New Drugs for Old Disorders
advertisement

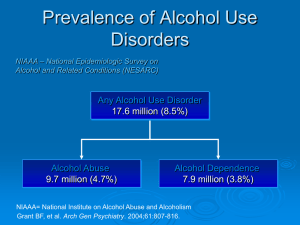
New Drugs for Old Disorders Psychiatric Disorders, Addiction and Meds 12 October 2010 Peter Banys, MD, MSc Director, Substance Abuse Programs, VA Medical Center, San Francisco Health Sciences Clinical Professor of Psychiatry, UCSF Past-President, California Society of Addiction Medicine Department of Veterans Affairs ffairs Lifetime Prevalence of Disorders Epidemiological Catchment Area Study (1990) Mental Disorder 22.5% 3.1% Alcohol Disorder 13.5% 1.7% 1.5% 1.1% Other Drug Disorder 6.1% Regier DA, et al. JAMA 264(19):2511-2518, 1990. Comorbidity for Persons with Mental Disorders Mental Disorders Substance Dependence Odds Ratio Antisocial Personality Disorder 83.6% 29.6 Schizophrenia 47.0% 4.6 Affective (Mood) Disorders 32.0% 2.6 Anxiety Disorders 14.6% 1.7 Comorbidity for Persons with Substance Abuse Disorders Any Mental Anxiety Affective Disorder Antisocial Personality Alcohol Disorders 36.6% 19.4% 13.4% 14.3% Drug Disorders 53.1% 28.3% 26.4% 17.8% Cocaine 76.1% 33.3% 34.7% 42.7% Opiates 65.2% 31.6% 30.8% 36.7% The Chicken or the Egg? Is addiction caused by an underlying psychiatric disorder? Self-medication hypothesis Mental illness impairs good judgment Addiction mimics common psychiatric disorders. Each disorder is independent but worsens the other. Self-Medication Hypothesis I’m not eating, I’m self-medicating.” CoMorbid Disorders in Addiction Psychotic Disorders Depressive Disorders Character Disorders Violence Suicide Schizophrenia NOT “split personality” Main Characteristics Positive Symptoms Early onset (teens to twenties) Debilitating life course Impaired social interactions Hallucinations, Paranoia, Delusions Disorganized speech & behaviors Negative Symptoms Flat affect, lack of presence, poor capacity for humor Little insight Delusional Disorders Unusually stable over time Types Erotomania Grandiose, Messianic Jealous Persecutory Somatic Psychoses from Addiction Alcohol Hallucinosis Alcoholic Paranoia Delirium Tremens Stimulants Post-Stimulant Paranoia Auditory Hallucinations Opiates Detox Psychoses (rare) Psychosis: Differential Diagnosis of Hallucinations Condition Age of Onset Clear Temporal Sensorium Relation to Drinking Autonomic Dysfunction Alcohol Withdrawal >30 No After Yes Alcoholic Hallucinosis >30 Yes Intoxication No Early Withdrawal Yes Unrelated No Schizophrenia <20 Yes Bipolar Disorder Highs and lows may actually co-exist as well as alternate Grandiosity, poor judgment Superficial insight Poor listening skills Post Traumatic Stress Disorder Two Types Hyperaroused, over-reactive Walled-off, numb Extreme level of trauma, or very sustained Disturbed sleep, nightmares, flashbacks Depression Clinical Treatment Problems Medication or therapy? How soon? What if they relapse? Treatment Principles Relationship of Alcohol Use and Affective Disorders Alcohol produces depressive symptoms in anyone Serious, temporary depression may follow alcohol or drug use Drinking can escalate during primary affective episodes, such as mania Depressive symptoms and alcohol problems can occur in a variety of psychiatric disorders Depression & Drinking In alcoholism, DSM criteria for depression can be produced … by chronic use and by withdrawal effects Delay medication trials for 2-4 weeks into abstinence if possible Be aware of increased suicide rates Treatment Principles: Depression in an Addict 2-4 Week Drug-Free Interval Conduct Systematic Medication Trials One drug at a time Change from one class to another Avoid dangerous O.D. drugs Complete Full Therapeutic Trial Adequate Doses Adequate Time Period (up to 12 weeks) ALCOHOL Alcohol’s Effects on Neurotransmitter Systems Gilpin & Koob, Neurobiology of Alcohol Dependence, Alcohol Research & Health, Vol. 31, No. 3, 2008 Medications for Alcoholism: Disulfiram (Antabuse®) ALDH blockers Calcium Carbimide Naltrexone (ReVia®) May also have efficacy for reducing cocaine use Opioid antagonists Nalmefene (ReVex®) Research only Tiapride Dopamine antagonist Research only Acamprosate (Campral®) Glutamate stabilization GABA effects Reduction of protracted withdrawal ? Ondansetron (Zofran®) Serotonin-3-receptor antagonist May be effective in an early onset, severe subset of alcoholic population Dopamine inhibition Reward Reduction [not approved] Topiramate (Topamax®) [not approved] Glutamate Reduction of protracted Medications for Relapse Prevention Mechanism Medication Comments Alcohol Agonist Benzodiazepines are cross-reactive but ineffective as maintenance therapies Alcohol Antagonist Roche has developed an experimental partial antagonist, but it does not block all alcohol effects, especially not lethal dose Acetaldehyde Metabolism Blocker Disulfiram (Antabuse) Calcium Carbimide Metronidazole (Flagyl) Deterrent medication. Disulfiram is no longer used in aversive challenges. Opioid Antagonist Naltrexone (ReVia) Relapse prevention Craving reduction? Acamprosate (Campral) Relapse prevention Serotonin SRI’s Late-onset alcoholics may be less genetically loaded. 5-HT3 Antagonist Ondansetron Early-onset (biological) alcoholics. 5-HT3 may be comodulator of dopamine function (via opioid system). Reduces mesocorticolimbic dopamine release. GABA Glutamate Topiramate (Topamax) Reduces heavy drinking, Promotes abstinence Alcohol Relapse-Prevention Disulfiram (Antabuse®) Naltrexone (ReVia®, Trexan®) 50 mg qd, Half-dose for 3-4 days at start. Liver Function Tests This med blockades ALL opiates, even morphine. Acamprosate (Campral®) 250 mg qd. Liver Function Tests, EKG 666 mg TID Recent US approval Ondansetron (Zofran®) Research Status Mary E. McCaul, Pharmacotherapy Strategies for Alcoholism Treatment, Symposium: New Developments in the Pharmacological Treatment of Alcoholism, 2003. Naltrexone Studies Naltrexone Study Additional Therapy Slowed Relapse Drinking Reduction Craving Reduction + + + + + + + + + + + + + + + + Older Studies Volpicelli et al. 1992 Intensive multimodality O’Malley et al. 1992 Supportive / Coping Skills Volpicelli et al. 1997 Relapse prevention Treatment completers Anton et al. 1999 Cognitive-behavioral More Recent Studies Chick et al. 2000 Compliant patients only Morris et al. 2001 Guardia et al. 2002 Krystal et al. 2001 TSF Twelve Step Facilitation Acamprosate in Europe In 14 of 15 European clinical trials with more than 3,000 patients, acamprosate increased abstinence rates by about 50% Approved for use in the U.S. Somewhat weak results in U.S. COMBINE trial. Acamprosate Studies Therapy Duration Abstinence Increase Craving Reduction Paille et al. 1995 12 + Lhuintre et al. 1990 03 + + Sass et al. 1996 11 Whitworth et al. 1996 12 Acamprosate Study Geerlings et al. 1997 + + + Mary E. McCaul, Pharmacotherapy Strategies for Alcoholism Treatment, Symposium: New Developments in the Pharmacological Treatment of Alcoholism, 2003. Acamprosate Topiramate (Topamax®) Inhibition of mesocortical dopamine release via facilitation of GABA activity Inhibition of glutamate function Hypotheses: Decrease mesocorticolimbic dopamine activity after alcohol intake Antagonize chronic changes induced by alcohol in the glutamate system Oral Topiramate for Treatment of Alcohol Dependence Bankole Johnson et al. (2003) Abstinence-Initiation trial N=150, Double-blind randomized trial comparing topiramate to placebo, 12 weeks Topiramate (up to 300 mg per day) Outcomes 2.9 fewer drinks per day 3.1 fewer drinks per drinking day 27.6% fewer drinking days 26.2% more abstinent days Reduced craving Johnson et al., Lancet, May 17, 2003, Vol. 361, No. 9370, pp. 1666-67 & 1677- Topiramate Other Targets for Medication Catecholamines (Dopamine, NE) Voltage-sensitive calcium channels Corticotropinreleasing factor (CRF) antagonists Ciraulo, Update on Treatment Approaches for Alcohol Dependence, ASAM Med-Sci Conf., April 23, 2004. Serotonin Receptor Subtype and Alcohol Abuse Serotonin’s Role in Alcohol Effects, in Alcohol Research & Health, Volume 21, Number 2, p. 114, 1997 Evidence Report/Technology Assessment: Jan. 1999 Agency for Health Care Policy and Research Disulfiram (Antabuse) A substantial literature has been generated on the use of disulfiram in alcoholism, but the number of controlled clinical trials is limited. Controlled clinical trials of disulfiram reveal mixed findings. There is little evidence that disulfiram enhances abstinence, but there is evidence that disulfiram reduces drinking days. When measured, compliance is a strong predictor of outcome. Studies of disulfiram implants are methodologically weak and generally without good evidence of bioavailability. Studies of supervised disulfiram administration are provocative but limited. Pharmacotherapy for Alcohol Dependence. Summary, Evidence Report/Technology Assessment: Number 3, January 1999. Agency for Health Care Policy and Research, Rockville, MD. http://www.ahrq.gov/clinic/epcsums/alcosumm.htm Evidence Report/Technology Assessment: Jan. 1999 Agency for Health Care Policy and Research Naltrexone (ReVia, Trexan) Trials of naltrexone in the treatment of alcoholism are recent and of generally good quality. There is good evidence that naltrexone reduces relapse and number of drinking days in alcohol-dependent subjects. There is some evidence that naltrexone reduces craving and enhances abstinence in alcohol-dependent subjects. There is good evidence that naltrexone has a favorable harms profile. Acamprosate (Campral) There is good evidence that acamprosate enhances abstinence and reduces drinking days in alcohol-dependent subjects. There is minimal evidence on the effects of acamprosate on craving or rates of severe relapse in alcohol-dependent subjects. There is good evidence that acamprosate is reasonably well tolerated and without serious harms. Evidence Report/Technology Assessment: Jan. 1999 Agency for Health Care Policy and Research Serotonergic Agents There are several controlled clinical trials of serotonergic agents in primary alcoholics without comorbid mood or anxiety disorders. There is minimal evidence on the efficacy of serotonergic agents for treatment of the core symptoms of alcohol dependence. There is some evidence on the efficacy of serotonergic agents for the treatment of alcohol-dependent symptoms in patients with comorbid mood or anxiety disorders, although the data are limited. Lithium There are limited studies on the effects of lithium in primary alcoholics without comorbid mood disorders. There is evidence that lithium is not efficacious in the treatment of the core symptoms of alcohol dependence. There is minimal evidence for efficacy of lithium for the treatment of alcohol-dependent symptoms in patients with comorbid depression. OPIATES Heroin Myths & Facts Opioid withdrawal is dangerous Detox works Symptoms are much like severe flu-syndrome Heroic medical treatments for detox are more dangerous than ‘cold turkey’ (Kleber) The vast majority of heroin detoxes fail, even over 180 days Death rate increases >8X after detox Methadone is just another addiction No “high” Not injectable, Does not impair motor performance (Zacny) 40 Year Natural History of Heroin Addiction 48% The natural history of narcotics addiction among a male sample (N = 581). From: Yih-Ing, et. al., 2001. A 33-Year Follow-up of Narcotics Addicts. Archives of General Psychiatry, 58:503-508) Fig 5.3 Annual Numbers of New Nonmedical Users of Pain Relievers: 1965-2002 Thousands of New Users All Ages Aged 18 or Older Aged Under 18 1965 1970 1975 1980 1985 1990 1995 2000 At Least One Non-Medical Use of Oxycontin During Lifetime 2002 National Survey on Drug Use and Health (NSDUH), SAMHSA, Sept 5, 2003 Why Crush OxyContin ? Pharmaceutical opioids are usually taken orally but may also be injected. They may be crushed to circumvent the mechanisms which control (delay) the release of the active ingredients in long-acting formulations. Triplicate Review Medications for Heroin Addiction Opioid Addiction New production of heroin in South America High purity/potency (smokeable) Detoxification is of limited long-term efficacy Most effective treatment for chronic users is Methadone Maintenance Medications Methadone, LAAM Opioid Agonist Therapy Buprenorphine Partial Agonist Therapy Naltrexone Opioid Blockade Opiate Addiction: Medications Detoxification Opioid Substitution Methadone (Agonist) [Illegal on outpatient basis] Buprenorphine (Partial Agonist) [Requires special DEA license] Non-Opioid Symptom Relief Clonidine (Catapres), alpha-2 adrenergic agonist Lofexadine Anti-spasmodic, anti-diarrheals NSAIDS for bone pain and myalgia Sleep meds Naltrexone & Opioid Blockade Extinction Paradigm Craving Reduction Attempts at opiate use produce no “high” Craving is highly situational. It is reduced when heroin cannot work. Naltrexone Dysphoria?? Unclear whether the blockade of endogenous opioids produces dysphoria or a loss of a sense of wellbeing Naltrexone: Efficacy vs. Effectiveness High Efficacy: Limited Effectiveness: An almost perfect, long-acting blocker of opiates Most effective in monitored treatment of medical or other professionals, executives, and individuals on probation Poor compliance in heroin-using population Poor treatment retention Combined Strategies: Contingency management and family therapy Criminal Justice leverage UROD: UltraRapid Opioid Detoxification Under general anesthesia administered opioid antagonist Continue opioid antagonist for several months, refer to outpatient followup Cost $5,000 – $20,000 Few long-term clinical trials, none demonstrate improved results Potential risks are high (medical co-morbidities and post-detox overdose deaths) Clonidine For Opioid Withdrawal Principle: Alpha-2 adrenergic agonist, suppresses activity in locus ceruleus, Decreases most withdrawal symptoms Advantages: partial relief of symptoms Disadvantages: Requires dose titration, orthostatic hypotension, Does not treat insomnia, myalgias or craving Protocol: 0.1-0.2 mg. q 4 hours, up to 1.2 mg/24 hours for 10 to 14 days David Fiellin, M.D. Opiate Addiction: Maintenance Methadone LAAM Dole & Nyswander’s opioid deficiency theory (1964). Daily Dosing, Competitive blocking dose usually > 60 mg qd Every other day dosing or 2-days a week Rare prolongation of QTc interval on EKG Buprenorphine (formulated with or without naloxone) Partial Agonist (high opiate receptor avidity but low innate activity) Daily dosing, 2-32 mg qd Methadone Maintenance Outcomes Gold-Standard for Opioid Treatment One of the most over-proven treatments in the entire psychiatry and drug abuse literature Detoxification methods succeed only < 3% of the time. Medically safe in pregnant women Outcomes Measures Reduction of … Death rates (8-10X reduction) Drug use Criminal activity HIV spread Increase in … Employment Social stability Retention, medication compliance, and monitoring Buprenorphine The New Kid on the Block (but not everybody likes him) Buprenorphine: Affinity & Dissociation High Affinity for Mu Opioid Receptor. Competes with other opioids and blocks their effects Slow Dissociation from Mu Opioid Receptor Prolonged therapeutic effect EFFICACY: 100 Full Agonist (Methadone) 90 80 70 % 60 Efficacy 50 Partial Agonist (Buprenorphine 40 30 20 Antagonist (Naloxone) 10 0 -10 -9 -8 -7 Log Dose of Opioid -6 -5 -4 Buprenorphine Summary Well accepted maintenance therapy Mild withdrawal Decreases opioid use Greater safety Lower diversion potential Opioid Summary: Heroin remains a lethal drug 48%+ Death Rate / 33 years Prescription opiate addiction, especially Oxycodone, has been accelerating since 1995 Opiate withdrawal is uncomfortable (flu-like syndrome) but not dangerous, per se Aggressive medical treatments for withdrawal can have serious, even lethal, consequences. Efficacy and Effectiveness often diverge in treatment of opiate addiction Methadone Maintenance is the Gold Standard for good outcomes Buprenorphine has a better safety profile, and it may be prescribed from MD offices. COCAINE (Meth) Amphetamine Discarded Pseudoephedrine bottles Methamphetamine Laboratory Crystal methamphetamine Stimulant Myths & Facts Cocaine/Methamphetamine self-medicates ADD (Attention Deficit Disorder) Paranoid Psychosis and Anhedonia are transient effects Few anecdotal reports, little research Very long-lasting paranoid thought disorders are seen in an unknown percent of chronic users Incomplete therapeutic responses to either neuroleptic antipsychotics or to antidepressants. “Crack babies” fail to thrive and develop ADD No discrete diagnosis or syndrome Other factors are intermixed (nutrition, smoking, prenatal care, drinking, etc.) Nicotine Nicotine 1968 1971 1976 Medications for Smoking Cessation NRT’s (Nicotine Replacement Therapy) Patches, Gum, Lozenges, Inhaler, Nasal Spray Base = NRT Patches (21-14-07 mg) Rescue = NRT oral products Bupropion (Zyban, Wellbutrin) Varenicline (Chantix) Partial agonist Warning: Possible severe mood changes Lessons from SF VA Smoking Cessation Clinic Don’t insist on a quit date for all. Consider an attrition paradigm for refractory smokers Go Slow … 6-12 months Use rescue meds liberally – but keep a rough count to know when to reduce patch dose Clean nicotine is better than dirty nicotine Some patients will need nicotine maintenance Monthly visits are essential CO (carbon monoxide) metering is fun and helpful Medications Today Alcohol: Disulfiram (Antabuse) Naltrexone (ReVia, Trexan) Acamprosate (Campral) Ondansetron Topiramate (Topamax) Deterrence Reward Blocker ?? NMDA, GABA 5-HT3 Serotonin Opiates: Naloxone (Narcan) Naltrexone (ReVia, Trexan) Methadone, LAAM Buprenorphine (Suboxone, Subutex) Overdose Rx Receptor Blocker Replacement (agonist) Replacement Stimulants: [None to Date] [? Modafinil under study] Nicotine: Nicotine Replacement (gum, patches, lozenge, spray, inhaler) Bupropion (Wellbutrin, Zyban) Replacement Varenicline (Chantix) Partial agonist GABA/Glutamate actions Discussion