human need for medicines to alleviate suffering, cure disease, and even delay aging is both timeless and personal. Indeed, the critical goal of personalized medicine is to address this need for each individual.
Identifying the right drug for the right patient at the right dose and time promises to revolutionize the treatment of disease while also improving drug safety. Pharmacologythe scientific discipline that seeks to describe the actions of drugs on living systems-has begun to provide us with answers to these age-old questions.
-William W. Chin
From the Recommended reading: Principles of Pharmacology: The
Pathophysiologic Basis of Drug Therapy, Golan, et al., 3rd Edition (2011)
BLOCK 1: General principles of pharmacology
Block Leader: Paul Insel
1. Jan 10: Paul Insel: Introduction to principles of pharmacology-
2. Jan 12: Alexandra Newton: Dose-response relationships
3. Jan 17: James Halpert: Drug Metabolism and Disposition
4. Jan 19: Palmer Taylor: Pharmacokinetics & Pharmacodynamics
BLOCK 2: Inflammation and inflammatory diseases
Block Leader: Tony Yaksh
5. Jan 24: Tony Yaksh: Inflammatory mediators and their treatment
6. Jan 26: Michael Karin: Inflammatory bowel disease
7. Jan 31: Tony Yaksh et al: Class discussion (papers)
8. Feb 2: Gary Firestein: Rheumatoid arthritis: therapeutic approaches
BLOCK 3: The Autonomic Nervous System, Asthma and Hypertension
Block Leader: Paul Insel
9. Feb 7: Paul Insel: Principles of autonomic pharmacology
10.Feb 9: Volker Vallon: Hypertension and its therapy
11.Feb 14: Fiona Murray: Asthma and its therapy
12.Feb 16: Fiona Murray/Volker Vallon - Class Discussion (papers)
BLOCK 4: Diabetes, Obesity & Metabolic Syndrome
Block Leader: Nick Webster
13. Feb 21: Nick Webster: Diabetes mellitus and obesity: Pt 1
14. Feb 23: Nick Webster: Diabetes mellitus and obesity: Pt 2
15. Feb 28: Steven Chessler: Treatment of diabetes and metabolic syndrome
16. Mar 1: Nick Webster, et al. - Class Discussion (papers)
BLOCK 5: Cancer: Carcinogens, metastases and chemotherapy
Block Leader: Bob Tukey
17. Mar 6: Bob Tukey: Carcinogens and carcinogenesis
18. WED, Mar 7* (1 -3) : Steve Howell: Cancer chemotherapy
19. Mar 13: Tannishtha Reya: New Targets in Cancer including metastases?
20. Mar 15: Bob Tukey et al.-Class Discussion (papers)
Principles of Pharmacology
Paul A. Insel, MD
Tuesday, January 10, 2012
“Poisons in small doses are the best medicines; and useful medicines in too large doses are poisonous”
(William Withering, “discoverer” of digitalis, 1789)
1
Lecture Outline
This lecture will answer the following questions
:
1.
What is pharmacology?
2.
Why are drugs important for human health and scientific research?
3.
How do drug efficacy and toxicity contribute to therapeutic success, therapeutic failures and medical errors ?
4.
What is the “therapeutic partnership”?
5.
What are some major principles of pharmacotherapy?
6.
Where does one obtain reliable information about drugs?
7.
Can drug therapy be individualized/personalized?
8.
What new efforts in pharmacotherapy and pharmacology are on the horizon?
9.
How are drugs developed and approved?
2
What is pharmacology?
• Pharmacology (from pharmakon, the Greek word for drug) is the study of drugs (substances that produce changes in the body) and the characterization of their:
– Structure, targets, and mechanisms of action
– Distribution in and handling by the body
– Effects on the body, including desirable responses ( efficacy ) and undesirable side-effects ( toxicity )
– Drugs include caffeine, nicotine, alcohol in addition to chemicals that are abused (e.g., cannabis, heroin, etc.), food constituents (vitamins, minerals, amino acids, etc.) and cosmetics.
• Pharmacology can be studied at multiple “levels”: molecular,
(sub)cellular, tissue, whole animal, or population
– Clinical pharmacology is the study of drugs in human patients
– Toxicology is the study of harmful rather than therapeutic effects
– Pharmacy involves manufacture, preparation, and dispensing of drugs
3
What is pharmacology?
• Pharmacokinetics (“what the body does to a drug”) and phamacodynamics (“what a drug does to the body”) are the two key aspects of pharmacology
• Prescribing drugs is what MD’s “do” and drugs are the raison d’etre of pharmacists.
• In research, many experimentalists in the biological sciences use drugs to produce or block responses and as a means to infer mechanisms (of cell, tissue/organ, organismal responses).
In addition, others seek new ways to treat disease
Understanding the principles of pharmacology is thus
“central” to the efforts of MD’s, PharmD’s and most biomedical researchers
4
Why are drugs important for health and scientific research?
• From early in human history, pharmacologically active substances (e.g., from plants, animals) have been used to ward off or treat disease
– Drugs can be molecules synthesized in the body (e.g., hormones or neurotransmitters [e.g. dopamine, epinephrine, acetylcholine]) or molecules not synthesized in the body (i.e., xenobiotics , from the Greek xenos , meaning “stranger”)
– Poisons are drugs that almost exclusively have harmful effects
• Discovery and development of drugs (including immunotherapy/ vaccinations) has been a major factor that has increased life span and improved the quality of life
– New scientific insights—in some cases, inferred from novel mechanisms of action – have been essential to this progress, together with controlled clinical trials, in particular, randomized, double-blind trials
– In parallel (especially in recent years) has been the promotion of
“alternative” and “complementary” treatments, many (most) of which have not undergone rigorous scientific validation
5
Why are drugs important for health and scientific research?
• The search for “magic bullets”—agents that treat disease or produce desirable effects but lack harm — and ways to improve such agents has driven scientific discovery for >100 years
– There are very few magic bullets* with high benefits and very low risk
• The challenge is to identify, test, approve and ultimately use drugs that maximize efficacy but minimize toxicity
Primum non nocere: “First do no harm”
• Because of problems (including deaths) that have occurred, governments use approval processes (which tend to emphasize safety>efficacy) before drugs can be marketed and prescribed.
*Examples: selective toxicity of antimicrobials that target bacterial cell walls (lacking in animals/humans) or enzymes found only in micro-organisms
6
Important Terminology
• Pharmacodynamics (“drug action”) includes the measurement of responses to drugs and how such responses relate to drug dose and concentration at a target site
Log Dose
• Pharmacotherapy is the use of drugs to treat disease
– Requires knowledge of drugs, physiology, and pathology (this course will teach you some of each of these but none can be covered in depth)
7
Important “pharmaco” terminology
• Pharmacoepidemiology investigates the effects of drugs on populations
• Pharmacoeconomics examines the cost-effectiveness of drug treatments
• Pharmacogenetics and pharmacogenomics study the influence of genetic variation on pharmacodynamic and pharmacokinetic properties of drugs
8
The Two Key Aspects of Pharmacology:
Pharmacokinetics and Pharmacodynamics
Drug
Pharmacokinetics
Intended target
Unintended targets
Toxicokinetics
Pharmacodynamics
Therapeutic effects
Toxic effects
Toxicodynamics
9
The Two Key Aspects of Pharmacology:
Pharmacokinetics and Pharmacodynamics
Drug administration
Distribution
Effector sites
Pharmacodynamics
Excretion Metabolism
Pharmacokinetics
10
Pharmacokinetics and Pharmacodynamics:
A More Complete Schema
11
Pharmacokinetics and Pharmacodynamics:
A More Complete Schema
Interaction with cellular targets is the focus of most research regarding drug action (“ Molecular pharmacology ”) and includes studies of receptors, receptor signaling, and post-receptor responses
11
How do drug efficacy and toxicity contribute to therapeutic success, therapeutic failures, and medical errors ?
• The major goal is rational therapeutics :
Knowing, understanding, and implementing general principles and specific facts about classes of drugs and individual drugs
• Rational therapeutics seeks to maximize therapeutic responses while minimizing therapeutic failures and medical errors that occur because of “ therapeutic wrongs ”:
Prescribing/dispensing/administering the wrong drug (or wrong dose )
To the wrong patient
At the wrong time
12
What is the “therapeutic partnership”?
• Patients and health providers (e.g., physicians and pharmacists) are partners that seek to optimize drug prescription/dispensing/administration and thereby maximize efficacy and minimize toxicity , thus increasing the
“therapeutic window” (between beneficial and toxic effects).
• Adherence (compliance) to drug regimens is a major problem in therapeutics: many patients do not take the correct drug/dose at the correct time/frequency for the correct period of time). Thus, new approaches are needed to solve this problem and will likely include :
• Simplification of medication regimens
• Patient/caregiver education
• Ongoing assessment of adherence and outcomes
• Novel formulations, delivery methods, monitoring/assessment
13
Therapeutic Window
[Drug] in Blood and Relation to Effects
Oertel, W. et al. Neurology 2007;69:S4-S9
Note the need to achieve effective concentration (efficacy) without exceeding levels that increase side effects (toxicity)
14
Therapeutic Window:
Relationship between Rx and Tx Doses
Rx effect Tx effect Rx effect Tx effect
Log Dose
Rx effect
Log Dose
Log Dose
Tx effect
Rx effect = Therapeutic effect
Tx effect = Toxic effect
15
What are some major principles of pharmacotherapy?
• Use of scientific method and application of fundamental principles must guide drug prescription/administration and the monitoring/evaluation of drug administration
Each patient’s prescription is a scientific experiment (but is not usually thought of in this way):
Hypothesis drug treatment assessment of outcome interpretation ?make changes for next experiment
• Since there are few “magic bullets”, it is critically important for those who prescribe, dispense and administer drugs to be knowledgeable and those who discover drugs must seek to optimize efficacy and minimize toxicity
16
Can one achieve selectivity in pharmacotherapy?
• Drugs are “selective” (rarely “specific”) in their sites of action
• Selectivity depends on several factors
• Chemical nature of drug
• Dose and route of administration
• Patient characteristics (e.g., genetics, age, gender, co-existing disease)
• Selective toxicity for drugs used as chemotherapeutic
(antimicrobial, anticancer) agents or pesticides (e.g.,insecticides) that kill targets without harming the host
• Difficult to achieve selective toxicity if the “target” resembles the host
•
Risk-benefit ratio describes adverse vs. beneficial effects of a drug; acceptable risk/benefit ratios depend on:
• Severity of the disease being treated (or prevented)
• Economic and societal factors: many new drugs are VERY expensive and raise concerns about “rationed care” that will only be available for the world’s most wealthy citizens: is this “moral”?
17
A worldwide problem of overuse of drugs: Antibiotic usage can enhance microbial resistance and ultimately, lead to failure of treatment
18
Where does one obtain reliable information about drugs?
• Textbooks of pharmacology (but most have “dated” info even at time of publication): Recommended text is this course provides a good overview on topics that will be covered
• Journals and especially from on-line sources that provide regular updates
– Clinical Pharmacology (Online Clinical Library @ BML)
– Micromedex (Online Clinical Library @ BML)
– The Medical Letter (E-Journals @ BML)
• Physician’s Desk Reference (PDR)
– Drug company-generated compilation of FDA-approved package inserts + pictures of drugs
19
Drug Names/Classifications
• Drugs have many names: chemical, generic (scientific, officially approved), and commercial (trade, brand)
– Brand names differ in different countries and with different products
– Scientists (and physicians) should use generic and not trade names
• Generic names are those in national pharmacopeias
– Pharmacopeias originally were books for medical materials ( materia medica ) with information about sources, extraction methods, assays but now usually contain info about pure drugs
• Increased harmonization in choosing generic names and in using common endings for certain drug classes
– -olol for β-blockers, -caine for local anesthetics, -clovir for antiviral
(herpes) drugs, -prils for ACE inhibitors, etc
20
Drug Names/Classifications
• Efforts are underway (by the World Health Organization
[WHO] and IUPHAR [Intl Union of Pharmacology]) for new, worldwide systems for classifying drugs
– Many classification systems are possible (e.g., based on therapeutic indication, site of action, mechanism of action, or chemical class)
– Diseases are being reclassified based on genetic/molecular
“signatures”; this information may lead to the reclassification of based on their targets and effects and these “signatures”
• Current pharmacologic classification emphasizes the site and nature of action (e.g., agonist/antagonist), the molecular target (receptor, channel, enzyme), and mode of interaction (e.g., reversible/irreversible; competitive/non-competitive)
21
Can drug therapy be individualized/personalized?
• Much current interest in the individualization of drug therapy and taking into account genetic and environmental factors
– There has been some success but progress toward individualized therapy has been slow —especially as related to drug action
• Many key questions remain, including:
– Are the most important inter-individual differences in pharmacokinetics or pharmacodynamics?
– Will knowing a person’s genome improve the choice among and dosing of drugs?
– Will/should clinical trials be “genomically stratified” such that drugs are tested and then approved for genomic sub-populations? Should basic research studies emphasize such issues during drug development?
Bottom line : This is a work in progress that will likely drive research and changes in drug approval and prescribing
22
What new efforts in pharmacotherapy and pharmacology are on the horizon?
• In addition to “genetically informed” understanding of disease, drug development/prescribing, other aspects of pharmacotherapy that will likely change are:
– ”New” disease/drug targets based on evolving information from genetic, biochemical, molecular biological, and imaging studies [as will be discussed in this course]
– New formulations with an increased number of “biological drugs” (e.g., antibodies, binding proteins, ?antisense, ?siRNA, ?gene therapy)
– Alternative methods of drug delivery (less pain and other side effects, better/more consistent delivery and bioavailability)
– Less-invasive but increased assessment of efficacy and toxicity
– Better methods and their wider use to assess compliance/adherence
– Efforts to create errorless drug prescribing/administration—these are a major source of medical errors, which in spite of much publicity are still seen as a serious, unsolved problem
23
To Err Is Human: Building a Safer Health System
Linda T. Kohn, Janet M. Corrigan, and Molla S.
Donaldson, Editors; Committee on Quality of Health
Care in America, Institute of Medicine (IOM)
National Academy Press
April 2000
Anywhere from 44,000 to 98,000 deaths/yr are caused by medical errors … ~10% from drugs
The IOM Roundtable on Quality of Care categorized threats to quality in 3 broad families: overuse (receiving treatment of no value), underuse (failing to receive needed treatment), and misuse (errors and defects in treatment). In its narrowest form, a focus on safety addresses only the third family , that is, a subset of the whole domain of quality of care.
How are drugs developed and approved?
Answer
: Following discovery of new chemical entities (NCEs) in academia or industry, studies are conducted in animals and humans. Randomized, placebocontrolled , double-blind clinical trials are the gold standard for demonstration of efficacy and determining benefit/harm..
Accumulated evidence suggests that the placebo effect is a genuine psychobiological event attributable to the overall therapeutic context. This psychosocial context can consist of individual patient and clinician factors, and the interaction between the patient, clinician, and treatment environment …The placebo intervention is designed to simulate a therapeutic context such that the effect of the intervention
( placebo effect ) is attributable to the way in which this context affects the patient's brain, body, and behavior. When an active treatment is given, the overall response is the result of the treatment itself and the context in which it is given. (Finniss DG,
Kaptchukb TJ, Miller F, Benedetti F. Biological, clinical, and ethical advances of placebo effects Lancet 375: 686-695 [2010]).
Drug discovery and approval:
Preclinical research and Phases 1-4
J.Molzon.The common technical document: the changing face of the New
Drug Application. Nature Reviews: Drug Discovery . 2:71-4 (2003)
Drug discovery, development and approval: the industry perspective
Preclinical and clinical drug development: Phases and success (with an optimistic timeline and success rate)
IND= Investigational New Drug; NDA: New Drug Application
Preclinical and clinical drug development:
Another view (and longer timeline)
Are drug approvals by the FDA slowing down?
Wall Street Journal: 12/31/10
Drug Approvals Slipped in 2010
Some Potential Blockbusters Suffered Delays Amid FDA's Tougher Safety Stance
The Food and Drug Administration approved about 21 drugs in 2010, a relatively modest figure that shows the pharmaceutical industry hasn't yet escaped its drought in recent years. A few potential blockbusters won approval during the year, but some of the most highly anticipated new products got delayed into next year or beyond. That partly reflects a tougher environment at the FDA, with regulators stepping up their scrutiny of safety issues in drugs for obesity, diabetes and other conditions.
According to monthly drug-approval reports on the FDA's website, 21 new drugs were approved in 2010, down from 25 in 2009 and 24 in 2008, but higher from a recent low of 18 in 2007.
Remember: Drugs are developed to treat people-- not cells or experimental animals!!
Patient (public) advocacy can influence drug approval:
Drugs for HIV and certain other diseases (e.g. especially infections) can be “fast-tracked” and given “priority review”