Centre for Remote Health
A joint centre of Flinders University and Charles Darwin University
CARPA Standard
Treatment Manual
5th edition
Main Changes
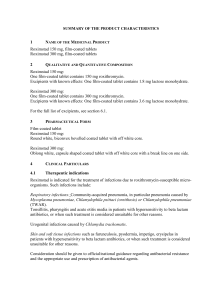
Protocol Format
• Ask - getting the person’s story
• S
• Check - observations, assessments, • O
tests, to help with diagnosis
(includes look, feel, listen, do)
• D
• Do – treatments or interventions
• A
• Follow Up - ongoing care or actions • F
New protocols
• Low blood glucose – Emergency and assessment
• Breathing problems in children – Child health
• Rashes – Child health – includes Measles
• Amphetamines and other stimulants – Mental health and
drug problems
• Interpreting results – Chronic diseases
• Assessing and reducing cardiovascular risk – Chronic
diseases
• Combined checks for chronic diseases – Chronic diseases
• Leprosy – General topics
New protocols 2
• Child growth and development – Child health – replaces Child
growth and malnutrition, includes developmental issues
• Sick babies under 2 months – Child health – replaces Babies
less than 3 months old who are sick
• Messages for healthy food choices, physical activity, size and
weight – Chronic diseases – replaces Healthy choices for food
and activity and Healthy weight for adults
•
Joint problems – General topics – replaces Joint infection
(septic arthritis), includes other swollen, painful joint
presentations
• Joint sprains and strains – General topics – replaces Sports
injuries
• Pain management – General topics – includes Paracetamol
doses and Pain relief
Changed protocols
Moved
• Breathing problems in adults – from Emergency and
assessment to General topics
• Asthma in Adults – from Chronic diseases to General topics
• Chronic lung disease in adults – from Chronic diseases to
General topics
• Adult health check – from General topics to Chronic diseases
• Brief interventions –from General topics to Chronic disease
• Nose bleed – from General topics to Emergency and
assessment
Name change
• Psychiatric emergencies – now Mental health emergency
• Kidney (renal) disease in adults – now Chronic kidney disease
• High fats in the blood (lipids) – now Abnormal blood fats
(lipids)
Removed protocols
• Mental health introduction
• Overview of chronic diseases
• Immunisation/vaccination
• Babies less than 3 months old who are sick – replaced by Sick
babies under 2 months
• Child growth and malnutrition – replaced by Child growth and
development
• Joint infection (septic arthritis) – replaced by Joint problems
• Sports injuries – replaced by Joint sprains and strains
Removed protocols
• Procaine penicillin reactions – combined with Anaphylaxis
• Healthy choices for food and activity – included in Messages
for healthy food choices, physical activity, size and weight
• Healthy weight for adults – included in Messages for healthy
food choices, physical activity, size and weight
• Syphilis – included in Sexually transmitted infections (STIs) in
men
• Chest pain assessment – included in Chest pain
• Pain relief – included in Pain management
• Paracetamol doses – included in Pain management
• Measles – included in Rashes
Emergency and assessment
General changes
• O by non rebreathable mask 10L/min child, 15L/min
adult (was 8L/min with reservoir bag)
2
• O 6L/min children (was 4)
2
• Put in IV cannula (was a drip)
• Normal saline (was Hartmanns, normal saline or
Haemaccel)
• O stats added to observations
2
Emergency and assessment
DR ABC D
• Aligned with Australian Resuscitation Council guidelines
Abdominal pain
• Buscopan removed as treatment for gallstones and diarrhoea
Anaphylaxis
• Use of hydrocortisone and antihistamines removed
Bites – animal and human
• Use clindamycin (was roxithromycin) if allergic to penicillin
Fits
• Glucose (was dextrose) doses changed
• Manage BGL less than 4mmol/L (was less than 2mmol/L)
Emergency and assessment 2
Burns
• Additional criteria to send to hospital – major and minor burns
• Working out children’s fluids
Need maintenance and replacement fluids
Fluid replacement at 4ml (was 3ml) x weight in kgs x % body
surface burnt
• Infected - cephazolin (was roxithromycin) if allergic to
penicillin
Chest pain
• Treatment
Initial – all
STEMI
AMI without ST elevation
• More details on thrombolysis
Emergency and assessment 3
Injuries
• Bleeding – manage shock
• Severe head injury – give flucloxacillin (was ceftriaxone)
• Spinal injury - check for erection (priapism)
• Abdominal injury – do not spring pelvis
• Infected wounds
dicloxacillin OR flucloxacillin AND probenecid (was procaine
penicillin)
Trimethoprim-sulfamethoxazole (was roxithromycin) if allergic to
penicillin
• Old wounds
Amoxicillin-clavulanate (was procaine penicillin) and
Clindamycin if allergic to penicillin (was roxithromycin)
Emergency and assessment 4
Low blood glucose – new protocol
Meningitis
• Added - give dexamethasone IV OR if not available, give
hydrocortisone IV
Near hanging
• Give fluids if low BP (was unless)
Nose bleed
• Details on Merocel pack and balloon catheter now in CPM
Unconscious person
• Section on immediate management added
Child health
Anaemia
• Diagnosis of anaemia – Hb by age
• Prevention of iron deficiency in preterm and small babies
• Information on screening
• Hb measurements in g/L (was g/dL)
• Do FBE if Hb less than 90g/L (was 11g/dL)
• Follow-up – check Hb at 4 then 12 weeks (was 4 then 4)
Chest infection – 2 months to 5 years (was 3 months)
• Fast breathing in children table
• Reliever – 3 doses 20min apart (was 2 doses 15min apart)
• Mild pneumonia - Procaine penicillin or amoxycillin oral for 3
days (was 5 days)
Child health 2
Breathing problems in children – new protocol
• CSLD
3rd line treatment azithromycin (was rozithromycin)
• Asthma
How bad is the asthma – O2 saturation: mild 95-100%, moderate
91-94% (was 94-100% and 90-94%)
Severe asthma – hydrocortisone IM/IV 5mg/kg/dose up to 100mg
– can repeat after 6 hours (was hydrocortisone IM/IV 0.25mg/kg)
Very severe asthma – Put 5mg salbutamol in nebuliser, mix with
normal saline to make 5ml (was put 5ml of undiluted salbutamol
in nebuliser)
Very severe asthma – hydrocortisone IM/IV 5mg/kg/dose up to
100mg (was hydrocortisone IM/IV 0.25mg/kg)
Child health 3
Child growth and development
• Child heath assessments
• Developmental issues
• Fetal alcohol syndrome
Dental and oral problems – 6 months to 5 years – new
protocol
Infant and child growth and nutrition
• Growth faltering
Oral zinc doses by age
Metronidazole oral or tinidazole to treat Giardia, give if there is
diarrhoea
Give vitamin A removed
Child health 4
Diarrhoea
• Persistent diarrhoea
Age categories for zinc doses
Diarrhoea lasting more than 7 days (was 14)
Give vitamin A removed
Ear problems
• Prevention strategies
• Assessing/diagnosing ear problems
• Drowning insects – Use lignocaine 1% or amethocaine 1%
• Hearing tests and results
• Otitis media with effusion – Amoxyicillin for 14 days (was 1014 days)
Child health 5
Ear problems
• AOM with bulge or perforation - Amoxyicillin for 7 days (was
14 days. If still bulge – double amoxyicillin to 50mg/kg/dose
(was think about using45mg/kg)
• Ciprofloxacin 5 drops 2 times a day (was dexamethasoneframycetin-gramicidin 2-4 drops 2-4 times a day)
• CSOM - Ciprofloxacin 5 drops 2 times a day (was
dexamethasone-framycetin-gramicidin 2-4 drops, 2-4 times a
day)
• Softening wax
Sodium bicarbonate solution 4 drops twice a day for 3–4 days
Docusate sodium eardrops (was Waxsol/Coloxyl eardrops)
Rashes – new protocol
Child health 6
Sexual abuse & sexual assault – children & young people
• Requirement to know legislation and protocols around
mandatory reporting
• Presentations of child sexual abuse
• Guideline for suspected sexual assault/abuse/maltreatment of
person under 18yrs
• STIs (includes screening and reporting)
Sick babies under 2 months (was under 3 months)
• Signs of serious sickness can be non specific - be aware of
warning signs – table of warning signs
• Give gentamicin (was think about gentamicin)
• Do U/A removed
Child health 7
Urine problems – 2 months (was 3 months) to 12 years
• Urinary tract infection
Reasons to suspect UTI – and think about balanitis, phimosis or
paraphimosis
Table - collecting urine samples
Amoxycillin-clavulanate for 5 days (was 7 days)
If allergic to penicillin, give trimethoprim-sulfamethoxazole
oral for 5 days (was 7 days)
MCUG for all children under 1 year with confirmed UTI (was child
under 5 years with abnormal renal US)
References to ‘preventer antibiotic’ removed
Child health 8
• Vesico-ureteric reflux
Explanation of VUR – involves urine flowing back up to kidneys
Child with VUR may be on long-term antibiotics
No age for MCUG (was under 5years)
•
Blood or protein in urine
Subclinical cases added
Other cause of blood in urine (haematuria) added
Protein in urine added
•
Problems in boys
New heading
Mental health
Mental health assessment
• Prompts for mental health examination: A-Appearance,
B-Behaviour, C-Conversation, A-Affect, P-Perception,
C-Cognition, I-Insight, R-Rapport
Mental health emergency
• Olanzapine - anti-psychotic of choice
• Do not give benzodiazepines, eg diazepam to child, or person
who is drunk – wait 6–8 hours after last drink
• Give diazepam 5-10 every 2-6 hours max 40mg daily (was 1020mg every 2-6hours max 60mg daily)
• Give risperidone oral 0.5–2mg (was 2mg)
Anxiety
• Panic attacks
Mental health 2
Confusion – delirium and dementia
• Cognitive assessment
Depression
• Depression assessment – Kessler K -10
• Medical review at 6 and 12 months (was 12 months)
• Stopping treatment – reduce by ½ tablet (was ¼-½)
Family and domestic violence
• Signs that child may be exposed or involved
• Checklist for intervention (ABCDEF)
Mental health 3
Grief and loss
• Clinical treatment section
• Sleeping tablets 1–3 nights (was temazepam 10mg 3–4
nights)
Psychosis
• Neuroleptic Malignant Syndrome
• Medicine – see AMH or Medicines Book (was risperidone 2-4mg
oral daily)
Suicide risk
• Suicide risk assessment
• Stay Strong Plan
Drug and alcohol
Alcohol information
• Safe drinking levels (per day) – safe: 0-2 , risky:3-4,
dangerous: more than 4. None if pregnant
Alcohol problems – acute
• Mild withdrawal – taper diazepam dose to nothing over 3-5
days (was 5 days)
• Diazepam oral doses – medical consult before giving more
than 80mg in first 24 hours – 90kg or under, 100mg in first 24
hours – over 90kg (was if you need to give more than 100mg
in a day)
Amphetamines and other stimulants – new protocol
Drug and alcohol 2
Cannabis
• Medicines for cannabis withdrawal
• Follow up
Petrol and solvent sniffing
• Immediate and long term effects
• Olanzapine oral 5-10mg – up to 20mg daily (was diazepam
10-20mg every 2-6 hours)
Sexual health
STIs in men
• Full STI check up table
• If oral or anal gonorrhoea – give ceftriaxone IM 500mg
• Confirmed/secondary syphilis give benzathine penicillin 1.8g
• If pain on passing urine or discharge from penis and outside
local area – Ceftriaxone IM 500mg (was 250mg)
• Herpes - first episode – Valaciclovir 5-10days (was 5 days),
recurrent – Valaciclovir oral 500mg twice a day for 3 days
(was 5 days) OR Famciclovir oral 500mg once then 250mg 12
hourly for 3 doses (was 250gm 3 times a day for 5 days)
• Viral warts – Use podophyllotoxin 0.15% cream (was
podophyllotoxin 0.25% cream or podophyllin)
• Putting on a condom pictures (see CPM)
Chronic diseases
Adult health check
• Age ranges added – older person 55 years (was 50 years)
• Have every 2 years (was every year)
• Older person – check vision, ask about hearing and dental
problems, osteoporosis risks
• Follow up – medical review, dental review, treatment if
cardiovascular risk over 15%
Brief intervention
• Sticking to it
• FRAMES
• Messages for healthy food choices, physical activity,
size and weight
• BMI table and information (see CPM)
Chronic diseases 2
Tobacco information
• Fagerstom test for nicotine dependence
• Details on medicines
• ‘5As’ approach to help people stop smoking
Assessing and reducing cardiovascular risk – new protocol
Combined checks for chronic diseases – new protocol
Chronic diseases 3
Interpreting results
• ACR results
Male 0-2.4, Female 0-3.4 – normal (was 0-3.4)
Male 2.5-34, Female 3.5-34 – Micro-albuminuria (was 3.4-35)
• Waist circumference
• Target levels for blood fats
• HbA1c and non-fasting OGTT for diagnosing diabetes
• Cardiovascular risk levels in relation to BGL results
• Normal BP results - 130/80 or more but less than 140/90 (was
less than 140/90)
Chronic diseases 4
Abnormal blood fats
• 2 yearly checks, annual checks for high risk
• Target level for blood fats
TC – less than 4 (was 4 or less)
HDL-C more than 1 (was 1 or more)
LDL-C less than 2.5 or less than 2 if known vascular disease (was
2.5 or less)
TG – less than 1.5 (was 2 or less)
• Try life style changes for 6-12 weeks before starting medicines
(was 3-6 months)
• Lipid controlling medicines include statins and fibrates
• Check LFTs, CK after 4 weeks on medicine (was check LFTs
after 6 weeks on medicine)
• Combined checks
Chronic diseases 5
Chronic kidney disease
• Glomerular filtration rate replaces calculated kidney function
• Need 2 abnormal ARC at least 3 months apart, or 2 reduced
eGFR to diagnose chronic kidney disease (was If ACR more
than 3.4 repeat within 1 month to confirm kidney disease)
• Action by stage
Stage 1 – ACEi (was not specified)
Stage 2 – ACEi (was ACEi or ARB)
Stage 3 – ACEi and ARB (was not specified)
• Target Hb is 110-130g/L (was 120g/L)
• Do not give metformin
Coronary artery disease
• Medicines for chest pains (angina)
Chronic diseases 6
Diabetes
• Impaired glucose tolerance – think about starting metformin
• Gestational diabetes
• Adjusting insulin dose for low blood glucose readings
• Metformin maximum dose 3g (was 1g)
• Think about starting insulin if 2 or more HbA1c results of more
than 7% (was 9%) or BGLs always more than 8-10mmol/L
(was 10 mmol/L)
• Foot examination details (see CPM)
Heart failure
• Chronic heart failure treatment significantly revised
Chronic diseases 7
High BP
• Routine check every 2 years (was 1 year)
• Management by absolute cardiovascular risk
• May take 4 weeks to see full response to medicine change
(was 3-4 weeks)
General topics
Bone infection
• If delay in sending to hospital – give cephazolin (was
flucloxacillin )
Chest infection – over 5 years and adults
• Looking for signs of chronic problem
• Mild/moderate pneumonia – doxycycline
• Severe pneumonia – ceftriaxone (was benzyl penicillin or
procaine penicillin)
• Sinusitis and bronchitis separated
Bronchitis – antibiotics no longer recommended
Sinusitis – doxycycline
General topics 2
Chronic lung disease
• Questions flagging obstructive sleep apnoea
• Comparison of chronic lung diseases
• Progression of medicines for COPD
• Separation of management of COPD and bronchiectasis
Asthma in adults
• Doses of inhaled corticosteroids
• Puffer and spacer use (see CPM)
Chickenpox and shingles
• Doses for antivirals removed
General topics 3
Coral and sea cuts
• Cellulitis
Treatment time frame – 5-7 days
If penicillin allergy – Clindamycin
• Pustule
Treatment time frame – 10 days
If penicillin allergy – Roxithromycin
• Moderate/severe
Send swab for MC&S
Follow up – repeat cephtriaxone and send to hospital if not
getting better
• Doxycycline – over 8 years (was over 10 years)
General topics 4
Dental and oral problems
• Oral health messages
• Severe infection – clindamycin if penicillin allergy
• Broken tooth
• Pain and significant swelling
Amoxycillin (was phonoxymethyl penicillin and probenecid)
If penicillin allergy clindamycin (was roxithomycin)
• Broken jaw – Amoxycillin (was procaine penicillin)
Heat illness
• Heat cramps
• Features of heat exhaustion and heat stroke
General topics 5
Eye problems
• Antibiotic eye ointment 4 times a day (was 2 times a day)
• Penetrating eye injury – give cephtriaxone (was give
cephtriaxone and gentamicin). If ceftriaxone not available give
cephazolin
• Conjungtivitis
Treatment for bacterial and viral separated
• Gonococcal conjunctivitis
Think of in babies under 6 weeks (was under 4 weeks)
Ceftriaxone (was procaine penicillin or amoxycillin with
probenecid)
Babies under 2 weeks send to hospital urgently (was under 1
month)
General topics 6
• Cellulitis
Orbital cellulitis – Check for relative afferent pupil defect
Periorbital cellulitis – Severe infection give ceftriaxone or
flucloxacillin and send to hospital
Orbital cellulitis – Give flucloxacillin (was only if signs of infection)
If stye, blocked tear duct or wound (was procaine penicillin until
better AND docloxacillin or flucloxacillin if abscess/sty, impetigo,
infected cut)
• Trachoma
Azithromycin for young children (was erythromycin)
Anti-glaucoma drops as advised by eye doctor (was timolol and
pilocarpine)
General topics 7
Hepatitis
• When to refer to a specialist – non-viral hepatitis infection
• Management of chronic hepatitis B and C
• Cirrhosis
• Tests for viral hepatitis infection
• Classification of hepatitis B status
Joint problems – new protocol
Joint sprains and strains – new protocol
Leprosy – new protocol
Meliodosis
• Give ceftriaxone and gentamicin (was ceftriaxone only)
General topics 8
Pain management
• Combines Pain relief, Chronic pain and Paracetamol doses
•
Acute pain
Visual pain scale
Paracetamol-codiene – do not use for children under 7 years
Do not use NXAIDs – Kidney function/eGFR less than 60 or
unknown or high cardiovascular risk
Dosing regimen for opioid injections changed
Naloxone given every 2 minutes (was 3 minutes)
Ibuprofen not used for moderate pain
IM Naloxone not used
Metoclopramide not used for children
• Chronic pain
Managing chronic pain
General topics 9
Painful scrotum
• Infected testes can be due to mumps virus
• Table Assessing a painful scrotum combines Ask and Check
tables
• Suspected UTI – Give cephalexin or amoxicillinclavulanate (was ceftriaxone or ciprofloxacin)
• Review at day 3 (was review next day, if getting better review
again at day 3)
General topics 10
Palliative care
• Expanded description including advanced care plan
• Working out pain medicine doses
• Other treatments
• Managing care (was Treating symptoms)
• Pain management (was giving medicines)
Rectal bleeding
• Ask about family history of bowel cancer
• Do abdominal examination
General topics 11
Skin conditions
• School sores
If injection not possible give amoxycillin oral
Follow-up
Clean sores with soap and water (was providone-iodine)
If there are clearly infected sores (was If more than 6 infected
sores or sores look severe)
If allergic to penicillin give trimethoprim-sulphamethoxazole
(was roxithromycin)
• Scabies
Leave crotamiton cream on babies under 2 months for 24 hours
Follow-up
For children 2 months and over and adults repeat treatment in 1
week ( was (was repeat after 2 weeks if moderate to severe, or
still itchy)
General topics 12
• Crusted scabies
Descriptions of mild moderate and severs crusted scabies
Give ivermectin if over 5 years. Best with full cream milk or food
(was Give ivermectin on empty stomach)
• Boils, carbuncles, abscesses
Keep boils covered with a dressing, was and change every day
until healed to prevent cross-infection to other parts of body. Most
important preventive measure
If allergic to penicillin give clindamycin
Ask family to wash all clothes and bedding in hot soapy water
while on antibiotics, encourage regular hand washing
Follow-up
BGL (was if person keeps getting boils)
Swab for MC&S if severe or several boils (was if person keeps
getting boils)
Give dicloxacillin or flucloxacillin for 5 days (was 5-7 days)
General topics 13
• Head lice
Treat with permethrin 1% shampoo if causing problems (was
treat with permethrin 1% shampoo)
Advice for avoiding head lice removed
• Cellulitis
If not improving after 2 days – medical review, treat as severe
cellulitis
If allergic to penicillin give clindamycin (was cephalexin)
Severe cellulitis – give cephazolin 3-5days (was give
dicloxacillin or flucloxacillin IV every 6 hours)
• Cold sores
Make sure they get enough fluids – may need IV fluids if severe
Medical consult if severe or recurrent – may need antiviral
treatment
Dab with povidone-iodine, if first day removed
General topics 14
• Molluscum contagiosum
May need antibiotics if it gets infected removed
• Tinea
Tinea of the scalp
Collecting samples for tinea diagnosis
Nails – Give terbafine continuously for 4 weeks OR 1 cycle (14
days) = 7days with treatment, 7 days without treatment : For
fingernails 4 treatment cycles, for toenails 8 treatment cycles
(was daily for 6 weeks for fingernails and 12-16 weeks for
toenails)
Tinea versicolor – Put ketaconazole 2% shampoo on affected skin,
leave on overnight (was selenium sulphide 2.5% shampoo on
affected skin. Leave for 60 minutes)
For small areas on skin – Terbinafine cream
For large areas of skin – Griseofulvin tablets
General topics 15
Sore throat
• Warning about difficulty of using oral antibiotics for full 10
days
• If allergic to penicillin give roxithromycin
Tetanus immunisation
• Giving tetanus immunisation
• Giving tetanus immunoglobin
• Follow-up
• Think about when treating a wound – injury, bite, lost tooth,
burn (was wound or burn)
• Indications for tetanus immunisation
General topics 16
Tuberculosis
• Think of tuberculosis if CSLD or bronchiectasis
• Treatment is usually given 3 times a week (was daily or 2-3
times a week)
Urine problems
• UTIs
Treatment – Give trimethoprim or nitrofurantoin or
amoxycillin-clavulanate (was cephalexin or amoxycillinclavulanate)
Female resistant – Treat as advised on pathology result for 7 days
(was 5-7 days, might need norfloxacin)
Female recurrent – Medical review (was treat as advised on
pathology result for 5-7 days, may need longer course)
Complicated UTIs – medical review (was give cephalexin or
amoxycillin-clavulanate or nitrofurantoin)
General topics 17
• Kidney infection
Follow-up mild kidney infection – review at 3 days, if not getting
better medical consult, EUC and refer for renal US
Mild kidney infection – Give cephalexin or amoxycillin-clavulanate for
10 days (was single dose gentamycin and cephalexin for 14 days)
• Blood in urine
Can be caused by cancer
Feel (palpate) abdomen and flanks/loins
General topics 18
Worms
• More information on individual worms
• Dwarf tapeworm
• Strongyloides – can cause growth faltering, low potassium
especially in young child
• Faeces testing – include strongyloides culture
• Test for strongyloides if on corticosteroids for at least 2 weeks
(was course of less than 1 week not likely to lead to
strongyloides)
• Community deworming – 6 months – 16 years give
albendazole single dose twice a year (was 6months – 5 years
albendazole single dose 3 times a year, 5- 16 years twice a
year)
Reference Section
• Reference Table
Normal values, fluid and oxygen rates
• Antibiotics doses table
• Abbreviations
• Contact Numbers
• Index detailed