Pharmacotherapy of Depression
Jerry Overman, Pharm.D., BCPP
Clinical Pharmacy Specialist, Mental Health (NIMH)
NIH Clinical Center Pharmacy Department
WMSHP and DC-CCP Spring Meeting
May 10, 2014
9:00 AM
Jerry Overman, Pharm.D., BCPP
– has no financial interest or relationships to disclose
Objectives
Define major depressive disorder and list the
core symptoms of the illness
Identify the various mechanisms and theories
proposed for the pathogenesis of depression
List the medication classes used to treat
depression
Discuss the pharmacology of the various classes
of antidepressants and how these mechanisms
relate to both efficacy and tolerability
Epidemiology of Depression
Lifetime prevalence of a major depressive
episode: 17%
– Male:
13%
– Female:
21%
Trends
– Age at onset:
Younger
– Incidence:
Increasing
Weissman MM, et al. JAMA. 2011;276:293-299.
Depression and Suicide
Up to 15% of patients with major
depressive disorder requiring
hospitalization commit suicide
Depression Guideline Panel. AHCPR publication 93-0550.
Additional Risk Factors for Suicide
Hopelessness
Male gender
White race
Advanced age
History of attempts
Medical illnesses
Substance abuse
(self or family)
Psychotic symptoms
Living alone
Insomnia
Anxiety
Depression Guideline Panel. AHCPR publication 93-0550.
Suicides/100,000 person-years
Pharmacotherapy Reduces
Risk of Suicide
300
250
259
Treated
Untreated
200
150
141
100
50
0
Isacsson G, et al. J Affect Disord. 1996;41:1-8.
DSM-5 Criteria for
Major Depressive Episode
≥5 symptoms present during same 2–
week period
Change from previous functioning
Functional impairment and/or distress
Symptoms not due to another cause
DSM-5. Washington, DC: American Psychiatric Association. 2013.
DSM-5 Criteria for
Major Depressive Episode
5 Symptoms in the same 2-week period
Sleep:
Insomnia or
hypersomnia
Interest:
Anhedonia - loss of
interest or pleasure
Guilt:
Feelings of
worthlessness
Energy:
Fatigue
Concentration:
Diminished ability
to think or make
decisions
Appetite:
Weight change
Psychomotor:
Psychomotor
retardation or
agitation
Suicide:
Recurrent thoughts
of death
* Must include 1 of these
DSM-5. Washington, DC: American Psychiatric Association. 2013.
Common Presenting Somatic Complaints
“Tired all the time”, “blahs”
Headache, Pain
Malaise
Vague abdominal or joint pains
Disturbed sleep
Sexual or relationship problems
DSM-5. Washington, DC: American Psychiatric Association. 2014.
Psychological Symptoms
Hopelessness
Low self esteem
Denial, discounting, or explaining away
stigmatized feelings
Impaired memory, difficulty concentrating
DSM-5. Washington, DC: American Psychiatric Association. 2013.
Depression Guideline Panel. AHCPR publication 93-0550.
Continuum of Depression and Anxiety
Major
depressive
disorder
Comorbid
depression
and
anxiety
Anxiety
disorders
Outcomes of Treatments of Major
Depressive Disorder
Dropout
Nonresponse/response w/residual symptoms
Response
– Incomplete remission
– Complete remission
Recovery
Acute Recovery in Major Depression
HAM-D score 7
Patient asymptomatic
– No longer meets criteria for depression
– Minimal or no symptoms
Psychosocial and occupational
functioning restored
Rush AJ, et al. Psychiatr Ann. 1995;25:704.
Consequences of Failing to
Achieve Recovery
Greater risk of relapse
Continued psychosocial limitations
Continued impairments at work
Worsens prognosis of other medical
disorders
Increased utilization of medical services
Sustained elevation of suicide and
substance abuse risks
Response and Remission
Remission
Relapse
Increased
severity
Euthymia
Symptoms
Recurrence
Relapse
Response
Syndrome
Treatment Phases
Acute
(6–12 wk)
Time
Kupfer DJ. J Clin Psychiatry. 1991;52(suppl 5):28-34.
Continuation Maintenance
(4–9 mo)
(1 yr)
Economics of Depression—
Total Annual Cost
Lost productivity—55%
Suicide—17%
Outpatient care—6%
Pharmaceuticals—3%
Inpatient care—19%
Profile of the Ideal Antidepressant
Rapid Onset
of Action
Once Daily
Dosing
Activity in a Range
of Disorders
Cost
Effective
Ideal
Antidepressant
Safety in
Overdose
No Drug
Interaction
Minimal
Side Effects
New Mechanisms
Various effects on:
– Serotonin (5HT)
– Dopamine (DA)
– Norepinephrine (NE)
– Gamma amino butyric acid (GABA)
– NMDA Glutamate (N-Methyl-D Aspartate)
Tachykinins
– NK1, NK2, NK3
Corticotropin releasing factor
Glucocorticoid receptor antagonists
Neuropeptide Y
Brain Derived Neurotrophic Factor (BDNF)
Cannabinoid receptors
Ascending Aminergic System
Cortex
Selective manipulation of
these aminergic
transmitters has been the
common denominator for
all currently marketed
antidepressants
These same systems are
implicated
in anxiety
DA
Midbrain
NE
5-HT
Brain Stem
Serotonin
Norepinephrine
Anxiety
Irritability
Energy
Interest
Impulse
Mood, Emotion,
Cognitive function
Sex
Appetite
Aggression
Motivation
Drive
Dopamine
Serotonergic Innervation of the CNS
Thalamus
Cingulum
Neocortex
Cingulate gyrus
Striatum
Hippocampus
Ventral striatum
Hypothalamus
Cerebellar cortex
Amygdaloid body
Olfactory and
entorhinal cortices
Intracerebellar nuclei
Caudal raphe nuclei
Hippocampus
Dorsal raphe nuclei
To spinal cord
From Kaplan HI, Sadok BJ. In: Synopsis of Psychiatry, Behavioral Sciences,
Clinical Psychiatry, 6th ed. Revised. 1991.
Physiologic Distribution of Serotonin
5% CNS:
-regulates cognition, mood,
appetite, sleep, sexual behavior
95% GI tract:
-regulates intestinal movement
-90% cells of the lining of GI tract
-10% enteric neurons
*Also located in platelets to
facilitate aggregation for
blood clotting
Types of Receptors (5-HT1-7)
Receptor
Function
1A, 1B , 1D, 1E, 1F
Anxiety, aggression, sexual behavior, appetite, vasoconstriction
2A, 2B, 2C
2A: inhibits dopamine release; mediates anxiety, agitation, hallucinations,
sexual behavior, weight gain/loss
2B: Smooth muscle (GI tract), cardiovascular function
2C: inhibits dopamine and norepinephrine release; mediates appetite,
anxiety, mood, GI motility, sexual behavior, thermoregulation, weight
gain/loss
3
Chemoreceptor trigger zone, emesis, GI/bowel motility, nausea, memory
4
Cardiac repolarization (seizure susceptibility), respiration, gastric
emptying, oesophageal peristalsis, appetite, anxiety
5A, 5B
Locomotion, anxiety, sleep, cognition, thermoregulation, respiration,
mood, memory
6
7
Norepinephrine Innervation of the CNS
Thalamus
Cingulate gyrus
Cingulum
Neocortex
Hippocampus
Hypothalamus
Pituitary
Amygdala
Cerebellar cortex
Olfactory and
entorhinal cortices
Locus ceruleus
To spinal cord
Hippocampus
Lateral tegmental NA cell system
From Kaplan HI, Sadok BJ. In: Synopsis of Psychiatry, Behavioral Sciences,
Clinical Psychiatry, 6th ed. Revised. 1991.
Neurotransmitters—Mechanisms of Action
Autoreceptor
PRESYNAPTIC CELL
SYNAPTIC CLEFT
Neurotransmitter
Reuptake
transporter
Neurotransmitter receptor
POSTSYNAPTIC CELL
5-HT Receptors
Regulatory Processes
5HT1A
5HT
1D
5HT
5HT1A
synthesis
2A
Sexual dysfunction,
CNS stimulation
5HT
5HT
storage
release
5HT
2C
Weight regulation ?
5HT
5HT1D
5HT
Transporter
5HT3
Might food intake
Regulate vasculature
Headache
Nausea
? anxiety, insomnia,
panic
Pharmacologic Effects of Antidepressants
Reduce depression
Psychomotor activation
Antiparkinsonian effects
Sedation/drowsiness
Hypotension
Weight gain
H1
block
Blurred vision
Dry mouth
Constipation
Sinus tachyardia
Urinary retention
Cognitive dysfunction
ACh block
Alpha2
block
DA
reuptake
inhibition
Antidepressant
Alpha1
block
5HT reuptake
inhibition
Reduce depression
Antianxiety effects
GI disturbances
Sexual dysfunction
NE
reuptake
inhibition
Anxiety
Postural hypotension
Dizziness
Reflex tachycardia
Memory dysfunction
Reduce depression
Tremors
Tachycardia
Erectile/ejaculatory dysfunction
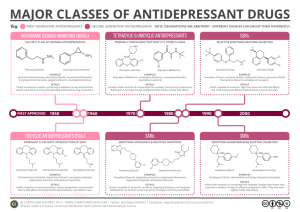
The Evolution of Antidepressants
1950s
MAOIs
1960s
Tricyclics
1970s
Older heterocyclics
1980s
1990s
SSRIs
Newer dual
reuptake inhibitors
Selective dopamine
reuptake inhibitors
Mixed Receptor
Effects
Brief history of MAOI’s
Monoamine oxidase inhibitors first observed to have mood elevating
properties (1950’s)
Limited prescribing
– Acute hypertension reported from ingestion of dietary tyramine “cheese reaction”
– Interactions with other medications
– Introduction of the newer antidepressants
Continued efforts have been made to develop MAOI’s that do not
require restriction of dietary tyramine
– One strategy has been to exploit the existence of multiple
isoenzymes of MAO (MAOA and MAOB)
Monoamine Oxidase Inhibitor Antidepressants
Type
Selectivity
Agent
Brand
Irreversible
Nonselective
Phenelzine
Nardil
Tranylcypromine
Parnate
Isocarboxazid
Marplan
Reversible
MAO-A selective
Clorgyline
MAO-B selective
Selegiline
MAO-B selective
Moclobemide
Brofaramine
Toloxatone
Befloxatone
Eldepryl
Monoamine Oxidase Inhibitors
Drugs
Brand Name
Dosage Range (mg)
Isocarboxazid
Marplan
20-60
Phenelzine
Nardil
45-90
Tranylcypromine
Parnate
20-60
Selegeline patch
Emsam
6-12
The Evolution of Antidepressants
1950s
MAOIs
1960s
Tricyclics
1970s
Older heterocyclics
1980s
1990s
SSRIs
Newer dual
reuptake inhibitors
Selective dopamine
reuptake inhibitors
Mixed Receptor
Effects
Tricyclic Antidepressants
Amitriptyline (Elavil)
Nortriptyline (Pamelor )
Imipramine(Tofranil )
Desipramine (Norpramin )
Clomipramine (Anafranil )
Amoxapine(Asendin )
Doxepin (Sinequan )
Maprotiline (Ludiomil)
Protriptyline (Vivactil)
Trimipramine (Surmontil)
Pharmacologic Effects of TCA’s
Sedation/drowsiness
Hypotension
Weight gain
H1
block
Blurred vision
Dry mouth
Constipation
Sinus tachyardia
Urinary retention
Cognitive dysfunction
ACh block
Antidepressant
Alpha1
block
Postural hypotension
Dizziness
Reflex tachycardia
Memory dysfunction
5HT reuptake
inhibition
Reduce depression
Antianxiety effects
GI disturbances
Sexual dysfunction
NE
reuptake
inhibition
Reduce depression
Tremors
Tachycardia
Erectile/ejaculatory dysfunction
The Evolution of Antidepressants
1950s
MAOIs
1960s
Tricyclics
1970s
Older heterocyclics
1980s
1990s
SSRIs
Newer dual
reuptake inhibitors
Selective dopamine
reuptake inhibitors
Mixed Receptor
Effects
Selective Serotonin
Reuptake Inhibitors
Drugs
Starting
Maximum
Range
Fluoxetine
10 (QAM)
80
20-40
Paroxetine
10 (QHS)
50
20-40
Citalopram
10
40*
20-40
Escitalopram
5
20
10-20
Fluvoxamine
50
300 (BID)
100-300
Sertraline
25
200
50-200
* http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm297624.htm?source=govdelivery
1.) The antidepressant effects of the drugs are known to be limited to the s-isomer
2.) The difference between the effects of citalopram and escitalopram on the QT
interval presumably means that the QT effects are not specific to the s-isomer
http://www.fda.gov/Drugs/DrugSafety/ucm297391.htm
FDA Recommendations re; Citalopram
Not recommended at doses greater than 40mg due to
prolongation of QTc interval
Not recommended for use in patients with congenital long QT
syndrome, bradycardia, hypokalemia, hypomagnesemia,
recent acute MI or uncompensated heart failure
Not recommended in patients who are taking other drugs that
prolong QTc
The max recommended dose is 20mg per day for patients with
hepatic impairment, patients > 60 years of age, patients who
are CYP 2C19 poor metabolizers and patients who are taking
another CYP219 inhibitor; these factors can lead to increased
blood levels of citalopram, increasing the risk of QTc
prolongation and Torsades de Pointes
http://www.fda.gov/Drugs/DrugSafety/ucm297391.htm
The Evolution of Antidepressants
1950s
MAOIs
1960s
Tricyclics
1970s
Older heterocyclics
1980s
1990s
SSRIs
Newer dual
reuptake inhibitors
Selective dopamine
reuptake inhibitors
Mixed Receptor
Effects
Serotonin and Norepinephrine
Reuptake Inhibitors
Drugs
Starting
Maximum
Range
Venlafaxine
(Effexor)
25
375
150-375
BID/TID
Venlafaxine
(Effexor XR)
37.5
225
75-225
QD
Duloxetine
(Cymbalta)
10
60
20-60
QD/BID
Desvenlafaxine
(Pristiq)
50
100
50-100 QD
Levomilnacipran ER
(Fetzima)
20
120
40 – 120 QD
The Evolution of Antidepressants
1950s
MAOIs
1960s
Tricyclics
1970s
Older heterocyclics
1980s
1990s
SSRIs
Newer dual
reuptake inhibitors
Selective dopamine
reuptake inhibitors
Mixed Receptor
Effects
Dopamine and Norepinephrine
Reuptake Inhibitors
Drugs
Starting
Maximum
Range
Bupropion
100mgBID
450mg(3-4
divided)
300-400
150mgQD
200mgBID
300-400
150mgQD
450mgQD
300-400
150mgQD
300mg
For 7-12wks
Wellbutrin
Bupropion
WellbutrinSR
Bupropion
WellbutrinXL
Bupropion
Zyban
The Evolution of Antidepressants
1950s
MAOIs
1960s
Tricyclics
1970s
Older heterocyclics
1980s
1990s
SSRIs
Newer dual
reuptake inhibitors
Selective dopamine
reuptake inhibitors
Mixed Receptor
Effects
Mixed Receptor Effects
SRI, 5HT2 antagonist
– Trazodone (Desyrel, Oleptro)
– Nefazodone
Noradrenergic (alpha 2), 5HT2, 5HT3 antagonist
– Mirtazapine (Remeron)
SRI, 5HT1 partial agonist
– Vilazodone (Viibryd)
SRI, 5HT1a agonist, 5HT1b partial agonist, 5HT3/7 antagonist
– Vortioxetine (Brintellix)
Some Augmentation Strategies
Lithium
Thyroid Supplementation
Atypical Antipsychotics
Buspirone
Modafanil
Lamotrigine
Stimulants
………………………
Discontinuation Syndrome
Withdrawal Syndrome
– Can occur with most antidepressants
– Symptoms: dizziness, nausea, paresthesias,
anxiety/insomnia
– Onset 36-72 hours
– Duration 3-7 days
Summary
Depression is a biologically based illness that responds
to antidepressant therapy in the majority of patients
Appropriate choice of antidepressant therapy should be
based on past response, patient characteristics and
adverse event profile
Appropriate trial length and dosage is important when
evaluating response to antidepressants
Questions?