Isovaleric aciduria Dr Lee Shing Yan Robert
advertisement

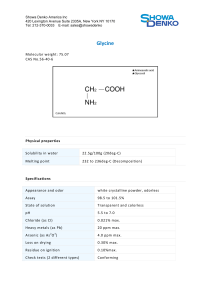
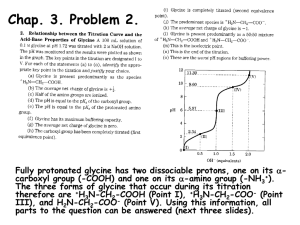
Isovaleric aciduria Dr Lee Shing Yan Robert, Pricness Margaret Hospital, Presentation in HKSIEM, 2011 Birth and perinatal history • 38+3 weeks. First born. Birth weight 3.35kg. Normal vaginal delivery in Kwong Wah Hospital. Discharged on Day 3. • Non-consanguineous marriage • On mixed feed, but poor feeding, baby was drowsy all along, took 1 hour to finish one feed, no cyanosis. Signs and symptoms Presentation • Day 9 • Lethargy • Respiratory distress with pneumonia • Smelly feet • Convulsion the next day Treament • Intubated • Sepsis work-up • Start of antibiotics Initial investigations • CRP 300 (Day 9)→69→33 (on day 19) • WBC : 3.2 → 1.1x 109 /Litre; Neutrophil: 1.1 → 0.1 HB : 16.8 → 12.1 g/dl Platelet :101 → 10 x 109 / Litre • Hypocalcaemia: Total calciium 1.11 mmol/L • Persistent metabolic acidosis pH 7.2. Base excess -11 mmol/L. Anion gap up to 20. Ammonia 214 mmol/L. Glucose 8-9 mmol/L. Differential diagnosis and then diagnosis • Clinical Dx: Metabolic disease and then isovaleric aciduria (day 11 -12) • Chemical diagnosis (day 13) - Urine: ↑isovalerylglycine, 3- and 4-hydroxyisovaleric acid, methylsuccinic acid • Genetic diagnosis on day 20: Father: heterozygous for p.Y371C; Mother: heterozygous for c.1148_1151dupGCTA(p.Y355X) Patient compound heterozygous for the above two mutations Other results back after discharge • • • • • Carnitine, free (umol/L) 8 (12 -46) Carnitine, total 23 (19-59) Acylcarnitine 15 (19-36) Acyl/Free carnitine 1.96 (0.45- 0.83) Raised C4 and C5 –acylcarnitine with other acylcarnitine levels either below or within the reference ranges. Treatment, presumptive dx of kind of metabolic disease day 11 • Intravenous arginine and oral sodium benzoate. multivitamin: thiamine, riboflavin, biotin Response: ammonia 214 84 mmol/L Arginine, Glycine Treatment with clinical diagnosis of Isovaleric aciduria day 12 • Double volume ET done on day 12 and 13 four times in 24 hours • Total parenteral nutrition with protein 0.5 g/kg/day 11th Jan • Carnitine given, dose 400mg/kg/d started on 10th Jan • Glycine not available in Hong Kong PROGRESS after exchange transfusion (ET) • Some spontaneous limb movement noted. • Less stuporous but still drowsy • Ammonia: 82 mmol/L → 118→ 88 (pre-ET on day 12) → 116 (post-ET day 13) →→ 42 (day 16) →50 (day 18). • No more acidosis after ET. pH 7.36-7.42. BE: 8.5 • Persistent neutropenia and thrombocytopenia • On day 17, decided to have haemofiltration scheduled on 16th Jan • On day 18, patient became quite active and conscious and haemofiltration called off Collaboration with other hospitals • Via email to members of HKSIEM, ask for glycine and experience • Dozens of response – negative • Dr Joanie Hui called up the Royal Children Hospital, Melbourne for glycine • Glycine got on board the plane departing at night (day 17) • In the early morning (day 18), glycine at the Customs • Joanie and I went to the Customs at the airport • We declare to the customs as “health food” X-leu available on day 18 • X-Leu analog added to regular milk on Day 18, providing low leucine formula (0.9 g protein 152.3mg Glycine and 53.28g leu/100ml) gradually increased to 2 gram/kg/day of protein and 80 mg leucine/kg/day) Fu in SOPD • Drugs: Glycine 150 – 300 mg/kg/day; L-carnitine 50 – 100 mg/kg/day Double drug during intercurrent illness • Leu restricted to 120 mg/kg/day • Dislikes X-leu after age of 2 years • Some protein aversion at age of 2 years but less so after age of 3 years • Meticulous leucine restriction replaced by low protein diet of 1.5 g/kg/day with X-leu stopped at age of 28 month Leucine content in food Food Leucine content Mature human milk Cow milk Cow and Gate formula Egg Rice, 1 exchange Fruits, 1 exchange Veggie, 1 exchange 99 mg per 100 ml 332 mg per 100 ml 160 mg per 100 ml 533 mg per 50 gram 210 mg 100 mg 90 mg Intercurrent illness • Appearance of sweaty leg odour • So far no increased ammonia, no acidosis or coma • Tx: double dose of glycine and Lcarnitine intravenous D10 forced tube feeding Outcome, CAC assessment at 2 years 3 months • Cognitive: 1 year 9 months • Language receptive: 2 years 3 months; expressive 1 year • Motor: 1 year 9 months Outcome currently, 3 years 6 months • Borderline delay only • Weakest in gross motor. (not yet jumping) Toxin removal • Theoretically: exchange transfusion, peritoneal dialysis, haemolysis • Review articles, textbooks • In the case reports in the literature: peritoneal dialysis and exchange transfusion were reportedly done in two patients • Emails to experts: Carlo Dionisi-Vici and Jean Mari Saudubray Expert advice on toxin removal • Dear colleague, the indication for starting CVVHD is the persistence of severe metabolic abnormalities or the lack of clinical response to medical therapy. I have a limited experience with IVA but as far as I remember patients are usulaay easyer to be managed compared to PA and MMAs. My suggestion is trying to keep the child anabolic and use carnitine also at higher dose up to 500 mg/kg. • Kind regards • Carlo Dionisi-Vici Expert advice, toxin removal • Dear Dr. Lee, if there is a too slow neurological recovery you should start with CVVHD • regards • Jean Mari Saudubray Conclusion • Dx: mimics sepsis; blood for ammonia and ABG and anion gap helpful • Tx: availability of L-glycine and L-carnitine • Resort to toxin removal by ET or peritoneal dialysis when response to drugs poor • Relatively easier in management of intercurrent illness compared to other organic aciduria