Slides - Harvard University: Program in Ethics & Health
advertisement

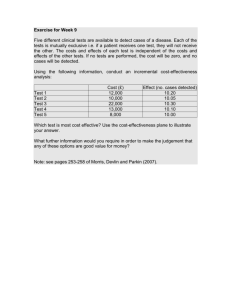
Priority Setting in Universal health coverage: Choosing services Tessa Tan-Torres Edejer Health Systems Financing 1| April 2013 The Three Dimensions (policy choices) Coverage Universal 3| April 2013 Health How does one choose needed services? What types of services to consider: – – – – – preventive, promotive, curative, rehabilitative, palliative Across the life course Across different levels of health facilities procedures and pharmaceuticals and other medical goods positive or negative lists Main criterion: – Cost-effectiveness to maximize health; Getting the most out of the available funding – Quantifying opportunity costs when choosing less cost effective interventions Implementation issues: 5| April 2013 6| April 2013 Millions miss out on needed health services Percentage of births by medically trained persons 0 20 40 60 80 100 Q1, Q5 and Average - 22 0 10 20 30 Q5 Q1 Average Source: Latest available DHS for each country (excl. CIS countries) 7| April 2013 40 50 MDG Tracer Conditions: CEA threshold defined de facto? Antenatal care: 4+ visits Birth attended by skilled health personnel Measles, DTP3, Hib3, HepB3 Children < 5: ARI visit; sleeping under ITN; ORT diarrhoea ART HIV; MCTC HIV + pregnant women TB: case detection rate Additional as possible (based on burden, CEA threshold, budget, logistical feasibility) 8| April 2013 But cost-effectiveness is not that straighforward: Cost-effectiveness might correlate with the other axes. – Many cost-effective interventions are for traditional diseases of the poor – But many cost-ineffective interventions are costly (trauma surgery, cancer drugs, renal replacement therapy) Cost-effectiveness may change: – Because of drop in prices due to national/global volume of sales /international pressure (tiered pricing) – Because of bundling of services (economies of scope); – Start up costs- special problem Even if cost-effective, it may still not be affordable (budget constraints) 9| April 2013 Shifting from pure cost-effectiveness to cost effectiveness ++ « Quantitative analysis for qualitative insight » Begin from CHOICE results (cluster of disease or health sector as a whole) Use checklist to identify excluded interventions of equity or priority setting interest Use quantitative techniques to explore concerns & illustrate impact of alternative choices – What resources will be released or foregone? – What existing treatments will have to be displaced? – What health benefits will be foregone? – What is society willing to pay for a more equitable choice of interventions? 11 | April 2013 11 Example: Mental health (cluster) At a mental health budget level of $3.50 per capita (India), efficiency results from CHOICE suggest funding the following conditions: – Epilepsy – Alcohol treatment – Depression treatment No funding would be allocated to treatment of bipolar disorder or schizophrenia on efficiency grounds alone However, equity & priority-setting considerations (checklist): – Conditions severe, chronic, lifelong – Not curable, limited capacity to benefit – Bad luck in the health lottery – Interventions are the only means to help 12 | April 2013 12 Example: Mental health (cluster) 13 | April 2013 13 Implementation issues There are already pre-existing services being provided by governments of varying cost-effectiveness; e.g SHI providing coverage for hospitalization with a cap; no description of the disease or intervention being covered (subsidy). Administrative ease The patient does not know on consultation what diseases s/he has or what procedure/medication will be needed 15 | April 2013 16 | April 2013 Health expenditures by condition Sri Lanka 2005 Maternal conditions Benign neoplasms Endocrine and metabolic Congenital anomalies Blood/Immune Disorders Female Oral health Neonatal causes Male Mental disorders Nutritional deficiencies Diabetes mellitus Malignant neoplasms Musculoskeletal Genitourinary Nervous system disorders Skin diseases Digestive system Cardiovascular Respiratory infections Chronic respiratory disease Injuries Infectious and parasitic Investigation of signs,symptoms and other contact 0 100 200 300 400 500 600 700 800 Expenditure per capita (Rupees) 17 Fig. 2. Health care choices in a low-income and middle-income country. The vertical axis indicates the level of public subsidy, the right-side horizontal axis refers to the population volume classified as poor and nonpoor, and the left-side horizontal axis represents clinical health services divided into the minimum and the essential packages. Public subsidies should be close to 100% for the minimum package for the poor. In low-income countries the subsidy should fall, perhaps quite sharply, as resources extend to the non-poor or to interventions outside the minimum package. In middle-income countries the subsidy could extend to the non-poor and can finance part of the essential package only if the minimum package is assured for the poor and all cost-effective services are covered for the entire population (WDR93). MIDDLE-INCOME COUNTRY LOW-INCOME COUNTRY Public fiannce share Public fiannce snare S/DALY S/DALY iNCOME 19 | Minimum package April 2013 Poverty line Total population Essential package Income Minimum package Essential package Total population