Opioid Addiction –
Pathways to Recovery
Objectives
• What does recovery from addiction entail?
• What is “treatment”?
• How can doctors access treatment for
patients? How can doctors help patients?
Conflict of Interest
• Work in a methadone practice, under AFM
• Have had honoraria for speaking about
addiction, methadone use, and suboxone
use
My work…………..
• 20+ years emergency medicine – lots of
addiction
• 2003 – moved to Addiction Unit (detox
unit) and visited many treatment providers
• 2005 – involved with prescription opioid
addiction, aware of deaths and destroyed
lives
Questions
• What is recovery?
• What is treatment?
• How can I interact with patients to move
along a path of improvement?
Recovery
• Recover from addiction
• Recover from a damaged life
Problems – before addiction
•
•
•
•
•
Broken families, foster care, loss
Trauma and abuse secrets
School problems, bullied
Identity – racial, sexual
ADD, depression, anxiety
Problems – after addiction
•
•
•
•
•
•
•
Family estranged
Kids in custody, unplanned pregnancy
Legal charges
Health challenges, suicidality
Debt, lost job, failing school
Housing
Unhealthy friends and partners
Coping Skills
• Family modelling
• Feeling safe and supported as you try new
things – recovering from failure
• Teen years – Using drugs blocks feeling
emotions, learning to cope
Coping Skills of an Addict
•
•
•
•
Alcohol
Marijuana
Pills
Cocaine
• Excitement – risks, sex, crime
• Anger & violence, blame
• Lies and Secrets
Good Assessment
•
•
•
•
Alcohol
Cocaine/crack
Opioids
THC
• Behaviours – gambling, eating disorders,
sex or porn
A Good History
• It’s not about the drugs –
• It’s about the person…..strengths,
supports, goals, problems, medical and
psych diagnoses, children, legal issues…..
Recovery
• At first, they want a “chemical fix” or detox
• Often want to regain control of drug use,
can’t imagine stopping forever – also want
to get work, $, school right away – can’t
believe it takes time
• Blind or resistant to the idea of emotional
and spiritual growth needs
Recovery
Build skills, don’t use pills!!!!!!
Recovery
• Stage 1 – chaos & survival
• Stage 2 – gaining stability
• Stage 3 – living the meaningful and
examined life, giving back
Recovery
• Stage 1 – chaos and survival
•
- housing, food
•
- trustworthy people
•
- income
•
- facing consequences – physical
illness, debt, legal issues, loss of family,
loss of work
• JUST TRYING TO STAY SOBER
Recovery
• Stage 2 - Gaining stability
• -work, housing, money
• -emotional skills
• -parenting, family contacts, healthy
friends
Recovery
• Stage 3 – meaning in life – honesty,
responsibility, gratitude, persistence,
service, spirituality, facing pain and
shame, finding joy, grace & balance
• Maintenance!!!!
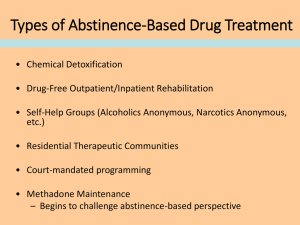
Treatment
• A variety of supports that address body,
mind, spirit
• Medication and/or emotional skills
• Outpatient or residential – or internet
• Professional or self-help
• Religion based or “humanistic”
• Addiction care or psychiatric care
DETOX IS NOT TREATMENT
• The family and addict think detox or taper
will be the quick invisible cure
• Opioid addicts feel more misery and
craving every day of detox – may have
protracted withdrawal for months
• Risk of death
Treatment starts with detox…for
alcohol, cocaine, crystal meth….
BUT – treatment for opioid addiction
starts with assessment, and then
consideration of different treatment options
-attempt at abstinence
-attempt at controlled prescribing
-refer for methadone or suboxone
Treatment Choices
• Methadone/suboxone – for those medically ill,
pregnant, really out of control – reasonable
choice for most
• Abstinence – for those who insist – for those
who still have some supports & stability
• Controlled dispensing/or taper – for select
patients – or for those on waitlist for methadone
Treatment is “longterm”
• Methadone – at least 1-2 years – may be
lifelong
• Abstinence – at least a year of intense
work to stay clean, change life - must keep
up recovery connections, especially with
stress
Narcotics Anonymous &
Alcoholics Anonymous
•
•
•
•
•
•
•
Very valuable
Available to most – free – welcoming
Sober social activity
Active guidance towards sobriety
Sponsor, work the steps
Relieve shame, self-acceptance
Create hope - stories
NA & AA
• Can guide towards honesty, spirituality,
atonement and responsibility, helping
others
• It’s free!
• Know how to get patients to try it……
Verna
• 24 year old health professional
• Early life – parents divorced, rarely saw
dad
• Mom alcoholic
• Good student – episode of depression @
19
• Loved health care work – married,
pregnant – profound depression
• Found stealing morphine at work
•
•
•
•
•
•
•
Immediate losses & intense shame
-job and reputation, licence
-financial stability
-marriage threatened
-all friends were colleagues
-future
-?custody
Outcome
• Starts methadone in hospital – premature
baby delivered, 4 weeks in hospital
• C&FS want to apprehend
• Close follow-up thru methadone clinic –
worry is depression, not addiction
• Never used opioids since Day 1
• Loving mother
Outcome
• Year 1 – coping with motherhood,
marriage, depression, isolation
• Year 2 – struggles with College, does 12
months DBT emotional resilience work
• Year 3 – gets licence with undertaking –
first attempts at work unsuccessful – then
finds work
• Year 4 – second baby, marriage strong, no
depression for 3 years, weans down MMT
Verna used….
• Methadone, encouragement and
supervision at clinic – for years
• DBT = Dialectical Behaviour Therapy –
emotional skills training, cognitive skills,
communication skills
• Work
• Being a mother
Ada -grandmother with pain
• 64 – loved work, friends, garden – chronic
hip arthritis, on high dose dilaudid for 2
years, finally had hip replacement
• Off work for 2 years – marriage
unexpectedly ended – withdrew from
friends – couldn’t garden or tend to house
• After surgery – could not wean off pain
meds – became panicky and distraught
Ada
• Great shame at thought of “addiction” ,
also feels her useful life is over
• Comes to addiction unit for assessment for
help with taper
• Plan – ward admission for 10 day taper
•
- must attend addiction groups as
many of the recovery and emotional
issues are the same
Ada
• Struggles but persists – down to zero –
warned she will have several weeks of
protracted withdrawal with some pain,
sleep problems, lethargy
• Got family involved and reconnected
• One year later – Happy, working PT, active
grandma, tramadol for pain “I never want
to be addicted again”
Ada used…
•
•
•
•
Helpful family doctor
Support with detox
Some information about addiction
A rebuilt social life with meaning
Shawn
• Terrible violent early life – father murdered
mother, siblings sent to orphanages
• Joined army – substitute family life
• Tours of Bosnia and Somalia – PTSD progressive alcoholism and codeine
addiction – two admissions to army
hospital for abstinence fail
• Now employed but in trouble
Shawn
• Empty, alone, shamed, devastated,
hopeless
• In alcohol and opioid withdrawal
• After discussion, wants methadone –
started in hospital setting to treat
withdrawal, get psych opinion, start groups
• Very needy and emotional
Shawn
• Manages to keep job
• Year 1 & 2 – continually distraught – joins
AA
• Does 12 months DBT – some emotional
peace
• Reconnects with his adult children and exwife
• Forced to stop marijuana
Shawn
• Year 5 – weans off methadone
• The future????
Shawn used…..
• Army abstinence programs (failed)
• Ward admission to manage severe alcohol
withdrawal and to start methadone
• Support of methadone clinic for years
• DBT 1 year
• Work – strong contract
• Army – PTSD program
• Family reconnection
Martha
• Comes from “nice part of town” – dad had
cocaine problem for several years, now
very active in recovery groups
• Bright and beautiful, but drifts, drops out of
school, travels to BC with boyfriend, on
and off heroin
• Back in Winnipeg – on IV fentanyl – sees
boyfriend die from accidental OD –
distraught, suicide risk
Martina
• Parents very concerned, involved, scared
• Admitted to hospital – starts methadone –
goes to residential treatment, minimal
participation – sees addiction psychiatrist
• Year 1 – erratic
• Year 2-5 – heavy involvement in N A,
cleans up, slowly rebuilds trust from family,
slowly finds work
Martina
• Slow wean off methadone
• 12 months later - back – tried dilaudid at a
party, habit “took off” – came back quickly
to treatment – on suboxone – will wean off
in next few months
Martina used….
• Methadone clinic and support, counselling
• Extensive use NA – travelled, spoke in
public
• Her own strengths – intelligence, warmth,
humor, work ethic, persistence, selfexamination
• Strong family support
Relapse is the norm
• Their brain will always “love opioids”
• Relapse is a learning opportunity
• Good connections with clinic and NA
usually mean quickly regain stability
Is Methadone Forever?
• Past history – most patients had 10-20
years of heroin addiction, medical illness,
had lost friends and family, crime to
survive – most were not successful at
coming off methadone and being clean
• Young prescription opioid addicts with
good supports – 46% clean, 2 years after
weaning off – Ontario study
Manny
• Using opioids and crystal meth IV for 15
years – schizophrenic, refuses psych
meds – on and off various methadone
programs – no interest in AA
• Sticks with our program for 4 years
• Year 1 – no major change
• Year 2 – no major change
• Year 3 – cleans up for 2 weeks to go to
wedding
Manny
• Year 4 – gets Hep C, arranges own
followup and treatment – cuts back on
crystal meth, rarely misses methadone
doses, grooming better
• Year 5 – moves back to parents – only
using opioids about once a month, doing
social activities, looks normal, has holiday
to BC
• Future????
Manny used….
• Tried several clinics til he found one he felt
he could work with
• “harm reduction” approach
• Social chance – a wedding
• Family reconnection
• Longterm program
• Program didn’t give up
Carly and Bobby
• Both ran away from severely abusive
home, poor education, survived with street
skills – two children
• Abuse of benzo’s, crack, alcohol – then
tried oxycontin, severe addiction, no
money, lost housing, gave kids to friends,
sought treatment – no spots – kids in
C&FS care
Carly and Bobby
• Finally on methadone
• Year 1 – stopped all crack, benzo’s,
opioids – both did residential treatment as
C&FS required it
• Year 2 – Bobby in drug court – started high
school course, good marks
• Year 3 – have baby with disability – with
supervision, allowed to take her home
Carly and Bobby
• Bobby finished Grade 12 – both help look
after daughter
• Both wean down from methadone 160 mg
to 80 mg. Only drug use is THC
• In prolonged battle to get other kids back
with no end in sight
They used….
•
•
•
•
•
Methadone program, longterm support
Month of residential treatment
Drug court
Schooling opportunities, “not a dummy”
Their desire to be a family & regain
children..persistence and hope
• Counselling for past trauma
Residential treatment
• If your patient goes to AFM, the option can
be discussed if appropriate
• Sometimes doctors are in trouble
themselves, or need help for spouse or
kids
• Where? What happens? Cost?
Residential Treatment
•
•
•
•
•
A month to “clear your head”, structure
Education about addiction
Groups plus individual sessions
Heavy exposure to AA
Possibly – cognitive and emotional skills,
life balance, trauma recovery, psych
assessment, help with housing & transition
Residential Programs
• Public or subsidized low cost
• Addiction Foundation - 4 weeks
• Behavioural Health Foundation – 6-12
months
• Anchorage @Salv’n Army – 2 months
Residential Programs
• Private – often $20-30,000 a month –
addiction medical staff, psych
assessments, yoga, exercise, meditation,
family week
• Homewood, Donwood, Bellwood, Top of
the World Ranch, The Orchard,
Whispering Pines
Who goes to residential?....
•
•
•
•
•
Court mandated
C&FS mandated
Family mandated
Work mandated
Many of the sickest
• People often have to attend 2 or more
times, and often do better on the second
or third attempt
Vanessa
• Dad died when she was 13
• Stormy teenager – became dancer – very
punk and tough and tattooed
• Used IV cocaine and morphine – on and
off methadone
• Saw me to give methadone 3rd try “I’ll be
off in 3-6 months”
Vanessa
• Severe cellulitis several times, in and out
of hospital – Hep C – mood swings,
desperation – every time she tries to wean
off methadone she reverts to IV cocaine
and morphine abuse & gets sick
• Tries AFM residential, “hates it”
Vanessa
• $15,000 inheritance - blows half on blow –
then “to save my life” searches internet
and goes to small private program in rural
Saskatchewan – “more intense than AFM”.
“really trusted the people”, strong AA
• Episodes of sobriety for 3 months, then 6
months, then 2 years
• Married with baby in small town Manitoba
What Vanessa Used….
• Support of methadone program over time
– finally agreed to bipolar meds
• SELF-ENGAGED – found program, used
her money, used psychologist
• Sask program was life-saving to her –
went back, could phone
• Strong NA++++ - women’s group
• Took cautious time to fall in love
Family Doctors
• Longterm support to someone in difficulty
• Know the system for psych and addiction
referrals
• Don’t be a prescription push-over
Benzo’s and Opioids
• NOT “patient centered care”!
• Physician-led care!
• Use with restraint, only after assessment.
Consider other options. Be able to say
NO.
Structured Opioid Therapy yes or no?
• Impulsive, difficult, intelligent 19 year old
girl comes to ward to try to detox from
opioids – difficult behaviour – walks away
from treatment
• Finds GP who offers her morphine 400
mg/day and wean down – continues to
inject – tries 4 times, always starts street
purchase at 200 mg – still injecting
Two years in…
• GP phones for advice “how can I make the
next attempt at taper more likely to be
successful?”
• “She is a special girl and not suitable for
methadone”
Opioid Rx, awaiting methadone
• Long wait list in city for methadone spots –
many doctors supporting patients with
daily dispensing moderate dose opioid rx
til spot opens
• Davinder sees GP, shows him note he has
seen addiction doctor and is on waitlist –
requests oxycontin 320 mg /day
• Receives it, daily dispensed – sells half
Awaiting treatment…
• Faces legal charges, goes to jail on no
meds – when out goes back to pharmacy
& they resume rx, no questions asked –
sells ¾ of it
• Goes to treatment, off opioids, for 2
months – when he gets out, rx is still
available!!!
• I find out thru a friend and inform GP
If you do structured rx for
addict…….
• Consider addiction consult or assessment
at methadone clinic or AFM
• Have a contract
• Time limited!
• See the patient regularly, urine screens
• Have clear arrangement with pharmacist
Use your leverage
• Insist no cocaine or street opioids or Rx
stops
• Insist on some form of addiction care –
AFM or narcotics anonymous
• Expect manipulation – check with
methadone clinic if “wait list” problematic
Trying a taper with an addict….
•
•
•
•
•
•
OK to try – also OK to refuse
Expect failure and watch for problems
Don’t do it repeatedly
Don’t do it for “snorters” and injectors
Insist on some form of treatment
Send them to a methadone clinic to be
more knowledgeable about options
What dose?
• Ask them the least and most they use in a
day – go low with Rx
• Consider a challenge dose in the office –
they pick up a “lowish” dose, take it in front
of you, wait 2 hours & see how they look
My son…
• “Mom, a few of my friends have found they
can make lots of money going to the
doctor with a pain story and then selling
the pills….”
• Know and practice the Opioid Guidelines
Resources
• Google “methadone clinics in
Manitoba”
• 1. AFM mine clinic – counselling,
programs, but wait list
• 2. CARI – some counselling - 2 locations
• 3. OATS clinics – 3 locations
• 4. mbatc – telehealth – some counselling
Patient access to methadone and
suboxone
• Patient can self –refer to any of the clinics
– some have same-week intake, some
have wait list
• AFM clinic –we enjoy complex patients rapid access for pregnant patients, or
significant medical illness – will assess
patients under 18
Patient access to abstinence
treatment
• AFM assessment – will help with arranging
detox if necessary – can get addiction
physician opinion – can help patient
change to methadone program if
abstinence too difficult
• Patient just phones the AFM intake line
Complex Patient, what to do?
• Opiate Assessment Clinic, Addiction
Unit, Health Sciences Centre – outpatient
assessment, 2 month wait to be seen –
can help arrange further treatment
• Patients with addiction, psych illness,
medical illness, chronic pain – referral
must come from physician
• Fax referral to Talia Weisz 204-787-3996